Achilles tendon
- one of the main tendons that are responsible for the full movement of a person.
Without it, it is impossible to bend the foot and turn it inward - movements that occur when walking. Given the constant daily stress, the Achilles tendon
is susceptible to injury and inflammation.
They occur especially often (about 6 times more often) in men. Also, people of postmenopausal age are predisposed to diseases and ruptures of the Achilles tendon
.
Is it possible to protect yourself from the problem and what to do if the Achilles tendon hurts
? Read below.
Anatomy of the Achilles tendon
Developed Achilles tendon
present only in humans and is an evolutionary adaptation to upright walking. It is believed that the human musculoskeletal system has not yet had time to fully adapt to upright walking, so its individual elements experience increased loads.
Although evolutionary selection gave the Achilles tendon
high endurance (its tensile strength reaches 400 kg) and has made it the thickest tendon in the human body, it is nevertheless considered one of the most vulnerable.
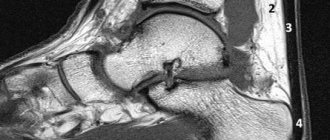
The Achilles tendon from above, in its widest and thinnest part, is attached to the fusion of the heads of the triceps muscle (formed by the gastrocnemius and soleus muscles), and from below, tapering at a level of 3-4 cm above the heel bone, it is attached to the calcaneal tubercle.
Due to its anatomical features, the Achilles tendon
is responsible for normal supination and pronation of the foot (the main biomechanical processes that occur during human movement). It also provides anatomically correct movement and stability in the knee, ankle and subtalar joints.
Mechanical properties of the Achilles tendon
fully correspond to these tasks: when running, it can withstand loads that are 8 times the weight of the person himself.
Subtleties of the disease
This pathological process mainly belongs to the group of occupational diseases of the musculoskeletal system.
Etiological factors can be called:
- Chronic injury to muscle tissue.
- Overstrain of tendons and surrounding tissue, stenotic ligamentitis.
- Repetition of the same type of motor acts with the feet or fingers, with a frequency of 50–60 times per minute. Moreover, the transition between the rhythm, speed and characteristics of the movements performed is carried out at a sharp pace.
Localization of the pathological process:
- The anterior surface of the lower leg. Statistically, it occupies about 10–20% of identified cases.
- The hip is damaged in extremely rare cases.
- Achilles tendon area. Occupies approximately 15%.
Paratenonitis is characterized by a professional nature. Consequently, the risk group consists of workers in the following list of professions:
- Sander and polisher.
- Stenographer, typist, seamstress.
- Pedal specialists.
- Ironer.
- Milkmaids with manual milking.
- Mechanic, turner, carpenter, blacksmith.
Some sources associate such a disease with meteorological factors (increased humidity, elevated temperature in the production workshop), which have a certain impact on the pathological process. However, the development of the pathological process is still influenced by the dynamics of motor acts, and weather conditions act as an aggravating factor.
Symptoms of inflammation and rupture of the Achilles tendon
Timely noticed symptoms of rupture or inflammation in the Achilles tendon
They often help with outpatient treatment - at home, with periodic consultations with a doctor.
And ignoring them can lead to surgery, because constant injury to already deformed collagen fibers can lead to complete rupture of the Achilles tendon. Signs of inflammation in the Achilles tendon
are:
- pain when palpating and stepping in the heel area, which intensifies after physical activity and subsides during rest;
- swelling of the ankle;
- redness and heated skin on the back of the ankle;
- crunching and pain when trying to rotate the foot;
- deterioration of plantar mobility;
- noticeable tendon stiffness, loss of normal stretching ability;
- difficulties when climbing stairs, jumping, rising on toes.
A ruptured Achilles tendon
is accompanied by the following symptoms:
- swelling in the ankle joint with “retraction” at the site of the rupture;
- sharp pain, especially when trying to stand on your heel or toe;
- severe difficulty walking.
