A person’s daily life is unthinkable without physical activity, and therefore diseases that lead to a decrease in it are perceived as especially painful at any age. Osteoarthritis of the knee joint, also called gonarthrosis, occupies a special place among such diseases. The knee joint is located lower than most others, and therefore experiences the greatest load. It can occur not only when walking, but also when sitting in an uncomfortable position.
Over 75% of elderly people complain of symptoms associated with gonarthrosis. In advanced cases, even moving around the apartment becomes difficult—to get to the kitchen, the patient needs crutches or the help of loved ones. Osteoarthritis of the knee joints is one of the 10 main causes of disability in Russia. However, the disease can be prevented at a young age - in the early stages its development can be significantly slowed down, the main thing is to learn in time how to treat osteoarthritis of the knee joint.
Features of the development of osteoarthritis of the knee joint
Osteoarthritis of the knee joint
is a common pathology that belongs to the category of the most common diseases that have an extremely negative impact on a person’s quality of life.
Degenerative-dystrophic processes most clearly manifest themselves in the form of physical dysfunction of the legs, accompanied by severe pain. Depending on how much the pathological process progresses, further forecasts for the course of the disease are made.
One of the disappointing forecasts is paralysis of the lower limbs. The seriousness of the consequences of pathological processes necessitates seeking qualified medical help.
What is osteoarthritis?
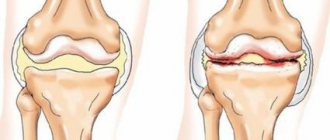
Stage 2 arthrosis is characterized by further thinning of the articular cartilage to 1.2-2mm (normal 2.5-2.7mm).
Joint deformation appears, the joint space narrows, subchondral sclerosis develops (inflammation of the bones forming the joint), single osteophytes and spines (bone growths) appear. Despite the progression of the disease, the course of the disease at this stage can be significantly slowed down. Today such technologies exist. It is possible to slow down destructive processes, relieve inflammation and symptoms, restore the functionality of the affected joint, and improve the patient’s quality of life.
What causes lead to knee arthrosis?
To identify the causes of arthrosis of the knee joint, it was necessary to conduct a large number of studies. Many years of examinations of patients and a thorough study of the clinical picture of the pathology allowed specialists to come to the conclusion that the influence of a number of negative factors is the root cause of the destruction of joint tissue, causing severe pain and inflammation.
Among the main reasons leading to degenerative-dystrophic processes, it is worth highlighting:
- previous injuries - a bruise, dislocation or fracture of the knee automatically classifies a person as a risk group and can cause the development of the disease. Damage to the joint presupposes its fixation, and long-term immobility is a direct path to the formation of arthrosis;
- strong physical activity - intense stress on the knees (especially in older people) leads to microtraumas, which also leads to the development of negative pathological processes;
- insufficiently strong ligamentous apparatus - abnormal joint mobility also negatively affects their condition, which manifests itself mainly in old age;
- excess body weight - extra pounds can cause irreparable damage to the knee joints, because the likelihood of meniscus injuries in this case is incredibly high. If a lot of weight is accompanied by varicose veins, then there is a high probability of developing severe forms of arthrosis of the joints of the lower extremities;
- metabolic disorders - a failure in the exchange of nutrients and elements in the body provokes the development of various kinds of diseases, which is caused by insufficient supply of various tissues, in particular bone and cartilage;
- increased levels of stress - worries and worries negatively affect not only people’s mood, but also the level of physical well-being.
Causes of knee pain due to osteoarthritis
The knee joint is very strong, and daily supports the weight of the human body, and also endures enormous loads when carrying heavy loads and loads. It can be damaged by a strong blow, but even in the absence of a fracture or dislocation, there is a possibility of long-term pain that increases over time. This is caused by microdamage to the cartilage tissue, which acts as a protective shell for the joint. Over time, this small crack begins to enlarge and grow, causing stronger sensations of discomfort, hindering movement, and over time does not even allow the person to move, leaning on the sore leg.
Characteristic symptoms of arthrosis of the knee joint
The symptomatic manifestation of the disease allows timely tracking of the onset and development of pathological processes, which gives each patient the opportunity to recover.
