The Achilles tendon is a large tendon that originates at the junction of the lateral and medial heads of the muscles of the back of the leg - the gastrocnemius and soleus muscles. If the impact is too strong, the tendon is overstretched and is forced to wear out. This leads to inflammation and over time can cause scar tissue to develop. If the Achilles inflammation continues to worsen, the tendon may tear or rupture.
Tendons are made up of connective tissue that attaches muscles to bones. The tendons themselves are very strong and have low extensibility. There is no clear boundary between muscles and tendons. Instead, there is a transition area - the tendon-muscular zone, where muscle fibers and tendons merge into a single whole. Only at the very end of this zone do the ligaments finally turn into white cords connecting the muscles to the bone, and it is this transition point that is the weakest link in this entire system.
Causes of Achilles inflammation
Heavy or tired calf muscles can cause too much stress on the Achilles tendon . This can be caused by improper stretching of the muscle and tendon, increasing running volume too quickly, mechanical injury, or simply overtraining. Excessive training such as mountain interval training or speed work also puts more stress on the Achilles, even more than other types of running training. All of this can cause tendonitis or inflammation of the Achilles .
High drop (the difference of the sneaker between the heel and toe), uncomfortable hard sneakers also create a high risk of inflammation. Achilles tendonitis can also be caused by the individual structure of the foot. For example, some people may have a flat arch, which puts excessive stress on the tendon.
The main complication of tendinitis is Achilles tendinosis . This is a degenerative form of the disease in which changes in the structures of the tendon occur.
Diagnostic methods ↑
The following examination methods are used for diagnosis:
- physical examination;
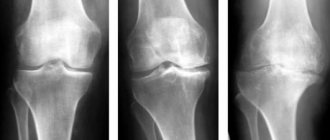
- radiology diagnostics;
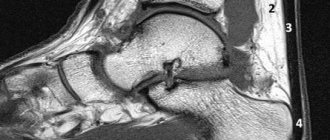
- Magnetic resonance imaging;
- ultrasonography.
Most often, the diagnosis is made based on a conversation with the patient and a physical examination; by palpation, the doctor determines the points of greatest localization of pain.
A characteristic feature of calcaneal tendonitis is that when moving the foot and further palpation, the pain moves slightly, as the tendon and muscles are stretched.
Particular attention is paid to inspecting for ruptures.
X-ray examination can show the presence of inflammation or degenerative changes only if there are areas of calcification.
If there are no calcifications, then radiation diagnostics will not help make a diagnosis.
MRI and ultrasound can determine whether there are ruptures and whether there is a need for surgery.
Prevention and treatment of Achilles tendinitis
If you begin to experience pain in the Achilles area, you should stop running. Inflammation can be relieved locally by applying compresses to the site of pain and affecting the entire body. In the first hours, it makes sense to apply ice and place the inflamed Achilles on a hill (above the heart) to remove swelling, if any.
dimexide perfectly relieves inflammation . It is diluted with water in a ratio of 1:3 (1 tablespoon of dimexide to 3 tablespoons of water), applied to a gauze bandage and applied to the site of inflammation for 2-3 hours. Medical bile will also help relieve swelling at the site of inflammation.
If pain is present, then it is worth making a compress from the following drugs: revalgin, novocaine, dexamethasone .
Locally it is necessary to smear with anti-inflammatory ointment, for example, diklak, nise . The active ingredient - diclofenac - will fight inflammation. Some people advise making a compress of diclofenac and traxevasin at night. Self-massage can also help.
As soon as the inflammation goes away, start stretching your calf muscles. You should not resume jogging until you can move your ankle without pain. On average, it may take 6-8 weeks before you can fully start running or just walking without pain again. It all depends on the severity of the inflammation. If the injury does not respond to self-treatment after a week, see a physical therapist or podiatrist.
Try alternative activities that can give your Achilles a rest, such as swimming and cycling. Stay away from strength exercises that target the site of inflammation.
Forms of the disease ↑
There are 3 forms of achilles tendonitis:
- Peritendinitis is inflammation of the tissues surrounding the tendon. It may be accompanied by tissue degeneration.
