1.What is a muscle tear?
The skeletal muscles of our body weave around the bone frame, supporting it in the desired position and providing precise movements. Based on our internal feelings, we can always assess whether the load associated with a particular task is feasible. However, in a number of cases - in extreme cases, in emergency situations, when events develop at lightning speed and protective reflexes are triggered, the load exceeds the allocated resources. The muscles perform excessive work even to their own detriment and, as a result, get injured.
The main properties of our muscle fibers are elasticity when stretched and contractility when changing body position or performing any action. During sudden movements, when falling, jumping, a mismatch may occur in neighboring muscles. They contract simultaneously, whereas normally the contraction of a part of the muscle should be combined with the relaxation of neighboring fibers. This conflict leads to tissues receiving pathological stretching and ruptures.
A must read! Help with treatment and hospitalization!
Rupture (sprain)
Terminology
Torn, pulled, stretched, tore, tore - all these verbs are very often heard in relation to the so-called ligaments.
It seems that each of us intuitively understands what we are talking about: the aching pain persists for a long time, and we should take care of this place, not make sudden movements in the affected joint, and you can also bandage it tightly with an elastic bandage, and just in case, apply something “ from a sprain”... but it will still hurt for a while. A ligament, or ligament (the Latin word “ligamentum” comes from “ligare” - to bind) is an anatomical element that ensures the integrity of the joint. This means that the articular capsule and the head of the movable (rotating) bone are kept at a certain distance (or rather, in the optimal range of distances) and cannot move away from each other beyond a certain limit: they are mechanically “prevented” by the ligaments, protecting the joint according to the margin of safety from dislocation. Functionally, ligaments are divided into inhibitory, strengthening and guiding.
These connecting cords are formed by longitudinal fibrous connective tissue (which in this case lives up to its name like nowhere else) and contains two basic proteins for it - coarser, stronger, “scar” collagen and flexible elastic elastin. There is more collagen, but the presence of elastin still provides the ligaments with a certain extensibility, which in turn further increases the stress resistance of the joint, its ability to absorb and compensate for applied forces. The ligaments are attached to the mating bones through the periosteum (periosteum), growing with fibrous ends into this blood supply and innervating membrane of the bone. Blood arterioles and conductive nerves are located in the ligaments along the connective tissue fibers, which is responsible for the high pain reactivity of the ligaments in response to mechanical damage.
Since ligaments have some elasticity (albeit slight), stretching and contraction is a normal process for them. What we call a “sprain” in everyday speech, hissing and wincing in pain, is actually a microtear of the ligament fibers. Both macro-rupture and complete separation of the ligament along with a fragment of the periosteum are possible - in cases where the forces acting on the joint are so great that they exceed the by no means small margin of safety of the ligaments.
Micro- and macro-tears of the ligamentous apparatus are, if not the most common, then certainly one of the most common injuries received by a person. Obviously, the most active and loaded joints most often suffer: knee, ankle, wrist, shoulder, elbow, hip, etc.
2.What are the symptoms of a muscle tear?
Violation of the anatomical integrity of muscle fibers causes severe pain and an attempt to adopt a forced, gentle body position, in which the affected muscles are least stretched. Often the rupture causes convulsions that cannot be relieved for a long time. If the skin at the site of injury is not damaged, intense internal hemorrhage begins, which causes swelling and redness. The resulting hematoma may appear after some time in the form of an extensive bruise.
Motor activity in the affected area becomes impossible due to severe pain with any attempt to move. If the muscle bundle is completely torn, certain movements are simply impossible. With a partial rupture, the function is preserved, but the acute pain syndrome forces the victim to remain completely at rest.
Diagnosis of this injury is not difficult. The symptoms are obvious and pronounced. It may just be necessary to differentiate trauma from more severe disorders. If it is necessary to exclude a fracture, an x-ray examination is prescribed.
Visit our Traumatology and Orthopedics page
The knee joint and the role of the anterior cruciate ligament
The knee joint is not only one of the largest, but also one of the most complex joints in the human body. It is formed by the condyles (expanding ends) of the femur and tibia. Between them is the patella or kneecap, which covers the joint when it bends. The condyles of the bones are covered with smooth hyaline cartilage, making them easy to slide and, accordingly, move.