Before determining who to turn to for help and how to treat arthrosis of the knee joint, it is important to become familiar with the symptoms of the disease.
Only a specialist competent in this matter can identify the presence and confirm the diagnosis by prescribing treatment for knee arthrosis. However, every patient should know the main symptoms of knee osteoarthritis, among which are usually identified:
- pain - discomfort that gradually develops into painful sensations does not appear immediately. Their slight manifestation in the knees can bother a person for many years, but at some point they may become stronger, and they will not stop in a calm state;
- crunch – “clicks” when flexing/extending a joint are an alarm bell, which manifests itself already in the second and third stages of the disease;
- synovitis is an inflammation of the joint membrane, in which fluid accumulates, which leads to local swelling;
- deformation is a characteristic feature that appears in the last stages of the disease, accompanied by pronounced inflammation and swelling.
medicines
medications
The key point in treating a disease is eliminating the factor that provokes its development. If the reason lies in excess weight, you need to start losing it under the supervision of specialists. If the reason is excessive stress on the legs, you need to reduce them. If the disease develops due to hormonal imbalance, it is necessary to regulate the indicators that affect this.
It is important to understand that selecting suitable medications is the task of a qualified specialist. Only under the supervision of an experienced doctor can success in treatment be achieved.
To understand what stage of the disease we are talking about in the current period of time, contact our clinic for an initial consultation. The doctor will examine your knee, take pictures and answer all your questions. Only after the necessary diagnostic measures will it be possible to draw up a detailed treatment plan.
Self-treatment with folk remedies is not the main thing and is applicable only after consultation with a specialist.
Diagnosis of arthrosis of the knee joint
Diagnosis and treatment of arthrosis of the knee joint is carried out by an orthopedist or rheumatologist. If you wish to undergo a diagnostic examination, each patient can contact a therapist, who will give a referral to a specialist or independently take a voucher to one of them.
The main diagnostic tool of specialists is, of course, an X-ray machine. Thanks to the image taken, you can track not only the presence of pathology, but also the degree of its development.
It is important to note that x-rays can exclude the possibility of the presence of other diseases of the musculoskeletal system.
X-ray examination opens up the opportunity for a specialist to:
- track the narrowing of the joint space;
- detect compaction in joint tissues.
The combination of clinical symptoms and information obtained from the image provides high-quality diagnosis and diagnosis, with the determination of further treatment for osteoarthritis of the knee joint.
Prevention and prognosis
The prognostic picture of stage 2 osteoarthritis is unclear, as it depends on many factors, including the thoroughness of compliance with medical prescriptions and the speed of development of the disease. In most cases, the prognosis is conditionally unfavorable, since there are no methods of completely curing the disease.
According to many medical studies, there are no reliable methods for preventing the disease. It is important to maintain a healthy lifestyle, do not lift heavy objects and avoid injury or hypothermia. Also, compliance with these recommendations is not a 100% guarantee of avoiding osteoarthritis in the future.
Degrees of osteoarthritis of the knee joint
Modern medicine divides knee arthrosis into several degrees, in accordance with the nature of the development of pathological processes.
To begin with, it is worth noting that according to observations, the disease can have a different nature:
- unilateral (right-sided/left-sided);
- bilateral.
In addition, the pathological process has three stages of development, each of which has its own clinical picture.
1st degree arthrosis of the knee joint
The initial stage of the development of pathology, the successful diagnosis of which is an incredible success not only for the patient, but also for the attending physician.
The peculiarity of the degree of development of arthrosis at this stage is the absence of clinical signs and clear symptoms. Identification of the disease can be carried out during medical examination or during the study of another disease.
Evidence of grade 1 arthrosis of the knee joint may be:
- local discomfort in the knee area during long walking;
- mild pain that disappears with rest.
It is important to note the fact that pain can be felt in one or both joints of the lower extremities.
It is interesting to note that left-sided gonarthrosis is often diagnosed in left-handed people, while right-sided gonarthrosis is typical for people involved in various sports.
