Cervical spondylosis is a common degenerative disease of the cervical spine. It is believed that the development of spondylosis is associated with age-related changes in the intervertebral discs. Several syndromes are observed clinically. These include: neck and shoulder pain, suboccipital and headache, radicular symptoms and cervical spondylogenic myelopathy. As the disc degenerates, mechanical stress increases and the formation of osteophytes occurs, which form along the ventral part of the spinal canal.
Often associated with spondylosis, degenerative changes in the facet joints, hypertrophy of the ligamentum flavum, and ossification of the posterior longitudinal ligament are associated with this condition. All this can contribute to damage to pain-sensitive structures (eg, nerves, spinal cord), which creates various clinical syndromes. Spondylotic changes are often observed in people of the older age group. However, only a small percentage of patients with radiographic evidence of cervical spondylosis are symptomatic.
Treatment of cervical spondylosis is usually conservative; the most commonly used treatments are nonsteroidal anti-inflammatory drugs (NSAIDs), physical modalities, and lifestyle modifications. Sometimes surgical treatment is performed.
Surgical treatment is recommended for cervical radiculopathy with persistent symptoms and lack of effect from conservative treatment.
Indications for surgical treatment of cervical spondylogenic myelopathy are somewhat controversial, but most clinicians recommend surgical therapy in the presence of moderate to severe myelopathy.
Epidemiology
Cervical spondylogenic myelopathy is the most common cause of non-traumatic spastic paraparesis and quadriparesis. Almost 23.6% of patients with non-traumatic myelopathic symptoms had cervical spondylogenic myelopathy.
Cervical spondylosis is more common in men.
The results of studies using radiographic data showed that spondylous changes are most common in people over 40 years of age. After all, more than 70% of men and women suffer from spondylosis in adulthood, but radiographic changes are more pronounced in men than in women.
Danger of sprains
People of any age are at risk of spinal ligament sprains. With weak back and abdominal muscles, the supporting function of the spine fails. Due to insufficient training, ligamentous structures are subject to high stress, which leads to their stretching and sometimes rupture. The main causes of sprains include leading a sedentary lifestyle, as well as playing strength sports.
What are the symptoms of sprained yellow ligaments of the spine?
- Pain syndrome immediately after a sudden load, reaching its maximum threshold on the second day;
- Muscle tension at the location of damaged ligaments;
- The pain increases during movement, but when returning to a state of rest, the pain goes away.
Causes of cervical spondylosis
The bones and cartilage in the neck are prone to wear and tear, which can lead to the development of cervical spondylosis. The most likely causes of the condition:
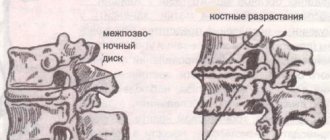
- Bone spines (osteophytes)
These bone growths are the result of the body responding to increased stress by trying to increase the amount of bone tissue in order to strengthen the spine. However, additional bone formations can put pressure on the nerve structures with the formation of pain.
- Disc degeneration
Between the vertebral bones are discs, which are thick pads that absorb force vectors from lifting, twisting, and other activities. The material inside these discs may dry out over time. This causes the bony surfaces of the vertebrae to touch when moving, which can become a source of pain. According to the Mayo Clinic, degeneration typically begins around age 40.
- Herniated disc
Intervertebral discs can develop cracks, allowing the disc's cushioning material to leak. Bulging discs can cause compression on the roots or spinal cord with the development of certain neurological symptoms (pain, sensory disturbances, muscle weakness).
- Injury
If the patient has had neck injuries, for example, whiplash during an accident, this accelerates degenerative processes.
- Ligament compaction
The tight ligaments that connect the vertebral bones to each other can become even stiffer over time, affecting the mobility of the movement segments of the neck.
- Excessive load
Some professions or hobbies involve repetitive movements or heavy lifting.
Ligament hypertrophy
Hypertrophic processes in the yellow, anterior longitudinal and posterior ligaments develop for many reasons. These include previous back injuries, sprains, and an inflammatory process that occurs after injury or hypothermia.
