Main symptoms
- Short stature. In the absence of treatment, the height of a patient with achondroplasia reaches 120-125 cm;
- Disproportion in the length of arms and legs (short length) in relation to a normally developed torso;
- O-shaped curvature of the hips and legs, looseness (instability of the ligaments) of the knee joints, flexion deformities of the shoulders, contractures (limited movements) of the elbow joints;
- Hydrocephalus, predominance of the “brain skull”, saddle-shaped nose;
- Associated spinal deformities;
Diagnosis of achondroplasia before birth
In 1994, researchers studied the genetics of achondroplasia and identified the gene responsible for the appearance of this disease. This discovery has made it possible to create extremely accurate prenatal tests that can help diagnose or exclude the possibility of developing achondroplasia.
Families wishing to have a child are encouraged to undergo such testing if both parents have this pathology, since in such cases every fourth child inherits one abnormal gene from each parent and as a result receives a form of the disease incompatible with life. After birth, this type of disease is diagnosed during a medical examination and x-ray examination.
What do patients with achondroplasia suffer from?
The main problem is the lack of social adaptation:
- psychological problems associated with non-compliance with growth “standards”;
- lack of adaptation of devices, instruments, switches, public toilets in the Russian Federation;
- difficulties with self-care: short arm length and limited movements in the elbow joints with a normally developed torso do not allow for full personal hygiene and self-care;
Medical (orthopedic) problems:
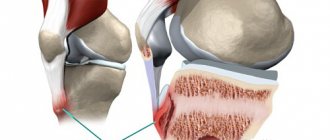
— instability of the ligamentous apparatus of the knee joints, together with deformities of the lower extremities, if left untreated, leads to the early formation of arthrosis of the knee joints, which is accompanied by pain and the need for early joint replacement
Pathogenesis and genetics
Achondroplasia is caused by mutations in the FGFR3 gene, and is located on the fourth chromosome. At the same time, the growth of cartilage is inhibited. FGFR3 encodes a protein called Fibroblast Growth Factor 3. This protein is responsible for the growth of bones in the body. In achondroplasia, FGFR3 cannot function properly, and bone and cartilage growth slows down. This results in short bones, abnormal bone shape, and short stature.
FGFR3 is a transmembrane tyrosine kinase receptor that binds to FGF. The binding of FGF to the extracellular region of FGFR3 activates the intracellular domain of the receptor and triggers a signal sequence. In endochondral bone, FGFR3 activation inhibits chondrocyte proliferation in the growth plate, thereby helping to coordinate chondrocyte growth and differentiation with the growth and differentiation of bone progenitor cells.
Achondroplasia-associated FGFR3 mutations are gain-of-function mutations that cause ligand-independent activation of the FGFR3 protein. This constant upregulation of the FGFR3 protein improperly inhibits the proliferation of chondrocytes in the growth plate and leads to shortening of long bones, as well as abnormal formation of other bones.
Guanine at position 1138 in the FGFR3 gene is one of the most mutable nucleotides identified in all human genes. A mutation of this nucleotide occurs in almost 100% of cases of achondroplasia; more than 80% of patients have a new mutation. New guanine mutations at position 1138 of the FGFR3 gene occur exclusively in paternal germ cells and their frequency increases with paternal age (>35 years).
Goals of surgical treatment
- correction of deformities (alignment of limbs);
- limb lengthening
Surgical treatment options:
- Corrective osteotomies (bone intersection) with immediate correction of deformity (without lengthening) and fixation (using orthopedic implants);
- Deformity correction and limb lengthening using the Ilizarov method. To do this, an osteotomy is performed and a transosseous device is installed. Lengthening is carried out by daily dosed changes in the lengths of the threaded rods between the annular supports of the transosseous apparatus
Lengthening or corrective osteotomies?
From an orthopedic point of view, lengthening (isolated lengthening) for achondroplasia has relative indications and is not mandatory, because does not improve joint function, while correction of deformity can save the patient from arthrosis of the joints and associated pain in the future.