2nd degree arthrosis of the knee joint
Symptoms of the second degree of development of pathology are accompanied by an expansion of signs, which are usually included:
- pronounced pain syndrome;
- stiffness and severe discomfort in the knee joint;
- atrophy of the muscles located near the knee joint, which is caused by tissue damage;
- increased pain;
- visually noticeable deformation of the joint;
- limitation of mobility.
Expanding the symptoms simplifies the diagnostic process. Changes characteristic of grade 2 arthrosis of the knee joint are easy to track during palpation. When undergoing a clinical examination, a specialist can easily detect an abnormal formation in the knee area.
3rd degree arthrosis of the knee joint
It is almost impossible not to notice the third degree pathology, because the patient faces constant pain. In addition, the progress of the disease reaches a critical point, which is manifested by severe deformation of the joint, in which the limb completely loses the ability to flex/extend.
The lack of proper treatment leads to complete destruction of the cartilage and, as a consequence, the development of ankylosis (fusion of articular bones).
The only solution for the final stage of development of the disease is an expensive surgical intervention, involving the removal of remnants of cartilage tissue or joint replacement.
Osteoarthritis: diagnostic and treatment algorithms
Algorithms for diagnosis and treatment for rheumatic diseases
Doctor of Medical Sciences, Prof.
A.L.Vertkin, Ph.D., Associate Professor A.V.Nosova, K.S.Artamonova Abstract:
In recent years, there has been a tendency to change the clinical concept of osteoarthritis (OA). For a very long time, this disease was considered as an “age-related pathology” and the outcome of a long-term pathological process. However, now many experts are inclined to the need to identify an early, pre-radiological stage of OA, when adequate therapy can not only stop the progression, but also reverse the development of structural changes in the joint. This review examines a number of pathogenetic and clinical aspects of the early stage of OA, which are important for timely diagnosis and selection of pathogenetic therapy. Some therapeutic approaches are considered, both “classical” and the recently actively discussed methods of using platelet-rich plasma and autologous chondrocyte transplantation.
Keyword:
osteoarthritis, early osteoarthritis, pathogenesis, treatment, platelet-rich plasma, autologous chondrocyte transplantation.
Osteoarthritis
- a chronic disease that causes damage to cartilage and surrounding tissues. The disease is characterized by pain, stiffness and loss of function.
The problem of osteoarthritis (OA) is a serious challenge to medical science and society; It is the most common chronic joint disease, causing severe suffering and disability for hundreds of millions of people worldwide. As of 2010, knee OA was diagnosed in 250 million people on our planet.
Osteoarthritis is divided into:
- primary;
- secondary.
The cause of primary (or idiopathic) osteoarthritis is unknown (as is the case in the vast majority of cases). Primary osteoarthritis can affect only certain joints, such as the knee, or many joints.
Secondary osteoarthritis is caused by another disease or disorder, such as:
- infection;
- a malformation of the joint, which is detected at birth;
- injury;
- metabolic disorders, such as excess iron in the body (hemochromatosis) or excess copper in the liver (Wilson's disease);
- a disease that affects the cartilage of the joint, such as rheumatoid arthritis or gout.
Pathogenesis of osteoarthritis: In recent years, a new understanding of the pathogenesis of OA has been formed. First of all, this concerns changing ideas about the significance of inflammation in this disease. At present, there is no longer any doubt that it is chronic low-intensity (“lowgrade”) inflammation that acts as the most important factor in the development and progression of OA. Elements of the inflammatory process, which are manifested by the activity of “resident” macrophage cells and the local synthesis of proteolytic enzymes, such as MMP, are a natural adaptive mechanism necessary for the normal functioning of living tissue. All joint structures that experience daily static and dynamic load (“mechanical stress”) are gradually destroyed, and this process involves both highly specialized cells, for example, chondrocytes, osteocytes and synovial fibroblasts, and elements of the intercellular matrix (ICM). It is obvious that the gradual “wear and tear” of biological structures must be compensated by the natural mechanism of repair and remodeling. But restoration processes can proceed effectively only against a “clean background”: dead cellular elements and “fragments” of MCM macromolecules must be removed, which, in fact, is the goal of local physiological inflammatory activity.
Which joints are affected by the disease?