Pathogenesis[edit | edit code]
Damage to the Achilles tendon occurs in middle-aged people (40-60 years old) after an unusually long load (walking or running) undertaken without preparation against the background of a predominantly sedentary lifestyle and despite the rigidity of the tendon and decreased mobility of the ankle joint. Damage can be avoided with stretching exercises and gradually increasing loads. In professional athletes, Achilles tendinitis always indicates a violation of the training regimen, incorrect running technique, or overwork.
Main causes of Achilles tendon injury
There are four groups of causes that can cause Achilles tendon rupture or inflammation
. This includes:
- tendon injuries (open and closed);
- inflammatory, metabolic, viral and other diseases that may not directly affect the Achilles (gout, rheumatoid arthritis) or occur in the immediate vicinity of it (heel spur, tendonitis, achilles bursitis);
- congenital problems with the Achilles tendon (its insufficient length from birth and paresis of the foot) or collagen synthesis, constitutional features;
- others (age-related, biochemical, related to patient habits).
Damage and pain in the Achilles tendon
may occur in case of infectious diseases while taking fluoroquinolone antibiotics. Already in the first 48 hours after the start of treatment with them, any high load on it can provoke a rupture of the Achilles tendon.
The tendon can also be damaged due to excess weight, constant wearing of uncomfortable shoes (too tight or high heels). These reasons cause deformation of collagen fibers and reduce their endurance. A sedentary lifestyle increases stress on the Achilles tendon
. This is due to poor development and shortening of the calf muscles - the “companions” of the Achilles in matters of load distribution.
Age-related changes in the body, which begin after 40 years, cause a decrease in the strength and elasticity of the tendons. Increasing physical activity at this age without prior long-term adaptation can cause inflammation and even rupture of the Achilles tendon
. At the same time, the correlation is different for men and women, because The microscopic structure of the tendon is different. The level of estrogen, the female sex hormone that is responsible for the elasticity of ligaments and tendons, also varies. Because men have less of it, their tendons are stiffer and less resistant to jerking loads.
Diseases
The Achilles tendon can hurt
due to the following diseases and pathologies:
- heel spur and Haglund's deformity;
- tendinitis and calcification of the tendon due to micro-tears;
- traumatic lesions of the heel and ankle;
- arthritis, arthrosis and other joint diseases (spine, knee, ankle, foot and toes);
- deformations in the musculoskeletal system (for example, flat feet);
- metabolic diseases (diabetes mellitus, gout) and endocrinological problems (ovarian dysfunction and others);
- systemic and autoimmune diseases that affect connective tissue (rheumatoid arthritis, rheumatism);
- systemic and local infections.
Injuries
Achilles tendon injuries
are accompanied by its partial or complete rupture, or separation of the tendon from the heel tubercle to which it is attached. Most often, the injury occurs at the start of sprinting, when landing in jumpers or dancers, and also during the game of tennis, volleyball, basketball or football. Particularly conducive to obtaining it:
- too rapid increase in load intensity, to which the musculoskeletal system does not have time to adapt;
- lack of normal warm-up and cool-down before playing sports;
- insufficient development of the calf muscles;
- physical overload;
- sudden jerking loads;
- uncomfortable shoes;
- running and jumping on unsuitable surfaces.
At the time of injury, the patient experiences a sensation of a sharp blow to the back of the ankle, which gradually passes, giving way to pain. A characteristic cracking sound may be heard. Traumatic damage to the Achilles tendon is often accompanied by severe hemorrhage and swelling. You can often feel a “groove” in the area of the rupture. The left leg is most often injured.
With a traumatic rupture of the Achilles tendon, the patient cannot voluntarily bend the sole or rise on the toes, and all attempts are accompanied by severe pain.
First aid for Achilles tendon ruptures
consists of applying ice and applying a special splint.
Classification[edit | edit code]
There are three forms of Achilles tendinitis that are closely related and require the same initial treatment.
- Peritendinitis is inflammation of the tissues surrounding the tendon, with or without tendon degeneration.
- Tendinitis is inflammation and degeneration of the tendon without involvement of surrounding tissues.
- Enthesopathy is inflammation and degeneration of the tendon at its insertion with or without calcification and heel spur formation.