In addition, the knee joint is not congruent, that is, the bones that form it do not fit tightly together. The gaps formed between them are closed by special crescent-shaped cartilage layers - menisci. They not only act as a shock absorber, but also increase the stability of the knee joint. But the main task of ensuring the stability of this large joint lies with the group of ligaments represented by:
- anterior and posterior cruciate ligaments (ACL and PCL);
- tibial collateral ligament;
- fibular collateral ligament.
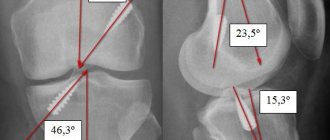
The anterior cruciate ligament (ACL) is located directly in the center of the knee joint and protects the lower leg from excessive anterior and inward movement. It is fixed at one end to the outer condyle of the femur, and at the other to the depression on the tibia, partially intertwined with the meniscus. The PCL is located perpendicular to the ACL, thus forming a cross, which is why they got their names.
On average, the length of the ACL is 3 cm and the width is 0.7–1.2 cm.
The anterior cruciate ligament is formed by tightly interwoven collagen fibers that are almost incapable of stretching. This causes a high risk of damage to it when too much load is applied, and subsequently the development of instability of the knee joint and an increased risk of arthrosis.
The ACL has a two-bundle structure, although some authors also identify a third bundle, called the intermediate one. Traditionally, there are 2 bundles (anterointernal and posteroexternal). When the knee joint is engaged during movement, they are in a complex interaction. It is thanks to this structure that the knee joint has an optimal level of stability at any angle of flexion. In this case, the anterior cruciate ligament is almost completely devoid of blood vessels, but has nerve endings.
Of all the ligaments of the knee joint, the ACL is the most commonly injured.
3. Treatment for muscle ruptures of varying degrees
Depending on the severity of the injury, the patient requires different amounts of medical care. The recovery period is also very individual. Muscle tears are classified according to two criteria:
- open or closed gap;
- full or partial.
First aid for muscle fiber injury is provided on the spot and includes:
- fixing the affected area in a position that ensures maximum approximation of the separated parts of the muscle;
- applying ice to stop bleeding;
- in case of an open rupture, it is necessary to treat the edges of the wound with antiseptic agents.
First aid measures may be sufficient for a partial rupture. In this case, further fusion of damaged tissue occurs under the condition of complete rest.
However, it is difficult for a non-specialist to assess the severity of the injury.
It is recommended to take the victim to the nearest emergency room for diagnosis and obtain qualified advice. The treatment plan based on the results of the examination may include:
- applying ice to the injury area according to a specific pattern;
- subsequent heat treatment;
- painkillers and anti-inflammatory drugs;
- first rest, and then physiotherapy aimed at development and recovery.
Muscle tears require 4 to 12 weeks to heal and recover. This injury is dangerous because the muscles can heal incorrectly and form a lifelong defect. If there is any suspicion that the rehabilitation process is being delayed or is not producing the desired result, you should contact a traumatologist.
The doctor will conduct intermediate studies and make adjustments to treatment tactics.
About our clinic Chistye Prudy metro station Medintercom page!
Treatment of ACL injuries
Treatment of anterior cruciate ligament injuries begins with the use of conservative methods, provided that there is no instability of the tibia in the knee joint and there are no other serious injuries, such as meniscal tears. Partial ruptures of the ACL, as a rule, do not cause the development of instability of the lower leg, since its fragment that has preserved its integrity is able to provide a sufficient level of stabilization of the joint.
Even complete tears do not always require surgical intervention, since the ACL can fuse with the posterior cruciate ligament over time and, in the absence of high loads, will provide a sufficient level of stability to the joint. However, with complete ruptures of the anterior cruciate ligament, especially in athletes and young patients, orthopedic surgeons cannot always rely on the high quality of fusion of the torn anterior cruciate ligament with the posterior ligament. Therefore, more often, in case of complete ruptures of the ACL, surgical intervention is still performed, except for children and adolescents with unclosed growth plates.
Also, surgery for ACL injuries is performed 5-6 weeks after the injury if there is no effect from the use of conservative methods, i.e. when:
- maintaining a feeling of “failure” in the knee;
- slipping or twisting of the shin;
- unruliness of the knee joint.