The following joints are most susceptible to the development of the disease:
- Knee;
- Hip;
- Intervertebral joints (cervical and lumbar regions);
- Brachial;
- Elbow;
- Small finger joints.
Symptoms
Typically, symptoms of osteoarthritis develop gradually and initially affect only one or a few joints. First of all, the joints of the fingers, the base of the thumb, the neck, lower back, big toes, hip and knee joints are affected.
Clinical picture and diagnosis of osteoarthritis
Clinical symptoms:
- pain in the joints and surrounding muscles;
- deconfiguration of joints (increase in size, anatomical deformations);
- decreased functionality of joints (inability to perform physiological range of motion in a joint);
- starting pain (a short-term episode of intense joint pain after a period of rest);
- decrease in the patient’s activity, up to immobilization;
- amyotrophy.
The course of OA in different patients is very variable, although radiological changes, as a rule, progress. In some cases, patients' condition remains stable for many years. However, in the vast majority of cases, only adequate pathogenetic therapy helps stabilize the process and prevent further progression of the disease. To determine the radiological stage of OA of the knee and hip joints, the classification of I. Kellgren and I. Lawrens (1957) is used, which is shown below in a modified form (Table 3).
Alarm symptoms (red flags) for joint pain that require a differential diagnosis:
- Symmetrical polyarthritis (possible collagenosis).
- Monoarthritis (possible history of joint injury, which requires consultation with an orthopedist).
- Prolonged morning stiffness (more than 30 minutes). Characterized by the inability to move the joints, especially the joints of the hands and feet (collagenosis).
- Joint pain occurred after significant stress: injury, hypothermia, surgery, etc. (possible collagenosis).
- Joint pain occurred after an infectious disease (possible infectious arthritis).
- Joint pain in young men who abuse protein shakes in fitness centers (possible gout).
- Joint pain in patients with connective tissue dysplasia (consultation with an orthopedist is necessary to select orthopedic devices that reduce the load on the joint).
- Joint pain in patients with thyroid pathology or in patients with diabetes (consultation with an endocrinologist and emphasis on the neuropathic component of pain is necessary).
- Failure of many examinations, muscle groups involved, muscle soreness, acute phase proteins in tests (possible polymyalgia rheumatica).
- Joint pain in asthenic women with a history of frequent diseases in childhood (you need to think about infectious arthritis: Epstein-Barr, Reiter's disease, etc.).
Associated clinical syndromes:
- depression;
- sleep disturbance;
- decreased cognitive function;
- hyperuricemia.
Osteoarthritis
Pain, often described as deep, is the first symptom. In weight-bearing joints, pain is typically worsened by activities that place weight on the legs (such as standing). Some patients may experience stiffness in the joint after sleep or inactivity, but the stiffness usually goes away within 30 minutes, especially with movement of the joint.
As new symptoms appear, freedom of movement in the joint may be further limited, making it impossible to fully flex or extend it. Due to the proliferation of bone and other tissues, an increase in the size of the joint is possible. Changes in the surface of the cartilage lead to the fact that the joints can creak, grind and crackle when moving, and pain appears.
Bone growths are usually observed in the joints located closer to the tips of the fingers (Heberden's nodes) or their middle part (Bouchard's nodes).
In some joints (such as the knee), the ligaments that surround and support the joint become so stretched that the joint becomes unstable. Alternatively, there may be stiffness in the hip or knee joint, with decreased range of motion. Touching or moving the joint (especially while standing, climbing stairs, or walking) may cause severe pain.
Osteoarthritis often affects the spine. The most common symptom is back pain. Usually, when the discs or joints of the spine are injured, there is only minor pain and stiffness. However, with osteoarthritis of the neck or lower back, you may experience numbness, pain, and weakness in an arm or leg if bone overgrowth puts pressure on nerves. The growth of bone tissue is possible in the lumen of the spinal canal in the lower back (lumbar spinal stenosis), it compresses the nerves leading to the legs where they exit the canal. Such compression can cause pain in the legs when walking, which leads to false suspicions of impaired blood supply to the legs (intermittent claudication). In rare cases, bone growths can cause compression of the esophagus, making swallowing difficult.
