What is osteoporosis of the foot
When moving, a significant load is placed on the feet, this can provoke the development of osteoporosis
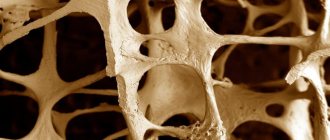
Osteoporosis of the foot appears as a result of damage to bone tissue, in which its structural changes are observed. They can occur against the background of deterioration of metabolic processes and decreased metabolism. One of the most common causes is calcium deficiency. If salts are not retained in the bone tissue, it becomes loose and brittle.
This type of osteoporosis develops quite often and occurs due to significant loads on the feet that occur during a person’s movement. The fact is that the entire weight of the human body falls on these parts of the legs. However, this is far from the only factor that can provoke the course of this disease.
At the very beginning of development, the pathology is focal in nature, affecting only some elements of the foot. Further, due to the loss of calcium, bone tissue begins to change significantly, which leads to a decrease in its density and loss of bone mass. The bone itself gradually becomes thinner and loses strength.
Such processes ultimately lead to fractures and various bone injuries. In general, serious injury can occur even with light loads. For example, the risk of fracture occurs even when walking on a flat surface.
The main disadvantage of this disease is its asymptomatic course in the early stages. It is during this period that therapy can be truly effective. However, the disease most often manifests itself when aggressive treatment is required to eliminate it, which is no longer capable of producing significant results.
Regional migratory osteoporosis (clinical observation)
A pulmonary neurodystrophy
(reflex sympathetic dystrophy syndrome) is well known.
Diagnosis of this disease in the case of a classic clinical picture, especially when the hand or foot is affected, usually does not cause difficulties. One of the frequent, but less well-known forms of the disease includes cases of simultaneous or sequential damage to several anatomical zones of the musculoskeletal system - the so-called plurifocal forms of algoneurodystrophy
.
A typical example is the “shoulder-hand” syndrome ( Steinbrocker syndrome
), observations of “bipolar” forms of algoneurodystrophy of other (very different) localizations are known, as well as “multifocal” lesions, when changes are noted, for example, in the area of the knee, hip joints and foot, or from the shoulder, hand and foot [1].
To describe cases of algodystrophy, the feature of which is sequential (separated by relatively short intervals) damage to two or more areas of the musculoskeletal system, the term “regional migratory osteoporosis”
[2]. We present our observation of this variant of algoneurodystrophy.
Patient Z., 45 years old.
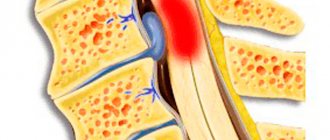
In December 1998, he suffered a traumatic closed fracture of the fifth metatarsal bone of his left foot. A month after plaster immobilization, satisfactory healing of the fracture was noted, and there was no pain. After another 3 months (April 1999), for no apparent reason, constant pain appeared in the entire left foot, as well as diffuse swelling of this area, spreading to the lower third of the leg, hyperemia and hyperthermia of the skin, and increased local sweating. These phenomena quickly intensified, reaching their maximum severity after about a month and depriving the patient of the ability to step on his left leg.
On X-ray examination (June 1999)
Diffuse osteoporosis of a patchy nature was revealed in all the bones of the left foot and the bones of the lower leg in the ankle joint (Fig. 1). The general condition was not disturbed, no changes were detected during laboratory examination. There was no significant effect from therapy with prednisolone (50 mg per day, followed by dose reduction and withdrawal after 3 weeks), calcitonin (100 IU intramuscularly daily), or novocaine conduction blockades. But by August (that is, a total of 3 months from the onset of the disease), the pain and swelling spontaneously disappeared, the function of the left foot was restored, and he began to walk without limping. In September 1999, the patient tripped and injured his left knee joint. The bruise was not severe, but the pain in the area of the left knee joint not only did not go away over time, but quickly intensified. They bothered me both when walking, causing lameness, and at rest.
