Causes of diseases
Arthrosis develops when:
- hereditary predisposition;
- injury;
- excessive load on the joint, which is most often caused by excess weight;
- impaired blood circulation and metabolism in the joint;
- hypothermia.
The causes of arthritis are:
- infections;
- allergies;
- injuries;
- physical exercise;
- metabolic disorder;
- rheumatism;
- diseases of the nervous system;
- deficiency of vitamins and minerals.
Quite often, arthrosis and arthritis can occur simultaneously: the degenerative processes that occur with arthrosis can cause inflammation, and inflammatory processes can lead to irreversible changes in the joint tissue.
Osteoarthritis in most cases affects one large joint, and arthritis affects several small ones.
How do diseases differ?
A disease such as arthrosis is age-related. Over time, the integrity is compromised and degenerative disorders of cartilage tissue appear. It is impossible to cure arthrosis, just as it is impossible to stop the aging process. Arthrosis is a chronic disease that occurs in waves: an acute attack is followed by a period of remission.
If you do not seek medical help, arthritis can greatly ruin your life: joint mobility will decrease, and you will be haunted by constant pain. In particularly severe cases, the disease can lead to disability. Therefore, do not delay going to the doctor, make an appointment on time. Our clinic’s specialists will help slow down irreversible changes and maximize the youth and health of your joints.
As for arthritis , it is an inflammatory disease that can affect one or more joints, adjacent tissues, ligaments and muscles. It is often a concomitant symptom of other diseases or joint injuries. The disease is treatable, especially if it is started on time. The peculiarity of arthritis is that it can spread to other joints and tissues, and also become chronic. In some cases, the disease develops gradually, in others it develops quickly and abruptly.
To cure arthritis, you first need to determine its root cause. To do this, our doctors conduct a full examination. Based on the results obtained, you will be prescribed complex therapy that will help you cope with the disease.
Age and risk groups
Arthrosis is mainly diagnosed in middle and old age. Most retirees who reach the age of 60 show degenerative signs in their joints. People who are overweight, have impaired metabolism, as well as those whose joints are subject to constant overload (athletes and people who have to remain in a stationary standing or sitting position for a long time) are especially susceptible to the disease.
Arthritis in most cases occurs in young and middle-aged people (30-55 years).
What is a heel spur and how is it treated?
Contrary to existing belief, a heel spur is not a cause, but a consequence of the disease. The human foot is a brilliant, almost perfect creation of nature. The structure of the foot resembles an arch and therefore its small bones in mass and thickness can withstand enormous loads.
Like human feet, arched bridges are constructed, assembled from thin elements and at the same time supporting the colossal mass of trains and cars.
The arched shape of the arch of the foot is supported on the plantar side by a powerful ligament - the plantar aponeurosis. The posterior end of the plantar aponeurosis is attached to the heel bone, and the 6 anterior ones diverging in a bundle are attached to the toes. In this way, it connects the forefoot and back of the foot and keeps the foot from spreading out.
Shifting the center of gravity of the body forward (stooping, excess weight, weakness of the leg muscles), especially in combination with walking, running or jumping, leads to repeated micro-tears of aponeurosis fibers from the heel bone, and healing of damaged fibers occurs by turning the damaged part of the aponeurosis into bone.
This is how the heel spur visible on x-rays appears. Pain when putting weight on the foot occurs mainly due to the appearance of new tears in the aponeurosis, and not due to the pressure of the spur on the tissues of the foot.
Relieving a patient of pain due to a heel spur is a completely doable task. Principles of treatment practiced in our center: 1. Return the center of gravity of the body to physiological limits. Usually this task is quite doable. Here we successfully use 6 methods of manual therapy and 4 methods of therapeutic exercises. 2. Support the arch of the foot from the plantar side and relieve the plantar aponeurosis. For this we use soft orthopedic insoles. The insoles fit into regular shoes. They can be used periodically or continuously. 3. Engage the calf muscles that support the arch of the foot. Often these muscles are not fully activated due to the fact that the nerve roots compressed in the lumbar spine do not fully conduct nerve impulses from the brain to these muscles (pain and/or heaviness in the lower back + heel spur). In this case, gymnastics and manual therapy again come to the rescue. 4. Relieve inflammation and stimulate healing at the site of damage to the plantar aponeurosis. To do this, we use medications with anti-inflammatory and healing effects. For severe and prolonged pain, we inject these drugs directly into the area of injury. The injection is performed with a very thin needle and is provided with local anesthesia.
Symptoms of arthritis and arthrosis
Basically, the signs of both diseases are similar:
- pain and crunching when moving;
- swelling of the joint area;
- limitation of amplitude and stiffness of movements;
- joint deformation;
- sensitivity to weather changes;
- exacerbation of symptoms due to overwork and hypothermia.
But there are some differences:
- signs of arthritis develop quickly, and arthrosis - gradually;
- with arthritis, the symptoms are more pronounced (for example, the pain with arthrosis is aching, and with arthritis it is sharp);
- arthritis, unlike arthrosis, may be accompanied by redness of the skin;
- with arthritis, signs of intoxication may occur: fever, headache, “ache”;
- A characteristic feature of arthrosis is the formation of “articular mice” - necrotic bone fragments penetrate into the joint cavity, which, falling between the articular surfaces, cause acute pain.
Diagnostics
Only an experienced doctor can determine the disease and the extent of damage, so contact SanMedExpert for help. To diagnose diseases, our specialists use modern equipment, techniques, extensive experience and accumulated knowledge.
If you suspect arthrosis or arthritis, the doctor will conduct a visual examination of the diseased joints, palpation, and ask you to talk about symptoms, previous diseases and injuries. Then you will be prescribed an X-ray examination, laboratory tests of blood and urine.