Osteoarthritis can be stable over many years or progress rapidly, but in most cases there is a slow progression after the onset of symptoms. For many patients, the disease leads to varying degrees of disability.
Doctors should evaluate patients whose joints are red, hot, and swollen because these symptoms are usually not caused by osteoarthritis and may be caused by infection or gout.
Diagnostics
- X-ray examination
Doctors diagnose osteoarthritis based on characteristic symptoms, results of a physical examination, certain blood tests, and X-ray appearance of the joints (such as enlarged bones and narrowing of the joint cavity). However, x-rays are not always indicative of early diagnosis of osteoarthritis, since they do not detect changes in cartilage tissue that appear first. Also, changes on x-rays often do not completely correspond to the patient's symptoms. For example, an X-ray of a patient with severe symptoms may show only minor changes, or a X-ray of a patient with few or no symptoms may show significant changes.
Magnetic resonance imaging (MRI) can detect changes in cartilage tissue in the early stages, but is rarely needed for diagnosis.
Blood tests do not diagnose osteoarthritis, although some may be helpful in diagnosing other diseases (such as rheumatoid arthritis).
If a joint is swollen, doctors may numb the area with an anesthetic injection and then insert a needle into the joint cavity to take a sample of synovial fluid. A sample is taken for analysis to differentiate between osteoarthritis and other joint diseases such as infections and gout.
Treatment:
- Physical modalities including physical therapy and occupational therapy.
- Medications.
- Surgical intervention.
The main goals of treatment for osteoarthritis include:
- anesthesia;
- maintaining joint flexibility;
- optimization of joint functions and functions of the whole body.
The achievement of such goals is primarily facilitated by physical activities, including exercises to develop strength, flexibility and endurance, as well as rehabilitation (physical therapy and physiotherapy). Patients are taught ways to change their daily activities to make life easier with osteoarthritis. Additional treatments include medications, surgery (for some patients), and new treatments.
Physical activities
Appropriate exercises—including stretching, strengthening, and posture exercises—can help maintain healthy cartilage, increase range of motion in a joint, and, most importantly, strengthen nearby muscles to better absorb shock. Exercise can sometimes slow the worsening of osteoarthritis in the hip and knee. Doctors recommend doing exercises in water (for example, in a swimming pool), since water can reduce the stress on the joint.
Stretching exercises should be performed daily.
Exercises should be interspersed with periods of rest of painful joints lasting a few minutes (every 4-6 hours during the day), but immobilizing the joint is more likely to worsen the disease than to alleviate the patient's condition.
Using chairs, armchairs, mattresses, or car seats that are too soft can aggravate symptoms.
Patients sitting in a chair should not place pillows under their knees as this can strain the knee and hip muscles. (This recommendation is contrary to the recommendation for placing a pillow between the knees in patients with low back pain and sciatica. In these patients, using a pillow reduces stress on the lower back and hip.)
It is often recommended to move car seats forward, sit in straight-backed chairs with fairly high seats (such as kitchen or dining room chairs), sleep on firm mattresses, use boards in the bed (available from many wood shops), and wear shoes with foot support or sports shoes.
Toilet seat lift devices can make getting up easier for patients with painful osteoarthritis of the knees or hips, especially if they have muscle weakness.
- Patients with back osteoarthritis should not place pillows under their knees while sitting in a chair, as this can cause strain on the knee and hip muscles.
Certain exercises sometimes help with osteoarthritis of the spine; If pain is severe, back support may be required. Exercise should include both exercises to improve muscle strength and low-intensity aerobic exercise (such as walking, swimming, and cycling). If possible, patients should maintain a normal daily schedule and continue to do their usual activities, such as hobbies or going to work. However, physical activity must be adjusted to avoid bending and exacerbating osteoarthritis pain.
Other additional measures may also relieve pain and help people live with osteoarthritis. They include the following:
- Exercise therapy, often combined with heat therapy such as heating pads, as well as physical therapy.
- Range of motion exercises done gently in warm water are beneficial because heat improves muscle function, reducing stiffness and muscle spasms.
- Thermotherapy. For example, apply heating pads or wet and warm compresses to the affected joints. (To avoid burns, patients should be careful not to use a heating pad that is too hot or leave it on for too long.)