Upon examination
moderate swelling of the left knee joint, severe pain on palpation of both the joint itself and the periarticular tissues, significant limitation of joint flexion, and hypotrophy of the left quadriceps muscle were noted. There were no changes in the area of the left foot and lower leg; only a slight painless limitation in the flexion of the left ankle joint was noted.
X -ray of the knee joints (January 2000)
Moderate widespread osteoporosis of the bones making up the left knee joint, including the patella, was revealed (Fig. 2). Repeat radiographs of the left foot showed widespread osteoporosis.
With skeletal scintigraphy
(99mTe-technifor) accumulation of radionuclide was established in the area of the knee joint, mainly in the articulating parts of the femur and tibia, the patella and soft tissues of the popliteal region (Fig. 3).
About 2 ml of viscous non-inflammatory fluid was extracted from the cavity of the left knee joint (no cells or crystals were found under microscopy).
During ultrasound examination
There were no signs of damage to the internal structures of the left knee joint. No deviations from the norm were found in the general blood test, biochemical and immunological studies.
Only local therapy
: repeated intra-articular and periarticular administration of hydrocortisone. After about 3 weeks, the pain in the left knee joint completely disappeared, and its function was restored. Judging by the information received after 10 months (November 2000), the patient noted moderate pain when walking in the area of the left ankle and left knee joint.
Discussion
The presence of algoneurodystrophy in the observed patient did not raise any doubts in our minds, since both during the first and during the second episode the classic picture of this disease took place [1]. Following the injury (approximately 4 months after the first and almost immediately after the second), severe pain developed, inadequate to the degree of injury and extending beyond the injured area, local vasomotor disturbances, especially pronounced during the first episode (widespread swelling of the foot, hyperemia and hyperthermia of the skin ), as well as sweating disorders. The pain in the affected foot was of the nature of allodynia, that is, it was noted when exposed to usually neutral stimuli. The function of the affected limb segments was sharply impaired; for some time after each episode of algoneurodystrophy, the patient could not bear weight on his leg. But the most convincing sign of algoneurodystrophy was regional widespread osteoporosis, which is revealed only by X-ray examination
. During the first episode of the disease, it was detected in all the bones of the left foot, as well as in the bones of the corresponding lower leg in the lower third, and during algoneurodystrophy of the knee joint - in the articulating tubular bones and the patella. And, finally, algoneurodystrophy was supported by the almost complete positive dynamics of clinical manifestations, which occurred, to a greater extent, spontaneously, and not under the influence of the treatment used. No signs of other diseases that may partially resemble algoneurodystrophy (damage to motor or sensory peripheral nerves, ischemic bone necrosis, infections or somatoform mental disorders) were observed.
The main feature of this observation is the sequential development of the algoneurodystrophic process in two localizations.
The second episode of the disease occurred a short period of time (approximately 5 months) after the first. This variant of algoneurodystrophy is known in the literature under the name “regional migratory osteoporosis,” probably first proposed by Duncan H. et al. (1967). Although regional migratory osteoporosis is a particular form of “plurifocal” algoneurodystrophy, works published under this name usually report cases of sequential damage to two, less often three, anatomical zones of the lower extremities (usually the feet, knee and hip joints). In some cases, the disease is preceded by trauma, but often no apparent cause is found. The interval between individual episodes of algoneurodystrophy ranges from several weeks to several years; a “return” of the pathological process to the previously affected area is not observed [2,3]. Published reports indicate a favorable outcome in regional migratory osteoporosis, which was also observed in our patient. References