Sometimes the thickening progresses very quickly. The reasons for this phenomenon are not well understood, but it is believed that the triggering factor is prolonged tension in the ligaments, causing complex biochemical disorders.
With partial destruction of the intervertebral joints and vertebrae, pathological hypertrophy of the yellow, anterior and posterior longitudinal ligaments also develops. This is a protective reaction of the body to the instability that has arisen in certain segments of the spinal column. Thickened ligaments take on the role of a supporting frame.
Risk factors
The biggest risk factor for developing cervical spondylosis is aging. Cervical spondylosis is usually associated with involutional changes in the joints of the neck. Disc herniation, degeneration and bone growths (osteophytes) are all associated with involutional changes in the body.
Other risk factors:
- neck injuries
- heavy lifting work that places additional strain on the neck
- holding the neck in an awkward position for a long time or repeating the same neck movements throughout the day
- genetic determination
- smoking
- overweight and inactivity
Calcification syndrome
Common pathologies of the ligamentous apparatus include calcification of its connective tissues. The development of chronic inflammation of the yellow ligaments due to dystrophic changes (ligamentosis) leads to the following problems:
- Calcification is caused by the accumulation of calcium salts in the connective structures;
- Ossification is associated with ossification of ligamentous elements at the sites of their attachment to the bone surface.
The development of an irreversible calcification process results in a loss of connective tissue strength. This threatens the spine with the appearance of pain in the back area with an increasing likelihood of injury.
Without adequate treatment to stop ossification, loss of mobility of the spinal column is predicted. Calcification usually spreads along several yellow ligaments, which leads to the destruction of cartilaginous discs, fusion of the vertebrae, and symptoms of ankylosing spondylitis.
Symptoms of cervical spondylosis
Most people with cervical spondylosis may not experience significant symptoms. If symptoms do appear, they can be variable (mild or severe), acute or chronic.
A common symptom is pain around the shoulder blade. Some complain of pain along the arm and fingers. The pain may intensify:
- in a standing position
- into a sitting position
- when sneezing
- when coughing
- neck extension
Another common symptom is muscle weakness. Muscle weakness makes it difficult to lift your arms or grasp objects.
Other common symptoms include:
- stiffness that gradually increases
- headaches that most often occur in the back of the head
- sensory disturbances in the upper or lower extremities
Less common symptoms often include incoordination and loss of bladder or bowel control. These symptoms require emergency medical attention.
Mechanisms of spinal stenosis formation
With isolated (without calcification) hypertrophy of the yellow, anterior and posterior longitudinal ligaments, their volume increases, which partially fills the spinal canal from the inside. Its lumen narrows and spinal stenosis develops. This type of stenosis is an acquired disease and often occurs in old age.
The next stage of ligament thickening is its calcification, which aggravates the severity of the disease and worsens its prognosis. {banner_st-d-2}
When should you see a doctor?
If a person suddenly experiences numbness or tingling in the shoulder, arms or legs, or if the person has lost bowel or bladder control, then seek medical help as soon as possible!
If discomfort and pain begin to interfere with daily activities, it is necessary to consult a neurologist. Despite the fact that spondylosis is part of involutional changes, there are nevertheless various treatment methods that can improve well-being and reduce symptoms.
Standard surgical treatment
Standard treatment for central stenosis involves performing an open operation - microsurgical decompression of the spinal canal. For lateral stenosis, root decompression and interspinous implants are installed. Open surgery is effective in 90% of cases. The results persist 10 years or more after the intervention.
But such operations have a big drawback: they are very traumatic. The intervention is performed through a large incision. The doctor has to excise the bone structures, which disrupts the stability of the spinal column. The syndrome of unsuccessfully operated spine may develop; adjacent segments are often affected. With osteoporosis, fractures of the vertebral bodies are possible after treatment. As a result, many patients will require repeated interventions to correct the consequences of too traumatic treatment.