- To relieve pain when the condition of one joint temporarily worsens, you can also apply cold.
- Shoe inserts (orthopedic), support or athletic shoes can help relieve pain when walking.
- If necessary, use special equipment (eg, canes, crutches, walkers, neck braces, or knee pads to protect the knees from excessive stress; or a bath chair to avoid excessive strain during bathing).
- Losing weight can relieve some of the pressure on your joints.
- Electrical stimulation. For example, transcutaneous electrical nerve stimulation (TENS) may help relieve pain.
- Impact on acupuncture points leads to the release of various chemical messengers (neurotransmitters) by the brain, which act as natural anesthetics, which can help in this situation.
- Massage performed by a qualified therapist and deep heating with diathermy or ultrasound examination are helpful.
Medications
Medications are prescribed in addition to exercise and physical therapy. Medicines, which can be used together or separately, do not themselves affect the course of osteoarthritis. They are used to relieve symptoms and therefore make normal daily activities easier.
To relieve mild to moderate pain, taking simple painkillers (analgesics) such as paracetamol before performing activities that cause discomfort, or taking them regularly to relieve persistent discomfort in the joint area, may be sufficient. Although side effects are rare, patients should not take more paracetamol than recommended, especially if they have liver disease. When taking paracetamol, it is not recommended to take various over-the-counter medications containing acetaminophen at the same time.
However, in some cases, patients require stronger analgesics, such as tramadol, or, in rare cases, opioid medications.
Alternatively, nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce pain and swelling. NSAIDs relieve joint pain and inflammation and may be used in conjunction with other analgesics. NSAIDs are also available in gel and cream form to be rubbed onto the skin (eg, diclofenac 1% gel) over the joints of the hand and knee to relieve symptoms. However, when it comes to long-term use, the risk of serious side effects is higher when taking NSAIDs than when taking paracetamol.
Sometimes it becomes necessary to use other types of painkillers. For example, a cream with cayenne pepper extract (with capsaicin as the active ingredient) can be applied directly to the skin over the joint. Your doctor may also recommend lidocaine patches for pain relief, but there is no evidence that these patches are effective. Duloxetine, an oral antidepressant, reduces pain caused by osteoarthritis.
Muscle relaxants (usually in low doses) can sometimes relieve pain caused by tight muscles trying to support joints affected by osteoarthritis. However, in older people they cause more side effects than benefits.
If there is sudden inflammation, swelling and pain in the joint, it may be necessary to remove most of the joint fluid and then inject a special dosage form of cortisone into the joint cavity. In some patients, such treatment can achieve temporary pain relief and increased joint mobility.
A series of 1 to 5 injections of hyaluronate (a substance similar to normal synovial fluid) into the knee cavity each week provides long-term pain relief in some patients. Such injections should be carried out no more often than once every 6 months. Hyaluronate injections are less effective in patients with severe osteoarthritis and do not slow the progression of arthritis.
Several dietary supplements (eg, glucosamine sulfate and chondroitin sulfate) have been studied for possible benefit in the treatment of osteoarthritis. To date, results have been mixed, and the potential benefits of glucosamine sulfate and chondroitin sulfate in the treatment of pain are not clear, and these drugs did not appear to have an effect on the progression of joint destruction. There is no evidence of effectiveness for any other dietary supplement.
Surgical intervention
Surgery can achieve results when other treatment methods are unable to relieve pain or improve function. It is possible to replace some joints with prosthetics, most often the hip and knee, i.e. replacement with an artificial joint. Joint replacement, especially the hip replacement, is usually very effective: in almost all cases it is possible to improve range of motion and function, as well as significantly reduce pain. Thus, if pain cannot be controlled and function is limited, joint replacement should be considered. Because the artificial joint does not last forever, the procedure is often delayed when treating very young people to minimize the need for revision prosthetics. If all other treatments have failed, surgery may be performed to relieve symptoms of osteoarthritis in the back or neck, especially when nerves are compressed. The benefit of limited arthroscopic surgical procedures for knee osteoarthritis, such as meniscal repair or knee ligament reconstruction, is controversial.