1. Doury P, Dirheimer J, Pattin S. Algodystrophy. Springer-Verlag, Berlin, Heidelberg, New York;, 1981.
2. Duncan H., Frame B., Frost H. et al. Migratory osteolysis of lower extremities. Ann. Intern. Med. 66:1165-1173, 1967.
3. Gupta R, Popovtzer M, Huffer W, Smyth C. Regional migratory osteoporosis. Arthr. Rheum. 1973; 16:363-368.
| Applications to the article |
| Rice. 1. Radiographs show a pronounced widespread increase in transparency of most of the bones of the left foot and the distal parts of the bones of the left leg (June 1999). |
| Rice. 2. Radiographs of the knee joints of the same patient on the left show moderate periarticular osteoporosis, as well as osteoporosis of the patella (January 2000). |
| Rice. 3. Skeletal scintigraphy (99mTe-technifor). Hyperfixation of radionuclide in the articulating parts of the femur and tibia, patella and soft tissues of the left popliteal region (January 2000). |
Causes of the disease
This disease can develop for a number of reasons:
- Age-related changes in the body. Most often, osteoporosis of bones and feet is observed in women after 50 years of age. The development of the disease most actively occurs during menopause or postmenopause.
- Calcium deficiency. This condition most often occurs with hormonal imbalance and gastrointestinal diseases. The latter are most often observed in men, especially against the background of alcohol abuse, as well as poor nutrition. Due to the physiological characteristics of the body, calcium deficiency due to smoking most often occurs in the female population.
- Excessive exercise, especially those types that place significant stress on the musculoskeletal system.
- Wrong lifestyle. We are talking about low activity, sedentary work.
- Excess body weight. Obesity of the 2nd and 3rd stages contributes to the occurrence of additional stress on the bone structure. As a result, the patient develops a deficiency of phosphorus and calcium, problems with the endocrine system and gastrointestinal tract.
- Heredity. Scientists have proven that osteoporosis occurs with a higher frequency in Europeans and representatives of the Mongoloid race. The disease also affects people whose relatives have previously encountered this problem.
Risk factors for osteoporosis
In childhood and adolescence, the process of bone tissue formation significantly prevails over its resorption. The older a person gets, the more bone destruction begins to prevail over its formation. The process of bone resorption intensifies especially in women after menopause. That is why osteoporosis in women is a typical and very common disease that occurs in old age.
There are factors that increase the risk of developing osteoporosis:
- female gender (women are much more susceptible to this disease than men);
- osteoporosis in blood relatives in the family (genetic predisposition to this disease is very important);
- age (as we mentioned earlier, with age the likelihood of developing the disease increases significantly);
- low mobility (immobilization, fixation of the patient’s limbs or body in case of injury, significant patient weight, mental disorders that make movement difficult - all these conditions are causes of the development of osteoporosis);
- drug therapy using glucocorticoids, high doses of thyroxine (a synthetic analogue of the thyroid hormone); bone tissue is also negatively affected by long-term use of aluminum-containing drugs - for example, antacids used to reduce the acidity of gastric juice during gastritis or peptic ulcers;
- the patient is overweight or underweight.
The patient cannot always change anything about the causes of osteoporosis, even if he understands that they can be dangerous. Indeed, neither gender nor age (the main risk factors) can be changed. However, there are factors that the patient can and should change in order to reduce the risk of developing such a dangerous disease. Smoking, excess consumption of alcohol and caffeine-containing drinks, lack of exercise, low consumption of foods rich in calcium (for example, dairy), little sun exposure, insufficient vitamin D intake - all of these factors can be changed, which is why they are called modifiable factors. risk.
Types and stages of osteoporosis
This disease is difficult to treat and is extremely dangerous.
Regarding the localization features, this disease is divided into the following types:
- Focal form. It is also called local. Usually this form is present in the early stages of the development of the disease, when it affects only some tissues of the foot. In the absence of adequate treatment, the lesions grow, unite and invade new areas.
- Diffuse. The most dangerous form, since it is the one that is characterized by damage to the maximum amount of foot tissue. Conservative methods do not help in this case and radical intervention is necessary.
Regarding the nature of the disease, there are five types of osteoporosis of the feet:
- Postmenopausal. Its cause is insufficient production of female sex hormones, which occurs during menopause.
- Local. The disease occurs in a specific area due to a number of reasons, without affecting other areas.