- Tendinitis is inflammation and damage to the tendon. The surrounding tissues are not involved in the process.
- Enthesopathy is degeneration and inflammation of the tendon at the site of its attachment to the bone. Sometimes accompanied by the development of heel spurs or calcification.
The beginning of treatment for each of these forms is similar.
Initially, acute pain appears and the tendon is subject to stress.
Without proper treatment, the pain may go away for a while, but then return and become chronic; in the worst case, a complete rupture of the tendon occurs.
How to choose the right running shoes?
To prevent Achilles tendinitis from recurring, strengthen and stretch your calf muscles. An excellent exercise to strengthen the Achilles using rubber bands . When we work the ankle back and forth and left and right, we have resistance in the form of rubber.
The second exercise that will help to simultaneously strengthen and stretch the muscles we need and work on the tendon is calf raise . We stand on a small step with the front of our feet, so that the heels hang down. And we begin slow ascents and descents. You can stay in one position for 10-20 seconds.
Don't forget that properly selected orthopedic shoes with a slight drop between the toe and heel are the ideal solution. During tendonitis, it is best to avoid hill training to avoid over-exerting yourself. And be sure to include rest in your training schedule.
Pharmacological drugs
Non-steroidal anti-inflammatory drugs are the first choice drugs in the treatment of Achilles tendinitis. Most often, orthopedists prescribe Ibuprofen, Diclofenac, Movalis, Nimesulide and Ketorolac. Taking the drugs quickly relieves swelling and inflammation, eliminates pain of any intensity. To enhance the therapeutic effect, ointments and gels are used for local application: Diclak, Voltaren, Fastum, Dolobene, Indomethacin. The duration of the therapeutic course should not exceed 10 days. When prescribing NSAIDs in tablets, proton pump inhibitors (Omez, Omeprazole) are simultaneously used to prevent damage to the gastric mucosa.
If the cause of tendinitis is intense physical activity, doctors often recommend Indovazin. It contains a non-steroidal anti-inflammatory drug and a venoprotector. After applying the gel, microcirculation improves in the affected tissues, promoting rapid tissue regeneration.
To eliminate pain, swelling and inflammation, compresses are used from injection solutions of Novocain, Analgin and the hormonal agent Dexamethasone, mixed in equal volumes. In case of severe pain, these drugs are used to carry out blockades. Parenteral administration of glucocorticoids is also practiced:
- Hydrocortisone;
- Diprospana;
- Prednisolone;
- Methyprednisolone;
- Dexamethasone.
These synthetic analogues of adrenal hormones reduce inflammation and swelling even after a single use. But glucocorticosteroids are used no longer than 3-5 days due to severe side effects. The most dangerous of them is pathological resorption of bone tissue. Hormonal drugs are injected only into the periarticular tissues. When injecting into the Achilles tendon, its integrity may be compromised. Glucocorticosteroids are subject to gradual withdrawal with a reduction in single dosages. If you suddenly stop taking hormonal medications, an exacerbation of tendinitis will quickly follow.
To prevent further degenerative changes in the Achilles tendon, chondroprotectors are included in the therapeutic regimen - Teraflex, Structum, Glucosamine-Maximum, Chondroitin-Acos. Their intake promotes the production of elastin and collagen - fibrillar proteins that form the basis of the connective tissue of the tendon.
| A group of drugs for the treatment of Achilles tendinitis | Names of medicines |
| Nonsteroidal anti-inflammatory drugs | Nimesulide, Meloxicam, Ibuprofen, Diclofenac, Indomethacin |
| Glucocorticosteroids | Prednisolone, Methylprednisolone, Hydrocortisone, Dexamethasone, Diprospan |
| Chondroprotectors | Structum, Dona, Teraflex, Artra, Alflutop |
| B vitamins | Milgamma, Combilipen, Pentovit, Neuromultivit |
| Ointments and gels for local application | Voltaren, Fastum, Ortofen, Diclovit, Dolobene, Artro-Active, Artrosilene |
Acute nonspecific infectious tendovaginitis
This form of tenosynovitis can occur when pyogenic microflora enters the tissue of the Achilles tendon and its vagina.