To heal small cartilage defects in young patients with osteoarthritis (often caused by trauma), a number of techniques are used to restore the cells within the cartilage. However, such methods are not effective for massive cartilage damage, which is usually observed in older people.
OA outcomes:
- long pain-free periods with an optimal level of patient activity (target outcome);
- aseptic necrosis;
- endoprosthetics.
Recommendations for outpatient clinicians
During the initial examination of a patient with OA, the following facts must be assessed and reflected in the clinical documentation:
- indicate painful joints;
- determine the intensity of pain (using a visual analogue scale [VAS]), duration, presence of starting pain (in the morning, after a period of rest);
- obtain information about the relief of previous pain relapses;
- examine and palpate the joint to assess the presence of: joint deformation, effusion into the joint cavity, bone growths, including Heberden and/or Bouchard's nodes, pain on palpation, atrophy of the periarticular muscles;
- study movements in the joint (limited mobility, presence of crepitus during movement) and assess the impact of damage to the joint(s) on the performance of everyday functions;
- assess gait;
- identify sleep disturbances and depression caused by pain.
Laboratory tests are not needed to diagnose OA. However, a mandatory study of uric acid concentration should be carried out to personalize the treatment strategy taking into account microcrystalline stress.
Radiographs reveal narrowing of the joint spaces, osteosclerosis, and marginal osteophytes.
Ultrasound examination is performed to detect synovitis.
Radiological changes alone are not sufficient for a clinical diagnosis of OA (clinical symptoms must be present).
For the purpose of differential diagnosis, the following studies are carried out: complete blood count (ESR, anemia in collagenosis, leukocytosis in reactive arthritis), uric acid, creatinine, C-reactive protein, antibodies to citrulline peptide, antibodies to double-stranded DNA, rheumatoid factor, general urine test . In order to personalize pharmacotherapy, the patient’s comorbid status should be clarified: biochemical parameters of lipid and carbohydrate metabolism, aminotransferases.
Indications for consultation with a rheumatologist upon initial visit to the clinic:
- long-term (more than a month) existing synovitis;
- suspicion of inflammatory joint diseases or systemic connective tissue diseases (prolonged joint swelling, accelerated ESR, high level of C-reactive protein).
Bibliography:
- Karateev A.E., Lila A.M. Osteoarthritis: modern clinical concept and some promising therapeutic approaches. Scientific and practical rheumatology. 2018;56(1):70-81. doi.org/10.14412/1995-4484-2018-70-81
- Alekseeva LI, Sharapova EP, Kashevarova NG, Pyanykh SE. New opportunities in the treatment of osteoarthritis. Directory of a polyclinic doctor. 2015;
- Balabanova RM, Erdes ShF. Prevalence of rheumatic diseases in Russia in 2012–2013. Scientific and practical rheumatology. 2015;
- Folomeeva OM, Galushko EA, Erdes ShF. Prevalence of rheumatic diseases in adult populations of Russia and the USA. Scientific and practical rheumatology. 2008;
- RUSSIAN SCIENTIFIC MEDICAL SOCIETY OF THERAPISTS. MANAGEMENT OF PATIENTS WITH OSTEOARTHRITIS AND COMORBIDITY IN GENERAL MEDICAL PRACTICE. CLINICAL GUIDELINES, Moscow, 2021 2 MANAGEMENT OF PATIENTS WITH OSTEOARTHRITIS AND COMORBIDITY IN GENERAL MEDICAL PRACTICE. COMPILERS: Professor A.V. Naumov, professor L.I. Alekseeva
How to treat arthrosis of the knee joint?
The level of modern medicine is at a fairly high level, which ensures successful treatment of various types of diseases. Osteoarthritis of the knees is no exception.
Today, there are a large number of methods for treating arthrosis of the knee joint.
At the initial stages of pathology development, predominantly conservative treatment methods are used. Conservative therapy includes:
- physiotherapeutic procedures;
- physical therapy (physical therapy);
- visiting various massages.