- Senile. Associated with wear and tear of bones and joints. Typically, the skeleton loses mass and strength after age 65.
- Secondary. It is one of the complications of diabetes mellitus in the presence of hypothyroidism, pulmonary diseases, chronic renal failure, various types of oncology, rheumatoid arthritis, chronic hepatitis, etc.
- Corticosteroid bone dystrophy. It is the result of long-term use of glucocorticoids.
Regarding the severity of the course, there are 4 stages of osteoporosis of the leg joints:
- The first stage is characterized by minor tissue damage. One or more lesions appear that do not cause discomfort to the patient and are not detected on x-rays.
- Second stage. Characterized by the appearance of a larger number of foci. A person may feel minor discomfort, but most patients attribute it to simple fatigue. Some changes may be visible on x-rays, and in most cases, osteoporosis of the toes at this stage is detected by chance.
- Third stage. At this stage, the disease enters a severe form of its development. Pain and visual changes in the foot appear. If treatment begins at this stage, then in most cases it will be ineffective.
- Fourth stage. It is the most severe and involves assigning the patient a disability.
How is osteoporosis prevented?
Prevention should include several areas aimed at eliminating the previously listed risk factors for osteoporosis.
It is important to ensure sufficient intake of calcium and vitamin D from food - for this you should eat dairy and other calcium-rich foods listed above. You should reduce your consumption of alcohol and caffeine-containing drinks and foods.
There are a number of scientific studies showing that long-term use of calcium and vitamin D supplements for the purpose of prevention can reduce the risk of developing osteoporosis. Taking moderate doses of calcium with vitamin D for 3-4 years does not lead to side effects, but can improve bone density. It is enough to take calcium carbonate in a dose of 500 mg with 200 IU of vitamin D twice a day (for example, calcium D3 Nycomed, 1 tablet 2 times a day; or Calcemin-Advance, also 1 tablet 2 times a day). Taking calcium and vitamin D supplements is safe even if you have urolithiasis. However, the issue of preventive therapy should still be decided after consulting an endocrinologist.
Physical activity is the next factor to prevent the development of osteoporosis. Prevention using physical activity can increase the load on the bone and stimulate its strengthening.
For women during menopause, an important factor in the prevention of osteoporosis is the use of hormone replacement therapy, which allows them to “imitate” normal ovarian function for a long time and reduce the risks associated with the extinction of the natural hormonal function of the ovaries. Such therapy is also an effective factor in the treatment of osteoporosis, if it has already occurred. Of course, the selection of treatment is carried out by an endocrinologist.
One should not forget about the need to monitor thyroid function if the development of osteoporosis is suspected. To do this, it is enough to perform an ultrasound of the thyroid gland and pass a basic set of tests (usually for the first examination it is enough to donate blood for TSH, T4 free, and antibodies to thyroid peroxidase). When taking tests, do not forget about the need to monitor the level of ionized calcium annually! Timely detection of an increase or decrease in blood calcium levels greatly facilitates treatment.
Symptoms
As mentioned above, the insidiousness of this disease lies in its long asymptomatic course. Therefore, early diagnosis of the disease is difficult, and most patients consult a doctor only when the consequences are irreversible.
Most often, the pathology causes bone fragility, when an ankle fracture is possible even with minor loads. This can be caused by poor foot placement during movement, landing in a jump, or making sudden movements.
The characteristic symptoms of osteoporosis of the legs appear in accordance with the progression of the disease:
- Initially, pain may only occur when walking up stairs. However, as the disease develops, it manifests itself even at rest.
- Pain is present when pressing on the affected bone.
- Starting from the third stage, swelling and redness occur.
- Over time, the pain becomes so severe that the patient is limited in movement, and his gait changes.
- Against the background of osteoporosis of the foot, general signs of deterioration of the patient’s condition are possible, such as sleep disorders, stooping, fatigue, weakness and decreased ability to work.