Recovery after open surgery is long and difficult. You need to wear a rigid corset for at least 1 month. Do not lean forward or lift more than 3 kg. It is advisable to completely avoid sitting. After a period of severe restriction, the muscles atrophy and the patient requires several months of rehabilitation to return to their previous physical condition.
Our expert in this field:
Malakhov Igor Yurievich
Neurosurgeon
Call the doctor
Call the doctor
Physical examination
First, the doctor finds out the presence of symptoms, their intensity, location, and history of the disease. A neurological examination is then performed, which includes examining reflexes, testing muscle strength, and determining sensory deficits and range of motion in the neck. A doctor may perform a gait analysis to determine how much damage to the spinal cord is present.
If a doctor suspects cervical spondylosis, he will order imaging tests and neurophysiological studies to verify the diagnosis.
Diagnostic measures
Hypertrophy of a structure such as the ligamentum flavum is often asymptomatic. The clinical picture is blurred, so laboratory and instrumental examinations are needed to make a correct diagnosis.
As a rule, an X-ray image shows a narrowing of the spinal canal, a violation of the integrity or location of the vertebrae. A more accurate diagnostic method is magnetic resonance imaging. This procedure allows you to assess the condition of not only the yellow ligaments, but also nearby tissues and structures.
During the diagnostic process, it is extremely important to find out what exactly caused the hypertrophy and whether there are any concomitant diseases, in particular osteochondrosis, hernia, displaced intervertebral discs, etc.
Visualization methods
- X-rays can be used to visualize bone spurs and other abnormalities.
- A CT scan can provide more detailed images of the neck.
- MRI scans, which create images using radio waves and a magnetic field, help doctors detect compression of nerve structures.
- Myelogram - This procedure uses contrast to be injected into specific areas of the spine. A CT scan or x-ray is then used to take more detailed images of these areas.
- EMG (ENMG) is used to test the functionality of nerve fibers, the method checks the electrical activity of the nerves and the conduction of impulses to the muscles.
- ENMG determines the speed and strength of the signals that the nerve sends. This allows you to determine the presence and level of damage to nerve fibers.
Osteochondrosis and other degenerative lesions of the lumbar spine are among the most common chronic diseases: 20–40% among the adult population [1]. The main pathomorphological substrate of osteochondrosis is damage to the intervertebral disc (IVD), especially in young patients. In patients over 50 years of age, along with damage to the IVD, there is a tendency to form multifactorial spinal canal stenosis (SCS), caused by hypertrophy of the elements of the articular-ligamentous apparatus of the spine - degenerative SCS.
Pathological narrowing of the spinal canal (SPNS) at the lumbar level is also called lumbar stenosis. If such compression is accompanied by progressive damage to the spinal cord and/or its roots, surgical decompression is required. The incidence of PCOS not associated with disc herniation among patients with osteochondrosis is 3–10% [2–4]. In addition to osteochondrosis, the causes of SPKD can be congenital anomalies of the spine, traumatic injuries to the vertebrae, neoplasms, hematomas, abscesses of the spinal canal, periarticular cysts, damage to the vertebral joints in rheumatoid arthritis, etc. Considering that this pathology is more typical for elderly patients, It is obvious that the incidence of SPKP will increase due to the trend towards aging of the population.
The purpose of this work is to summarize current data regarding indications for surgery for degenerative SPC.
The first mentions in the literature of SPKP as a cause of weakness and muscle atrophy in the lower extremities date back to 1803 (cited from [5, 6]). The pioneer in a detailed study of degenerative lumbar spinal stenosis is considered to be Henk Verbiest (1954), who described the syndrome of “neurogenic intermittent claudication,” introduced a classification of stenosis, and also described 4 patients with lumbar stenosis who underwent laminectomy, which led to regression of complaints [7] . The advent of CT and MRI methods has expanded the understanding of the pathomorphological substrate and pathogenesis of SPKP.