Most often, the nonspecific form of pathology that is described occurs when an infectious agent penetrates from:
- a purulent focus that is located nearby;
- external environment during injury.
In the first case it could be:
- panaritium of any of the toes;
- purulent arthritis of the ankle or small joints of the foot;
- osteomyelitis - the formation of a purulent focus in the tibia, fibula, and also the bones of the foot with the subsequent formation of a purulent fistulous tract;
- phlegmon of the leg or foot
and so on.
In the second case, infection occurs due to penetrating wounds - punctures, cuts, chopped, lacerations, gunshots, or even deep damage to the skin in this area.
The disease has a classic character - first a serous process develops, then it transforms into a purulent one. In this case, pus accumulates in the cavity of the tendon sheath. Due to swelling and compression of the tendon by purulent exudate, the following symptoms occur:
- pain;
- deterioration of tendon function;
- deterioration of the general condition of the body.
With a serous process, the pain resembles a pain syndrome, as in acute aseptic tendovaginitis of the Achilles tendon. With the development of a purulent process, the picture is as follows:
- pain;
- severe swelling;
- redness of the skin in the tendon area;
- dysfunction of the Achilles tendon.
Characteristics of pain:
- by location - in the tendon area;
- by distribution - they can “shoot” upward in the direction of the shin;
- by nature - sharp twitching or pulsating;
- in severity - strong, intensifying when trying to move the ankle joint. Due to pain, the patient cannot sleep at night;
- by occurrence - they worry from the moment the serous contents form, they increase with suppuration.
Due to the presence of pus, signs of intoxication appear:
- hyperthermia (increase in body temperature) – often up to 38.5-39.0 degrees Celsius;
- weakness;
- brokenness;
- deterioration in work ability.
Regional lymphadenitis is detected - namely inflammation of the popliteal lymph nodes.
note
If pus “spreads” to the synovial bursa, which is located in the area of the Achilles tendon, then tendobursitis may develop.
If the examination for other types of tendovaginitis of the Achilles tendon does not differ in features, then with acute nonspecific infectious tendovaginitis at the stage of suppuration the following is observed:
- the skin in the area of the affected tendon is purple-bluish;
- severe swelling;
- gentle artificial immobilization of the foot.
Treatment depends on what stage the pathology is at.
Therapeutic measures before the formation of an abscess consist of conservative prescriptions - these are:
- immobilization of the foot with a plaster or plastic splint;
- novocaine blockades for severe pain syndrome;
- semi-alcohol lotions;
- physiotherapeutic methods of influence - UHF, laser therapy.
When the pathological process transforms from serous to purulent, surgical treatment is performed - the tendon sheath is opened, washed with antiseptic solutions, and drained. Conservative therapy is also carried out - this is, first of all, the use of antibacterial drugs.
Surgical intervention
Surgical treatment is indicated for the patient if conservative therapy is unsuccessful several months after its initiation. During the operation, the doctor makes an incision in the middle and exposes the tendon. The surrounding altered tissues are excised along with the formed thickenings. In case of extensive destruction, surgical intervention is highly complex:
- to restore functional activity, plantar muscle tendons are placed on the excised areas;
- strong tension of the tissues is prevented by suturing their incisions in the front in a weakened position for better posterior closure.
In patients with enthesopathy, the tendon bursa is excised after a lateral incision. With a Haglund deformity (the presence of a bone ridge), the heel spur puts excess pressure on the area where the tendon attaches to the heel bone. In this case, the patient is indicated for orthopedic surgery with bone dissection under general anesthesia. The process may use surgical instruments, laser or ultrasound. After tissue excision, the bones are fixed in the desired position using various devices: nails, plates, bone graft, plaster cast. Skeletal traction, which involves inserting a steel pin into the bone and suspending a weight, is widely practiced. The bone gradually stretches and takes on an anatomically correct position.
Throughout the entire postoperative period (1-1.5 months), the patient is advised to wear an orthosis or a plaster boot. When moving, he must use crutches so as not to put stress on the operated leg.