Basically, limb lengthening solves problems of social adaptation and improves self-care capabilities, namely: putting on socks and shoes, the ability to care for hair, personal hygiene, the ability to use switches, sockets, etc., and the ability to buy standard clothes.
Achondroplasia - what is it?
This disease has many names, such as: Parro-Mar disease, daphyseal aplasia, congenital chondrodystrophy. Achondroplasia is a genetic cartilage disease that can be inherited. The main features of chondrodystrophy are dwarfism and disproportionality of the limbs.
History of origin
Archaeological information about people with achondroplasia appeared in Ancient Egypt because... The climate there is hot and mummification was common. Scientists, studying the ancient art of Egypt, found that such people were treated very respectfully and did not consider their deviation as a shortcoming. The Egyptians even praised them as gods. Based on the found cave paintings and images on the tombs, it became clear that the dwarfs worked as dancers, jewelers, artists and held high-ranking positions. People with achondroplasia were so respected that they were buried in a cemetery near the pyramids, and this was considered a great honor. According to some scientists, dwarfism occurs as a result of incest, and in those days this phenomenon was very common.
Symptoms
As mentioned above, a person with achandroplasia has visual differences from a healthy person. Main signs of the disease:
- Slowing down of physical development;
- Short stature (approximately 130 cm);
- Curvature of the legs;
- Underdeveloped shoulder and hip girdles, causing the limbs to become short.
- Kyphosis, curvature of the spine
.
Children have normal mental development, but they encounter difficulties walking independently. There may be difficulty breathing due to compression of the spinal cord, which is a common cause of death. As you get older, you may experience severe pain in the lower back. The hip and shoulder joints become more curved over time; this is genetically determined.
Causes
The cause of chondrodystrophy is a mutation in the FGFR3 gene. This gene is responsible for the function of stimulating the growth of cartilage, bones and joints.
During development, cartilage tissue is influenced by an altered genotype, as a result of which the correct process of bone tissue growth is disrupted. When diagnosed, uneven, modified bones can be detected in a child.
The probability of inheriting the disease is 50%, provided that the parents have such an autoimmune disorder.
The causes of spontaneous gene mutation are the following factors:
- Parent's age. The older you are, the greater the risk of developing achondrodysplasia;
- Father or mother with chondrodystrophy.
Be that as it may, the child’s genetics plays a fundamental role in the development of the disease. If one parent has the disease, the child has a 50% chance of inheriting achondroplasia. If you have two parents, the risk increases and is 70%.
Diagnostics
To diagnose a patient, it is necessary to conduct a general medical examination by a specialist, as well as apply instrumental methods. Special instrumental methods make it possible to study in detail the nature of the pathology and the number of affected areas. Laboratory tests are not needed to make a diagnosis.
During a general examination by a doctor, you need to pay attention to the main signs of the disease, manifested in structural pathologies. Next, the specialist prescribes a certain type of diagnosis:
- X-ray and computed tomography. These methods are based on X-ray radiation. Such radiation makes it possible to examine organs in detail, focusing in various tissues of the body. CT is a more modern method, it uses improved equipment that scans faster than x-rays.
- Magnetic resonance imaging. In this case, the method of studying pathology is based on electromagnetic waves, which provides a safe scan of the body, which reduces the risk of developing cancer.
Treatment
At this time, there are no known cures for achondroplasia. However, medicine can reduce the risks of complications of the ongoing disease.
There are two types of treatment: radical and conservative. Conservative treatment is used if pathology is detected in a newborn. In this situation, there is a chance to influence the growth of cartilage and bone tissue using medications. Drug treatment is used in the form of growth hormones. Cases have been recorded in which this hormonal therapy eliminated structural changes in the musculoskeletal system.