Pathological anatomy
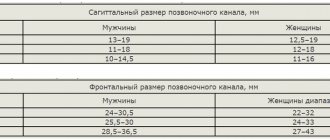
According to localization, SPC is divided into central, lateral and mixed/combined (central and lateral). Central includes stenosis of the middle zone of the spinal canal - at the level of the dural sac, lateral - stenosis in the area of exit and passage of the root, including the foraminal foramen (Fig. 1). Central stenosis is diagnosed based on a decrease in the anteroposterior (sagittal) size of the spinal canal. Normally, its size at the lumbar level is 25-15 mm (Fig. 2). A decrease in the anteroposterior size of the canal of less than 12 mm is considered relative spinal canal stenosis, and less than 10 mm is considered absolute spinal stenosis [8]. Lateral stenosis is diagnosed based on a decrease in the size of the radicular canal (another name for the radicular canal is the zone of lateral recess with a transition to the zone between the pedicles of the arches) and the foraminal foramen (Fig. 3) [9, 10]. Normally, the anteroposterior size of the root canal is at least 5 mm (Fig. 3, a), a decrease is regarded as stenosis [11, 12]. Normally, the height of the intervertebral foramen is 20–30 mm, width 8–10 mm, and a decrease in its height of less than 15 mm is regarded as SVC (Fig. 4) [13].
Rice. 1. Schematic representation of axial and frontal sections of a lumbar vertebra. a - general image; b — zone of central stenosis; c — zone of lateral stenosis.
Rice. 2. Schematic representation of an axial section of a lumbar vertebra; the arrow shows the anteroposterior (sagittal) size of the spinal canal.
Rice. 3. Schematic representation of axial sections of the lumbar vertebrae, the zones of passage of the nerve root are marked (arrow). a—recession zone; b — interpeduncular zone; c - foraminal opening.
Rice. 4. Schematic representation of the spinal motion segment with a radicular foramen and an exiting root. a — unchanged vertebrae; b — vertebrae with severe osteochondrosis, spondyloarthrosis, and a pronounced decrease in the height of the radicular foramen (arrow) — foraminal SPK.
The two main pathomorphological substrates of SPKP are spondyloarthrosis with hypertrophy of the joints and the yellow ligament (interaricular ligamentosis) (Fig. 5). It is believed that spondyloarthrosis with joint hypertrophy is the main cause of SPK in 50-70% of cases, hypertrophy of the ligamentum flavum in 10-30% [14-18]. More rare causes of the formation of SPK are synovial cysts of the vertebral joint and/or large osteophytes, sometimes in combination with IVD protrusion. If the patient simultaneously has all of the listed pathological changes, the stenosis is defined as multifactorial (Fig. 5, f). Spondyloarthrosis is usually the cause of both lateral and central stenosis or a combination of both. Hypertrophy of the ligamentum flavum is a common cause of central stenosis. In the lumbar spine, there is a tendency for the shape of the spinal canal to change from the first lumbar to the fifth vertebra: from round, then triangular, then trefoil-shaped (Fig. 6). The anatomical prerequisite for the formation of the SPCS is the constitutionally determined trefoil-type shape of the spinal canal [19]. With this canal shape, there is an anatomically narrow lateral recess.
Rice. 5. Schematic representation of the various causes of lumbar stenosis. a — unchanged vertebra; b - hypertrophy of the arch and vertebral joint - spondyloarthrosis (arrow) with the formation of predominantly lateral stenosis; c — hypertrophy of the ligamentum flavum (arrow) with spondyloarthrosis with the formation of both central and lateral stenoses; d — marginal osteophyte of the vertebral body (arrow) with the formation of lateral stenosis; e — central extended osteophyte of the vertebral body with disc protrusion (arrow) and the formation of central stenosis; e - multifactorial stenosis caused simultaneously by hypertrophy of the arches and spondyloarthrosis, hypertrophy of the ligamentum flavum, extended osteophyte of the vertebral body with disc protrusion.
Rice. 6. Schematic representation of various forms of the spinal canal of the lumbar vertebrae in an axial projection. a - round shape; b - triangular; c - in the form of a trefoil.