Achilles tendon treatment
Conservative treatment of the Achilles tendon
is based on pain relief, relieving swelling and providing rest to the affected tissues.
The etiology of the problem makes its own adjustments to the treatment strategy. For example, if an x-ray reveals calcification of the Achilles tendon
, characteristic of tendonitis, it is recommended to use shock wave therapy, and, if necessary, surgical treatment.
If the Achilles tendon
pain due to injury, local anesthesia (for example, novocaine) and a plaster cast are used. For complete ruptures and avulsions, suturing surgery is always performed.
Medicines
For the treatment of Achilles tendon
There are 2 main groups of drugs used: NSAIDs (non-steroidal anti-inflammatory drugs) and chondroprotectors.
NSAIDs (same as NSAIDs) help relieve symptoms of inflammation and reduce pain and swelling. They are usually prescribed in the form of gels, ointments and compresses, but in case of severe inflammation of the Achilles tendon
, tablets can also be used.
The course of treatment with oral NSAIDs usually lasts 10-12 days. You can use external remedies for inflammation for several weeks or even months (for tendon injuries). If the Achilles tendon hurts
even after taking NSAIDs, with severe tendonitis or inflammation, glucocorticosteroids are prescribed.
The value of chondroprotectors for the treatment of Achilles tendon
lies in their effect on collagen synthesis and the health of joint structures. This group of drugs also has a preventive effect, and therefore is recommended for regular use by people who are at risk for Achilles disease (professional athletes, patients with musculoskeletal diseases). Because the Achilles tendon lacks blood vessels, tissue repair is usually very slow. Taking chondroprotectors helps speed up this process and prevents the appearance of abnormal, unstable collagen fibers.
Chondroprotectors should be taken for at least 2-6 months a year, since they have a cumulative and prolonged effect. A classic example of a chondroprotective drug is Artracam - these sachets with glucosamine should be taken daily for 2-4 months. Artracam not only relieves pain and promotes normal collagen synthesis in the tendon, but also protects other joints and tendons involved in maintaining upright posture.
Fixation
Since the Achilles tendon is extremely sensitive to loads associated with body movement, patients are recommended to wear fixing bands and orthoses. It is also important to provide rest to the sore limb: you should avoid running, jumping, and suddenly stepping on the foot and heel; During everyday activities, such as climbing stairs, the body weight should be compensated by the calf muscles.
Ankle bandages help prevent further injury to the Achilles tendon, relieve swelling and promote normal tissue repair without unwanted scarring. At the first signs of an inflammatory process, it is recommended:
- applying a pressure bandage;
- rest with the ankle joint raised higher than the hip joint (for example, you can place a pillow or sofa cushion under your leg);
- applying ice or an ice compress (for no longer than 20 minutes).
To fix the affected tendon, you can tightly bandage the foot and lower leg with a regular or elastic bandage. It is advisable to consult a doctor before doing this. Practicing traumatologists say that it is extremely rare for patients to be able to apply the bandage correctly the first time and actually fix the muscles, ligaments and tendons in a stable position.
Exercises
For diseases and injuries of the Achilles tendon, therapeutic exercises are allowed only after the inflammatory process has resolved. At the initial stages, gentle stretching of the ankle muscles is performed. Strengthening them allows you to reduce the load on the tendon, and stretching them helps to properly structure the “young” collagen fibers, which were initially twisted like spaghetti.
With painless movements in the ankle joint, incl. when rotating the foot or lifting on the toes, you can move on to the main exercise therapy complex. Physical activity is increased gradually. adding from 5 to 10% per week. If your Achilles tendon hurts
after exercise, the load is reduced. Each therapeutic exercise session should begin with a warm-up (warming up the muscles) and a cool-down (stretching). This helps to avoid re-injury of the tendon and adjacent structures of the musculoskeletal system. The following groups of exercises are used:
- Balancing exercises. They train not only large, but also small muscles that are responsible for maintaining balance and serve to prevent tendon injuries.
- Stretching exercises for the short and long calf muscles.
- Exercises to stretch the muscles of the foot.