In case of severe skeletal deformation, a radical method is prescribed. It involves surgical interventions:
- An operation aimed at eliminating deformity. First, the bones of the patient’s legs are cut, and then they are fixed in the correct position. This method is called "osteotomy".
- An operation performed on the spine. Patients with achondroplasia experience pain and disturbances in brain activity, which is caused by a narrowing of the spinal canal. There are fatal cases. This operation allows you to reduce the pressure in the patient’s spinal canal by making an incision. This method is called laminectomy.
Prevention
For prevention purposes, potential parents are recommended to undergo testing to identify a genetic predisposition to chondrodystrophy. During the examination, a diagnosis is made for the presence of a mutagenic gene as part of the biological information of the parents. The results of such a study make it possible to warn about possible threats.
The disease cannot be prevented because the child receives genetic material with a mutated gene that causes achondroplasia.
Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Extension options
The issue of lengthening and correction of deformity in a patient with achondroplasia is resolved individually
in every case.
We do not recommend
starting lower limb lengthening before
5 years
. In most cases, from our point of view, it is optimal to start the first “circle” of lengthening at the age of 7-8 years.
In all cases, during the initial examination of the patient, the doctor, together with the parents, develops a primary plan for upcoming surgical interventions, which takes into account the following points:
- the desired amount of height increase depending on the child’s current age and height;
- number of elongation cycles;
- breaks between cycles;
- social employment of the child (school, holidays, etc.);
- the number of segments and the sequence of their lengthening and deformity correction;
brief information
Achondroplasia (also called: diaphyseal aplasia , Parrot-Marie disease , congenital chondrodystrophy ) is a cartilage disease that is one of the main causes of disproportionate dwarfism: affected patients have shorter-than-normal upper and lower limbs and a normal torso.
The causes of achondroplasia are genetic: a mutation in the FGFR3 gene, located on chromosome 4, causes its occurrence.
In addition to the characteristic features of short stature and lack of proportionality between the limbs and trunk, achondroplasia causes other clinical signs including : short toes, valgus of the knees or feet, large head and prominent forehead.
There are currently no specific treatments for achondroplasia . Therefore, achondroplasia is an incurable disease.
How do we lengthen?
We use ring and semi-ring transosseous devices (Ilizarov type). Elimination of deformation (at the end of the lengthening period), in most cases, is carried out using a unit based on computer navigation Ortho-SUV (hexapod).
Sequence of cycles.
In most cases, depending on the proportions of the hips and legs, the patient undergoes the following algorithm:
- 1st cycle – parallel lengthening and correction of deformities of both legs;
- Cycle 2 – cross lengthening and correction of femur-tibia deformities;
- Cycle 3 – cross lengthening and correction of femur-tibia deformities (opposite).
The cycle ranges from 6 months to 1 year. Between cycles - a break of at least 1 year. Between the first and second cycles of lengthening the lower limbs - lengthening of the shoulders. Repeated lengthening of the shoulders (if necessary) after the 3rd cycle of lengthening the lower limbs.
In some cases, the algorithm may include 4 cycles:
- 1st cycle – parallel lengthening and correction of deformities of both legs;
- Cycle 2 – parallel lengthening and correction of deformities of both hips;
- Cycle 3 – parallel lengthening and correction of deformities of both legs;
- Cycle 4 – parallel lengthening and correction of deformities of both legs.
Standard Treatments
There is currently no way to prevent or treat achondroplasia, as most cases involve new, unexpected mutations. Treatment with growth hormone does not significantly affect the height of a person with achondroplasia. In some very specialized cases, leg lengthening surgery may be considered.
Detecting bone abnormalities, especially in the back, is important to prevent difficulty breathing and leg pain or loss of function. Kyphosis (or hunchback) may require surgical correction if it does not go away when the child begins to walk. Surgery may also help leg flexion. Ear infections caused by illness must be treated immediately to avoid hearing loss. Dental problems may need to be addressed by an orthodontist (a dentist with special training in straightening teeth).