Clinical picture
The clinical picture of SPKP can be varied, which is determined by the pathogenetic features of the disease [20-22]. The classic manifestation of central SPCS is neurogenic intermittent claudication syndrome. Patients complain of weakness and heaviness and/or pain or cramps (cramps) that suddenly appear in the lower extremities when walking. The pathogenesis of this syndrome is due to the fact that during walking, mini-rotation movements occur in the spine and an increase in blood supply to the epidural veins, which leads to an additional increase in compression of the neural structures in the area of stenosis. These complaints partially regress if the patient squats or leans forward, since flexion of the spine increases the volumetric space in the spinal canal. Since one of the causes of suffering is spondyloarthrosis, patients may present complaints typical of damage to the vertebral joints - persistent, aching pain in the area of the affected joints, intensifying after sleep or prolonged stay in a horizontal position, as well as when bending back and decreasing after warming up. Due to muscular-tonic syndrome with spondyloarthrosis, pain can radiate to the lower extremities no lower than the level of the knee. Palpation of the affected joint area causes severe pain. The central SPKP is often combined with the lateral one. In the presence of lateral stenosis, the spinal root is compressed, which causes radicular symptoms that worsen when walking. In rare cases of isolated lateral stenosis, SPKP manifests as monoradicular disease only. Loss of functions in SPCS is determined by the number of compressed neural structures in the area of stenosis: from the absence of any neurological deficit to severe paresis, sensory impairment and dysfunction of the pelvic organs. Thus, the clinical picture of degenerative SPCS is quite diverse and, in addition to the classic syndrome of neurogenic intermittent claudication, may include other mono- and polyradicular symptoms. It is important that due to the lack of reserve spaces in the spine at the level of stenosis, the patient is predisposed to serious damage to neural structures even with minimal spinal trauma.
Differential diagnosis
Intermittent claudication in SPK must first of all be differentiated from intermittent claudication in patients with chronic lower limb ischemia (CLI) (see table) [23]. HINK will lead to hypoxia, metabolic disorders and tissue acidosis, which is the cause of muscle pain that occurs when walking. The main cause of CLI is atherosclerosis, however, in young patients, arterial damage may be associated with anomalies of their development, arteritis, fibromuscular dysplasia, cystic adventitial disease, arterial dissection, compression of the artery by a tumor, etc. It is also necessary to take into account the possible combination of two types of intermittent claudication, if a patient with SPKP has concomitant stenotic arterial lesions.
Differential diagnosis between neurogenic and vascular intermittent claudication
The appearance of pain in the muscles of the lower extremities, which intensifies when walking, is also possible with thrombosis of the deep veins of the lower extremities, in particular in young people with a genetically determined tendency to hypercoagulability. Venous thrombosis is characterized by Homans and Moses symptoms, swelling of the limb, and usually one-sided lesions. However, in the case of deep vein thrombosis only at the level of the leg, these manifestations may be minimal. The diagnosis is verified by duplex scanning of the veins of the lower extremities. Pain, cramps and weakness in the leg muscles when walking occur in a rare pathology - glycogenosis associated with a defect in muscle phosphorylase (McArdle disease). In the case of a local form involving the muscles of the lower extremities, the disease clinically manifests itself as intermittent claudication. The diagnosis is confirmed by histochemical and molecular genetic methods.
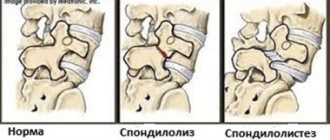
Instrumental diagnostics
Spondylography is an insufficiently informative method for diagnosing SPCS, since it does not allow adequate assessment of the size of the spinal canal. This method makes it possible to visualize severe damage to the vertebral joints and, on this basis, to suspect spondyloarthrosis, at least roughly assess the decrease in the height of the interdisc space and suspect the presence of an IVD hernia. With spondylography in a ¾ rotation, the size of the foraminal openings is indirectly assessed, on the basis of which the presence of lateral stenosis can be assumed. The informative value of spondylography lies in the diagnosis of spondylolisthesis when performing functional tests for instability of the affected spinal motion segment. In the presence of spondylolisthesis in SPKP, performing spondylography with functional tests is mandatory, since the results of these tests determine treatment tactics.