- Exercises to strengthen the calf and other muscles.
Therapeutic and preventive gymnastics for injuries and diseases of the Achilles tendon involves all the muscles of the legs, lower back, abdominals - i.e., those parts of the skeletal muscles that are directly responsible for stabilizing the human body and keeping it in an anatomically correct position. Such complex training, carried out every day to maintain tone, can significantly redistribute the load from the Achilles tendon.
During exercise, it is recommended to wear sports shoes that stabilize the ankles and provide good shock absorption of the foot (especially the heel). As an example, the following are effective exercises for restoring and strengthening the tendon.
- Stand upright until you feel a stretch in your ankles, then gently shift your weight to your affected leg. Trying to take the weight off your ankles through your calf muscles, shift your weight to your heel, lifting the front of your foot. Use your healthy leg to return to the starting position. When performing the exercise, noticeable discomfort is possible, which, however, should not turn into acute pain. The exercise is performed in 3 sets of 15 times twice a day. If necessary, you can increase the load with a small backpack.
- Place your heels on a step or other small raised surface so that your toes hang freely from it. Extend your right hand in front of you and place your left hand on your belt. Without losing your balance, slowly squat down and then straighten up. It is recommended to perform 3 sets of 10 exercises daily.
- Stand facing a wall at arm's length (not including your palm). Place one foot on the wall, pressing your heel into the surface with both hands. After a minute, change legs.
- Sit on the floor with your legs straight. Place a rolled towel over the instep of your foot, holding it by the ends. Gently extend your foot away from you, creating moderate resistance using the towel. It is recommended to perform 2 sets of 10 times throughout the day.
- Place a massage roll under your shin. Perform back and forth movements on it, trying to knead the calf muscles, but without touching the sore tendon. The shin can be rotated in different directions to increase the area of the muscles being stretched.
- Sitting on a chair, alternately “write” in the air with the toe of first one foot and then the other (letters, numbers, shapes). 10-15 approaches are recommended at intervals of 20 seconds.
To strengthen the calf muscles, patients may be recommended swimming, water aerobics, and cycling.
Physiotherapy
Physiotherapeutic procedures contribute not only to the elimination of local symptoms and speedy recovery from injuries. They also trigger the formation of healthy collagen fibers in the Achilles tendon (i.e., straightening and strengthening them). If your Achilles tendon hurts
, the following physiotherapeutic techniques are used:
- magnetic therapy;
- shock wave therapy;
- ultrasound therapy with medications (most often these are anti-inflammatory drugs that prevent the formation of unstable and rupture-prone scar tissue in the tendon and its sheaths);
- ozokerite;
- cryotherapy;
- paraffin applications;
- balneotherapy (especially mud therapy);
- therapeutic massage and exercise therapy.
As a rule, the duration of a course of physiotherapy is 10 sessions, but it can be extended as prescribed by the attending physician.
Surgery
Surgical treatment of Achilles tendon is used in cases where the Achilles tendon hurts
, despite complex therapy - i.e., when conservative treatment methods have already been exhausted or a priori cannot resolve the pain syndrome.
Typically, it is indicated for the formation of a bone spur on the back of the heel bone (called Haglund's deformity), severe ruptures, or even complete separation of the Achilles tendon. There are 3 main types of operations used:
- removal of bone growths;
- excision of damaged tissue that cannot be restored;
- stitching the tears with a lavsan or nylon seam.
Also, in case of ruptures, tendon repair may be recommended. Recovery after surgery on the Achilles tendon involves immobilizing the limb (including the knee joint) and wearing a special “boot” made of plaster or other material for 45-60 days. In the absence of contraindications, for a speedy recovery, massage, physiotherapy and exercise therapy are carried out under the supervision of a qualified rehabilitation physician.
Crepitant paratenonitis of the forearm
This is an aseptic, serous-hemorrhagic inflammation of loose connective tissue. It is characterized by four symptoms: pain, swelling, crepitus and decreased hand function. Paratenonitis occurs most often acutely, after unusual, excessively intense or too long work, with strain on the hand (twisting clothes, working with a wrench, levers, etc.). The disease is also observed after influenza, rheumatoid infection, etc.