If the disease becomes systemic, it will radically affect the condition of the nails and hair.
Reviews about
Svetlana
14.01.2021
If I had the opportunity to go back a few years and give myself advice, I would say: Sveta, throw away your heels. These shoes are beautiful and expensive, but incredibly uncomfortable and narrow. The result was osteoporosis of the foot, so I began treatment. At first I took pills, then I realized that it was useless and took it more seriously here in the center. I see the result.
Arthur
20.08.2020
I have already had my back treated at this center, and it’s time to treat osteoporosis of the foot. The doctor says. I applied just in time; another couple of years and the pain would have been unbearable. But it’s not like playing sports; it’s impossible to put on boots. The staff and doctors worked at the highest level. Thank you!
Diagnostics
Only a doctor can choose the right method of diagnosis and treatment
To identify this disease, a whole range of procedures should be carried out, including:
- X-ray of bones;
- osteodensitometry;
- computed tomography;
- ultrasonic densitometry.
Since x-rays do not show bone loss up to 30%, this method is not used for accurate diagnosis.
Traditional medicine in the treatment of osteoporosis
Start with the simplest thing - go. Go as far as possible and for as long as possible. Walking will take you away from osteoporosis and lead you to a healthy lifestyle. The more you sit, the more your muscles and bones degrade. Play sports and go to a fitness club.
Sport helps prevent osteoporosis
At any age, if the patient is not predisposed to allergies, beekeeping products: honey and propolis have an excellent therapeutic effect. We firmly believe in this and mix the following medicine:
100 g propolis, 50 g buckwheat honey, 100 g eggshells, previously dried and crushed. This miracle is taken 2 tsp. per day for at least two months.
Systemic treatment of osteoporosis with folk remedies provides significant relief. If you use herbal treatment, it is good to combine it with massage. You can try several remedies and settle on the one that seems more acceptable and effective. Women, as the main victims of osteoporosis, should select herbs with extragenic activity to produce female hormones (anise, oregano, hops, lemon balm).
Treatment with folk remedies
There are a lot of herbal-based recipes, here are just a few of them:
- Horsetail and knotweed are boiled in an enamel bowl. This decoction is drunk for a month three times a day before meals.
- Steamed nettle leaves combined with bird buckwheat.
- Brewed St. John's wort take 3 tbsp. in a day.
- Pour 100 g of chamomile and sweet clover into 0.5 liters of vodka and infuse. Not to drink! Use as compresses.
- Mix crushed eggshells and lemon juice in a 1:1 ratio. Take a quarter teaspoon per day.
- The most attentive ones manage to catch the period before the nettles bloom and prepare a spring remedy when the juice is squeezed out of the young leaves.
httpv://www.youtube.com/watch?v=embed/PM1rGJoX_D0
It is worth highlighting mumiyo as a means to combat osteoporosis. This is a mountain mineral that contains many macro- and microelements and strengthens bone tissue. Purified mummy is used, and the volume depends on the person’s weight. The solution is taken on an empty stomach according to the following scheme:
- the first 10 days - 3 times a day: in the morning and at lunch before meals, in the evening before bed,
- the next 20 days - 2 times a day: in the morning before breakfast, in the evening before bed,
- then drink in the morning on an empty stomach every 10 days with a break of 5 days.
Whether or not there is osteoporosis in your body depends directly on you. Today, a healthy lifestyle is being promoted in every possible way. You could say it's fashionable. So make it a fashion to be healthy.
Why is osteoporosis of the foot dangerous?
If this disease is not detected and treated in a timely manner, a number of negative consequences are possible:
- a significant decrease in performance, up to disability;
- Frequent bone fractures not only interfere with normal movement, but can also cause dysfunction of nerve endings and blood vessels;
- development of compensatory gait and corresponding bone deformation;
- due to a deficiency of nutrients in the body, internal organs suffer, in particular the cardiovascular system;
- severe pain due to osteoporosis in the legs limits physical activity.