Multislice CT allows for a detailed assessment of pathological changes in bone structures and is a necessary method in the complex diagnosis of PCOS. Its use makes it possible to determine the exact bony boundaries of the spinal canal, hypertrophy of the arches and joints, characteristics of osteophytes, foraminal stenosis, ossification of the longitudinal ligament and IVD hernia, etc. [24]. The capabilities of visualizing the neural structures of the spinal canal and ligaments with this method are significantly inferior to those of MRI.
MRI (high-field) is currently the most informative method for diagnosing PCOS (Fig. 7, 8, 9). Using MRI, IVD hernias, hypertrophied vertebral joints, the degree of their impact on neural structures are visualized, and the characteristics of spinal canal stenosis are determined: localization, substrate, extent. To obtain an objective picture, MRI examination of the spine must be carried out on a device with a magnetic field strength of at least 1.0 Tesla.
Rice. 7. MRI of the lumbar spine; formation of spinal canal stenosis as a result of hypertrophy of the ligamentum flavum (arrow). a - axial projection; b, c — sagittal projection.
Rice. 8. MRI of the lumbar spine; formation of spinal canal stenosis as a result of spondyloarthrosis and hypertrophy of the facet joints. a — sagittal projection of the hypertrophied joint (small arrow), stenosis of the foraminal opening (large arrow); b — axial projection of hypertrophied facet joints (arrows).
Rice. 9. MRI of the lumbar spine, axial projection. A relatively rare cause of lumbar stenosis, a synovial cyst of the lumbar joint (arrow), is presented.
CT myelography for diagnosing SPKP is used when MRI is not possible, for example, when there are metal implants in the body. In some cases, this method allows one to assess the degree of compression of the nerve roots better than MRI. For example, in the case of multilevel lesions identified by MRI, CT myelography may be a necessary additional method to clarify the level at which surgical intervention is primarily necessary. If CT myelography is not possible, contrast myelography may be performed. Both methods demonstrate the area of narrowing of the dural sac; by the nature and side of the narrowing it is possible to indirectly judge the pathomorphological cause of the stenosis.
Treatment
Conservative treatment
Conservative treatment tactics for SPCS are chosen in the absence of neurological deficits caused by compression of neural structures in the lumbar canal [25–27]. In the presence of a neurological deficit, the possibility of surgical treatment is discussed, since delaying decompressive surgery increases the risk of irreversible damage to the neural structures in the area of stenosis. Conservative treatment is symptomatic, aimed at relieving pain and trying to slow the progression of the disease. It is impossible to cause expansion of the spinal canal in the SPCS area using conservative treatment methods, which is a fundamentally important point. Treatment includes a therapeutic and protective regimen, wearing a corset during an exacerbation, analgesics and NSAIDs, local injection of anesthetics into the area of joints and ligaments, physiotherapy, and exercise therapy. It is possible to use chondroprotectors. In some cases, with SPCS, the pain syndrome is persistent, which is associated with irritation of the nociceptors of hypertrophied joints and ligaments. In the case of a satisfactory analgesic effect when blocking these structures in such patients, it is possible to discuss the issue of minimally invasive surgical intervention - dereception [28]. In general, there are no highly effective principles of conservative treatment of SPKP; persistent nature and progression of complaints are noted during conservative treatment [25, 29-33].
Minimally invasive interventions
They are used to relieve pain that is resistant to conservative treatment if the patient does not have clinical manifestations of compression of neural structures. They include dereception of vertebral joints, ligaments, electrical stimulation, as well as transsacral epidurofibroscopy, which makes it possible to dissect adhesions and install an epidural catheter in the area of stenosis for targeted administration of anti-inflammatory and decongestant drugs [34, 35].