With arthrosis, blood counts are usually within normal limits. Whereas with arthritis, the patient exhibits an increased erythrocyte sedimentation rate and a high level of leukocytes, which indicates the development of an inflammatory process. An x-ray will not show changes in the joints due to arthritis, but in case of arthrosis, the doctor will identify such changes in the image. Also, with arthritis, the so-called rheumatoid factor will be increased.
In addition, for diagnosis we use special instrumental studies (ultrasound, arthrography, arthroscopy, myelography). The patient must be examined by a rheumatologist, traumatologist, and consult a dermatologist, infectious disease specialist, or phthisiatrician. Only based on the results of research and the opinions of highly specialized specialists can an accurate diagnosis be made and effective treatment prescribed.
Is it possible to solve the problem radically? What are the forecasts?
Osteoarthrosis (coxarthrosis, gonarthrosis, osteoarthrosis of other joints)
It is almost always possible to improve the patient’s condition - completely relieve pain or reduce it to an acceptable limit, increase joint mobility. Of course, if the joint is not destroyed and does not require surgical treatment. However, without supportive treatment, arthrosis can progress. To maintain the achieved treatment results for a long time, the following measures will be required:
- Gymnastics. Usually it is enough to do it 2-3 times a week for 15 minutes. Maintains mobility and proper biomechanics of joints, which protects them from further mechanical damage.
- Periodic preventive treatment (chondroprotectors, physiotherapy, manual therapy, massage). The frequency of preventive treatment is from 1 time every 2 years to 2-3 times a year, depending on the severity of arthrosis and the age of the patient.
- Follow the exercise regimen and balanced diet recommended by your doctor.
Inflammatory joint diseases (arthritis, polyarthritis, spondyloarthritis, ankylosing spondylitis, etc.)
It is almost always possible to extinguish the activity of joint inflammation, by greater or lesser measures, within a period of several days to 2-3 months. Pain goes away, mobility of joints and spine is restored. The most important task in these diseases is to avoid relapse of inflammatory activity. It would be honest for us to say that these diseases require long-term treatment, periodic medical monitoring and systematic prevention. And yet, inflammatory joint diseases recede with punctual implementation of the following measures:
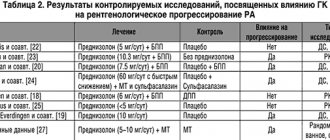
- Regular laboratory (2-4 times a year) and x-ray (1-2 times a year) monitoring of inflammation activity for many years. Allows you to notice in time a tendency towards an increase in the activity of inflammation of the joints or, conversely, a state of improvement when anti-inflammatory treatment can be canceled.
- Timely anti-inflammatory treatment based on the results of tests and radiography. Almost the only reliable way to maintain your ability to work. In addition to safe modern non-steroidal drugs, we use basic therapy with sulfasalazine.
- Gymnastics. Usually it is enough to do it 2-3 times a week for 15 minutes. Maintains mobility and proper biomechanics of joints, which protects them from mechanical damage and limited mobility.
- Periodic preventive treatment (chondroprotectors, physiotherapy, classes with a rehabilitation specialist, massage). The frequency of preventive treatment is 1-2 times a year.
- Follow the exercise regimen and balanced diet recommended by your doctor.
Periarthritis, bursitis, tendinitis
Treatment takes about 1-3 months. It is always possible to relieve pain and increase joint mobility; pain decreases already in the first week of treatment. In cases of advanced periarthritis (6 months or more without proper treatment), joint mobility is often limited by 10-20%. For 1-2 years, preventive treatment is highly desirable (chondroprotectors, physiotherapy, classes with a rehabilitation specialist, massage). The frequency of preventive treatment is 1-2 times a year.
Heel spur
Treatment takes from 1-2 weeks to 3 months; pain decreases already in the first week of treatment. In the future, it is very important to maintain correct foot biomechanics: wear soft orthopedic insoles, maintain a healthy spine (gymnastics, manual therapy, massage, swimming).
When should you resort to surgical treatment?
When the joint is unable to support and move (destroyed), we refer our patients for surgical treatment. Conservative treatment in such cases is an unjustified waste of the patient’s money and precious time. The fact is that an incompetent joint “relieves” the load when moving and relying on healthy joints and the spine. This is the path to arthrosis of other joints and herniated intervertebral discs.
Full or partial joint replacement is possible. Joint replacement surgeries have been performed for a long time; surgical and postoperative rehabilitation techniques have been developed and adapted for older people with age-related concomitant diseases.
How do we help our patients?
We strive to provide maximum help and support to our patients: 1. We use any treatment methods that can help our patients return to normal life and work. 2. We strive to save time and money for our patients, and at the same time provide high quality treatment. With your consent, you will be prescribed and performed any diagnostic or therapeutic procedure, expensive or cheap, necessary for a successful result. 3. We teach our patients, whenever possible, to independently maintain their health through exercise, proper nutrition and other preventive measures.
We are convinced that it is a mistake to isolate yourself in any one method of medication, manual therapy or physical therapy. Therefore, our doctors use modern medications, physiotherapy, 6 methods of manual therapy and various types of therapeutic exercises, combining them in the interests of their patients. The doctors of our center have been trained by leading world experts - professors Robert Wood, Johannes Vossgreen, Paul Rennie, L.F. Vasilyeva and others; have certificates from European medical associations and participate in international medical congresses.
We pay great attention to motor rehabilitation and restoration of patients' ability to work. Control of posture and movement has a very complex organization and is provided by the central nervous system, therefore, during the treatment process, we not only restore the mobility of the vertebrae and joints, but also, using special techniques, “show” the central nervous system deviations in its work and retrain it.