Immediately after a knee injury, you should not try to get up and move independently, as this can lead to even greater damage to the intra-articular structures. It is important to provide complete rest to the injured leg, apply cold and even try not to lean on it.
Conservative treatment
Thus, in the acute period with fresh injuries, they always start with conservative treatment. It is aimed at eliminating soft tissue swelling and pain. For these purposes, painkillers and cold compresses are prescribed for 2-3 days, and a puncture of the knee joint may be performed to remove blood. The leg is provided with complete rest, and subsequently the load is limited, allowing partial support on it and limiting the range of movements.
Immobilization of the knee joint can be achieved by applying a plaster splint or a special orthosis. The cast completely immobilizes the leg and makes movement in the knee impossible. The orthosis can either provide complete fixation or allow movements with a given amplitude. Adjustment is carried out using special hinges, but changing their position independently is unacceptable. Only an orthopedist can accurately assess the extent of ACL damage and set a safe range of motion.
In the absence of damage to other structures, the knee joint can be completely immobilized only during the acute period. Longer immobilization can only worsen the situation and lead to contracture, i.e. persistent limitation of knee mobility as a result of the formation of adhesions.
After the acute period is over, i.e. a few days after the injury, severe pain and hemarthrosis are eliminated, patients are prescribed specially selected exercises. But wearing an orthosis is not canceled! Their regular implementation will allow you to maintain the necessary muscle strength and gradually restore the range of motion in the knee joint.
Thus, the main method of conservative treatment of ACL injuries is exercise therapy. In the absence of additional damage, i.e., while maintaining the integrity of the menisci and other ligaments of the knee joint, the exercises prescribed by the doctor are performed with increasing amplitude and gradually increasing intensity. But it is strictly forbidden to perform any movements that can provoke instability of the knee joint. Therefore, it is important to strictly follow the exercise therapy program developed by the orthopedist and not perform exercises obtained from other sources on your own, although a properly adjusted orthosis will help to avoid such mistakes.
Strong thigh muscles help stabilize the knee joint, which is critical for ACL injuries.
3-5 weeks after the injury, the patient must be re-examined by an orthopedist. This time, the condition of the knee joint is assessed in a new way using the same diagnostic tests. If during this period there are no signs of instability, the treatment is considered successful and the doctor allows the orthosis to be removed, and also recommends gradually increasing the load during exercise therapy. At the same time, a decrease in the physical capabilities of the knee is absolutely normal. To fully restore its normal functioning, it will take several more weeks, during which it is important to systematically train the thigh muscles.
But if, 3-5 weeks after the injury, pain still persists and there are other signs of instability of the knee joint, including slipping, buckling of the lower leg, surgical intervention is indicated. Surgery will also be indicated in cases of development of chronic anteromedial instability, when after removal of the orthosis and apparent positive dynamics, the functions of the knee are not fully restored after several weeks.
Diagnostics in Germany
Diagnosing a pathology such as a skier's finger, that is, an acute rupture of a ligament, is not difficult. Based on the medical history, the doctor makes an assumption about the type of pathology and confirms the diagnosis by ordering an x-ray examination. In addition to ligament rupture, the x-ray will determine the presence or absence of damage to bone structures.
In case of old damage, when doubts arise about the diagnosis, an MRI of the affected hand is prescribed. In addition to instrumental studies, mandatory general clinical tests are carried out. Also, if surgery is necessary, examinations are prescribed to determine the general condition, such as chest radiography and ECG.
Surgical intervention
Surgical treatment of thumb ligament rupture in Germany is carried out in a minimally invasive way - using arthroscopy.
Indications for surgical treatment are:
- complete rupture of the ligament;
- old damage;
- ligament injury with separation of bone fragments;
- ineffectiveness of conservative therapy within 10-14 days.
During arthroscopic treatment, the specialist makes 2 incisions several millimeters long in the projection of the affected joint. This determines minimal trauma to healthy tissue, which means the absence of postoperative complications and relatively short rehabilitation.
A skier's toe in Germany is repaired by suturing the damaged ligament and restoring the integrity of the joint capsule. In addition, plastic surgery of bone structures is performed (if necessary) by applying fixing screws, plates and wires. Resorbable systems are often used, which are absorbed and excreted from the body over time.