Surgery
If clinical manifestations of compression of neural structures are confirmed by instrumental examination data, decompression of the spinal canal is indicated [36–38]. A large number of randomized studies examining the effectiveness of microsurgical decompression of the spinal canal in SPCS have shown that 70–90% of patients after surgery experience significant or complete regression of complaints, complete or partial regression of neurological deficits [39–46]. Up to 80% of patients remain satisfied with the results of surgical treatment. Observations of operated patients for 4–10 years demonstrate the preservation of the effect of the operation [44, 47]. The high efficiency of surgical treatment of SPKD is associated with the development of microsurgical techniques. Thus, 20 years ago, the usual surgical procedure for SPK was laminectomy with removal of the vertebral joints, which led to instability of the vertebrae at the operated level and frequent recurrence of the pain syndrome (Fig. 10). Currently, microsurgical techniques make it possible to carry out radical decompression with minimal surgical trauma and preservation of all supporting structures of the spine [48–50] (Fig. 11 and 12). When choosing the type of operation, they are guided by the clinical picture and the results of instrumental examination methods. In the case of only central stenosis caused by hypertrophy of the yellow ligament and vertebral joints, microsurgical decompression of the central parts of the spinal canal is sufficient (see Fig. 11 and 12). In the case of lateral stenosis and radicular compression, microsurgical decompression of the affected root with installation of an interspinous implant is indicated (Fig. 13). Such an implant increases the height of the intervertebral foramen and turns off rotational movements in the operated spinal segment, which prevents recurrence of lateral stenosis [51]. An increase in the effectiveness of microsurgical decompression using interspinous implants has been shown [38, 52—54]. In the case of a combination of SPCS with instability of the affected segment, decompression of the spinal canal and installation of a stabilizing system are indicated (Fig. 14). Before such an operation, it is necessary to exclude osteoporosis, otherwise vertebral fractures are possible during the installation of implants and in the postoperative period. Considering that SPKP is more common in elderly patients, a number of studies have been conducted [46, 55–58] to study the effectiveness of surgical treatment in this age group. It was revealed that in patients aged 75-80 years, the positive effect of surgical treatment of SPKP was observed in 80%.
Rice. 10. Schematic representation of various types of decompressive operations for SPKP. a — spine before surgery; b — classic laminectomy with removal of the entire arch and joints; c — hemilaminectomy with removal of half the arch, partial resection of the joints; d — arcotomy — borderline resection of the edges of adjacent arches with preservation of the joints; e — modified laminectomy with partial removal of the arch while preserving the joints.
Rice. 11. Schematic representation of microsurgical decompression of the spinal canal from a unilateral approach (arcotomy) when removing the hypertrophied ligamentum flavum.
Rice. 12. Schematic representation of microsurgical decompression of the spinal canal from a unilateral approach (arcotomy) with partial bilateral marginal resection of joints on both sides.
Rice. 13. Schematic representation of an arcotomy for microsurgical decompression with installation of an interspinous implant for additional stabilization of the posterior vertebral structures, turning off rotational movements in the corresponding spinal motion segment.
Rice. 14. Schematic representation of decompression of the spinal canal with installation of an interbody implant and posterior transpedicular fusion in the combination of SPKP with vertebral instability.
Postoperative period
The next day after the operation, the patient is verticalized in a corset, and after 2-3 days he is discharged home. For 1 month after the operation, the patient maintains a strict regimen: wearing a corset, avoiding bending forward, lifting weights of more than 3 kg, and, if possible, avoiding sitting in a sitting position. Osteochondrosis and osteoarthrosis are chronic progressive diseases. After decompression of spinal stenosis, they persist, and in the presence of risk factors, the likelihood of relapse of stenosis at the operated level and damage to other parts of the spine remains. It is important to adhere to a protective regime: avoiding heavy dynamic and static loads, sudden, jerking movements, daily performance of a certain set of exercise therapy exercises aimed at strengthening the muscular corset and abdominal muscles, and regular swimming.