Symptoms
Pain occurs in the lower third of the forearm, on the dorsal radial side in the area of the intersection of the tendons of the long muscles of the first finger with the tendons of the extensor radialis of the hand. When these muscles are overstrained, often associated with pronation and supination of the forearm, friction occurs between the tendons, causing a characteristic sign - “crepitus” - a sound reminiscent of the crunching of dry snow underfoot. Often it is distinguished by the ear and caught by the patient himself. The disease is characterized by swelling, small hemorrhages and aseptic inflammation in the loose connective tissue surrounding the tendon. The swelling begins from the retinaculum extensorum above the styloid process of the radius, goes obliquely proximal to the middle third of the ulna, but never extends beyond it. The swelling has an elastic consistency, oval-cylindrical shape, is not fused with the underlying tissues, is painful and tenses when the fingers are clenched into a fist.
Diagnostics
It is not difficult to recognize professional crepitant paratenonitis of the forearm in the acute phase, when there are four main symptoms, and in case of prolonged disease it is necessary to differentiate from specific and rheumatoid tendovaginitis, myositis, neuritis of the cutaneous branch of the radial nerve and stenosing ligamentitis of the first dorsal carpal tunnel, from degenerative-dystrophic diseases of the radial nerve. wrist joint. A carefully collected anamnesis, examination of the patient, and radiography almost always help clarify the diagnosis. Occupational crepitating paratenonitis is more often observed in young, untrained workers, and sometimes in craftsmen who have had a break in work or a change in standards, technology and production rhythm.
Treatment
Treatment of professional crepitating paratenonitis of the forearm has been sufficiently developed. In the acute period of the disease, the main and mandatory method is immobilization, ensuring complete rest of the limb.
It is recommended to adhere to the following treatment regimen. Once the diagnosis is established, a novocaine blockade is performed on the forearm in the area of greatest pain, a plaster cast is applied from the distal phalanges to the elbow in the functional position of the fingers, with the first finger abducted and opposed in a fixed position. Two days later, in case of persistent pain, swelling and crepitus, the blockade is repeated, methindol or butadione is prescribed orally - 2-3 times a day. From the 3-4th day heat is applied: heating pad, Sollux, UHF therapy; from the 5th-6th day - short-term active and passive movements in the wrist joint and fingers; on the 6-7th day, the plaster splint is removed and the range of movements not associated with tension increases. On the 8-9th day, when the symptoms of the disease disappear, the patient can be discharged on an occupational sick leave for light work for 3-5 days (depending on the nature of the work) and only after that, if he feels well, he can be allowed to return to his main work. In this case, it is necessary to teach the patient daily hand sanitation, muscle relaxation and compliance with the rhythm of movements and micro-rest. The average duration of disability for acute occupational paratenonitis is 10–20 days. All authors who have studied this disease note a tendency to relapse (16-20%), if the treatment was short-term, the immobilization of the arm was not long enough or was performed incorrectly, and if the patient was immediately discharged to work that required strain on the arm. To prevent recurrence of crepitating paratenonitis, it is recommended that workers wear an elastic cuff on the forearm, which leads to a significant reduction in the incidence of paratenonitis. The treatment regimen for crepitating paratenonitis in the acute phase has not lost its importance, but the general health of the patient should be taken into account, and combination therapy with the use of enzymes and other anti-inflammatory factors should not be abandoned.
Preventive actions
In clinical traumatology, there are a number of recommendations on the prevention of injury leading to paratenonitis:
- In the case of monotonous and stereotypical work activity, it is recommended to use interval pauses between movements performed. You need to rest for 5-10 minutes. The recommended interval between breaks is approximately 50 minutes.
- After a long period of inactivity, the load should increase gradually - over about three to five days.
- Performing industrial gymnastics.
If you belong to a risk group, it is recommended to wear special bandages.
Attention!
The information on the site does not constitute a medical diagnosis or a guide to action and
is intended for informational purposes only.