Symptoms
Osteopenia usually does not cause pain as long as there is no bone fracture. In addition, even fractures with osteopenia can be asymptomatic. Osteopenia or osteoporosis may occur for many years before diagnosis. Many bone fractures due to osteoporosis or osteopenia, such as hip fractures or vertebral fractures, are very painful. However, some fractures, especially vertebral fractures, may not be painful, so osteopenia or osteoporosis may not be diagnosed for many years.
Any person who has been diagnosed with osteopenia should make lifestyle changes and work with a doctor to select medication for the correction of osteopenia.
Treatment
Proper nutrition in combination with medications has a positive effect on the treatment of osteoporosis
To obtain positive results, an integrated approach to the treatment of osteoporosis of the foot is necessary. In modern medicine, many techniques are used for this.
Drug therapy
Involves the prescription of bisphosphonates, vitamin complexes, chondroprotectors and calcium supplements.
Physiotherapy
To reduce the rate of development of osteoporosis of the ankle joint, a special set of exercises has been developed. It is selected by the attending physician depending on the stage of the patient’s disease.
Nutrition adjustments
To enrich the patient’s body with phosphorus, calcium and proteins, he is prescribed a special diet. In this case, you will have to give up pickles and fatty foods for a while, since they disrupt the functioning of the gastrointestinal tract, and calcium is washed out of the body.
Physiotherapeutic procedures
These techniques are designed to alleviate the patient’s condition and are used in combination with other types of therapy. We are talking about UHF, therapeutic baths, laser therapy, mud therapy, massage. In this case, manual massage is not used due to its aggressiveness and risk of injury to weakened bones.
Folk remedies
Used to enhance the effectiveness of essential medications. The most effective are dandelion tea, onion infusion, eggshells, etc.
Surgical intervention
If conservative therapy fails, the patient undergoes joint replacement surgery.
Given the symptoms, treatment for osteoporosis of the foot should primarily be aimed at eliminating the underlying causes of the disease. Otherwise, the therapy will not give the expected results.
Prices
| Consultation with a doctor on the treatment of osteoporosis of the foot | From 500 rub. |
| First treatment cycle (12 sessions) | From 6,500 rub. |
| Second treatment cycle (12 sessions) | From 5,900 rub. |
| One lesson | From 700 rub. |
| Foot massage | From 250 rub. |
| Simple zonal taping | From 500 rub. |
| Combined zonal taping | From 800 rub. |
Based on the results of the consultation, diagnosis and/or treatment will be prescribed.
*Prices in different regions may vary; current information on the cost of services can be obtained from the center manager.
What Causes Spot Lesions?
The focal form of osteoporosis refers to pathologies of secondary origin, because the lesion develops for certain reasons:
- due to trauma - post-traumatic osteoporosis;
- after surgery - postoperative;
- as a result of the influence of unknown sources of the disease - .
In addition, bone damage is provoked by various factors indicated in the table:
| Groups of causes causing pathology | Specific factors that provoke the disease |
| Genetic | Belonging to the Mongoloid or European race |
| Presence of osteoporosis in close relatives | |
| Low weight | |
| Lifestyle | Asthenic body type |
| Excessive alcohol consumption and smoking | |
| Adynamia - lack of physical activity | |
| Vitamin D deficiency associated with living in cold climates | |
| Gynecological | Hormonal imbalances |
| Menopause | |
| All types of infertility | |
| Endocrinological | Diabetes |
| Hypocortisolism syndrome - the release of excess hormones by the adrenal glands | |
| Hematopoietic diseases | Rheumatoid polyarthritis |
| Libman-Sachs disease, when a person’s immune system perceives its own cells as foreign and begins to fight them | |
| Chronic hemodynamic insufficiency | |
| Taking medications | Glucocorticoids - hormonal drugs |
| Anticoagulants that prevent blood from thickening | |
| Anticonvulsants | |
| Some antibiotics | |
| Cytostatics for the treatment of oncological diseases |