Conclusion
One of the consequences of degenerative lesions of the vertebrae and IVD is SPC. This pathology is more typical for mature and elderly patients. Due to the aging population, lumbar stenosis is increasingly encountered in the practice of neurologists and neurosurgeons. The clinical picture is varied: from moderate pain to severe neurological deficit, characterized by neurogenic intermittent claudication. In the case of isolated pain syndrome and the absence of clinical manifestations of compression of neural structures, conservative treatment is indicated for the patient. In case of ineffective treatment of pain syndrome, the use of minimally invasive interventions is indicated - dereception of vertebral joints and/or ligaments, therapeutic and diagnostic epidurofibroscopy. In the presence of a neurological deficit (neurogenic intermittent claudication, mono- or polyradicular syndrome), conservative treatment is ineffective; it is necessary to resolve the issue of surgical decompression of the spinal canal. Modern microsurgical techniques make it possible to perform a radical operation with minimal surgical trauma; the patient is verticalized the next day and after 2-3 days he can be discharged home. With adequate selection of patients for surgery, 90% of operated patients experience regression of neurological deficit and pain, which allows us to judge the high effectiveness of the method. After surgery, in order to exclude recurrence of stenosis and/or damage to another spinal segment, the patient is required to maintain a certain lifestyle: do not overload the spine, do physical therapy, swimming, etc. every day.
Treatment of cervical spondylosis
The goal of treating cervical spondylosis is to reduce pain, reduce the risk of permanent damage, and restore the patient to a normal lifestyle. Non-surgical methods are usually very effective and avoid surgery.
Treatment options for cervical spondylosis include neck immobilization, pharmacologic treatment, lifestyle modifications, and physical modalities (eg, traction, manipulation, exercise).
•Neck immobilization
(using a soft collar or a rigid orthosis) is often used as a non-operative treatment for neck pain and/or suboccipital pain syndromes caused by spondylosis and cervical radiculopathy.
As symptoms improve, the collar should only be worn during strenuous work. Eventually, you can stop wearing the collar.
Stiffer orthoses and devices may better restrict cervical spine motion, but they can reduce muscle tone and cause neck stiffness. Using a daily neck exercise program can limit the loss of muscle tone.
Treatment of the ligamentum flavum using manual therapy methods
Currently, official medicine does not have effective pharmacological drugs that allow treating the ligamentum flavum without surgery. The volume of hypertrophied tissue can be reduced using manual therapy methods. With a properly developed individual course, the patency of the spinal canal is completely restored and all clinical symptoms are eliminated.
We use the following methods to treat the ligamentum flavum of the spine:
- massage and osteopathy to restore impaired microcirculation of blood and lymphatic fluid in the affected area;
- therapeutic exercises and kinesiotherapy to restore the physiological state of the ligamentous apparatus of the spine;
- reflexology – to launch tissue repair processes through the use of hidden reserves of the human body;
- traction traction of the spinal column, increasing the elasticity and structural structure of the ligaments;
- laser exposure and physiotherapy methods.
If you require treatment for the ligamentum flavum, we recommend that you make an initial appointment with a vertebrologist at our manual therapy clinic. Consultation with a doctor is free. During your appointment, you will learn about all the possibilities and prospects for manual therapy in your individual case.
Other types of therapy
The ligamentum flavum is an important component that ensures the integrity and mobility of the spinal column. Therefore, it is extremely important to restore normal functioning of the ligaments and prevent developing stenosis. For this purpose, a variety of types of treatment are used:
- physiotherapy, in particular electrophoresis and ultrasound, eliminates swelling and pain and accelerates metabolism;
- massage helps relieve spasms, improve blood flow and tissue trophism, strengthen the muscle corset, thereby relieving the load on the spine;
- manual therapy is carried out in order to eliminate displacement of intervertebral discs and relieve pressure from nerve endings (the procedures should be carried out by an experienced specialist; such treatment at home can be dangerous);
- therapeutic exercises, as regular, properly selected exercises help strengthen muscles and ligaments.
Of course, the treatment regimen is drawn up by the attending physician. In most cases, the prognosis for patients is favorable.