Progressive methods of treating osteoarthritis of the knee joint are also actively used. Among the modern effective ways to combat dangerous pathologies are the following:
- Ozone therapy is a local effect of ozone on the affected joint tissues. Helps reduce pain and stop inflammatory processes. Improves blood circulation in the problem area;
- kinesitherapy is a set of exercises for arthrosis of the knee joint, aimed at increasing its mobility and increasing blood flow.
Treatment of knee arthrosis with physiotherapy
Physiotherapy is one of the most popular methods of treating knee osteoarthritis.
Methods of physical influence, subject to a certain number of conditions, have the most positive effect on the area of localization of pathologies of various types.
Physiotherapy includes procedures such as:
- electrophoresis;
- ultraphonophoresis;
- irradiation with laser/infrared radiation;
- pulsed magnetic therapy.
The effectiveness of the procedures is individual and depends on the quality of the patient’s basic treatment plan.
Massage as a treatment for osteoarthritis of the knee joint
Massage is a useful addition to the treatment strategy for knee arthrosis.
Most experts around the world are of the opinion that massage is a mandatory component of the treatment of symptoms of arthrosis of the knee joint, which has a beneficial effect on metabolic processes and helps speed up recovery.
Knee massage can be performed both at home and within the walls of a hospital. The main thing during massage is preliminary high-quality warming up of the joint and compliance with the optimal duration of the process (from 10-15 minutes).
Treatment of osteoarthritis of the knee joint with massage should include techniques such as stroking, rubbing and kneading.
Gymnastics and exercise therapy for arthrosis of the knee joint
Exercises for arthrosis of the knee joint are an effective way to eliminate unpleasant symptoms and treat the disease.
The process of treating knee arthrosis is a rather complex and lengthy process, and physical therapy is an excellent assistant in achieving the desired result.
The type of exercise therapy and exercises for arthrosis of the knee joint are selected by a specialist individually, depending on the degree of development of the pathology and the general state of the patient’s physical fitness.
The main principle of gymnastics for arthrosis of the knee joint sounds like this: no increased loads on the affected joint, only rational, calm actions.
Non-drug therapy
During the period of remission, the patient should take care of his health in order to delay the risk of re-exacerbation as long as possible. In order to avoid loss of range of motion in case of grade 2 osteoarthritis of joints, it is necessary to do special exercises. If there is severe stiffness in the knees, it is better to do gymnastics while lying on your back. To give an adequate assessment of regularly performed physical exercise, you need to monitor the range of motion in the joints over time. If there is no deterioration and stiffness goes away, then rehabilitation is effective. If the joint continues to lose mobility, then the restoration method should be reconsidered.
Electrophoresis for osteoarthritis
Physiotherapeutic procedures are also a good rehabilitation method. Physiotherapy can only be performed if there is no acute inflammatory process in the joints due to osteoarthritis. One of the most effective options for such treatment is electrophoresis. The essence of the procedure is to apply the drug to the affected area followed by exposure to electromagnetic radiation of a certain frequency. With a course of treatment, stiffness and chronic discomfort disappear.
Massage is the best way to normalize blood circulation in the area of the affected joint. Recent medical research indicates that massage is most effective for grade 2 osteoarthritis of the axial joints. Competent work by a specialist will help relax tense muscles, relieve general tension, and improve blood circulation. During exacerbation, massage is contraindicated.
Drugs for the treatment of osteoarthritis of the knee joint
Drug treatment for arthrosis of the knee joint is used to relieve symptoms such as pain and swelling, as well as to activate regenerative processes.
Drugs for the treatment of arthrosis of the knee joint can come in different forms (ointments/gels, tablets or injections, patches).
IMPORTANT! Any medication must be prescribed by a specialist as part of an existing treatment plan developed taking into account the symptoms of knee arthrosis.
Self-medication is unacceptable and can lead to extremely negative consequences, in particular, paralysis of the lower limbs and disability.
Painkillers for arthrosis of the knee joint
Used to eliminate symptoms of arthrosis of the knee joint.
Painkillers play an important role in the treatment of arthrosis of the knee joint, because their use improves the patient’s well-being and gives him the opportunity to get a good night’s rest.
Relief of pain is achieved through the action of active substances. The most effective tablets for pain in arthrosis of the knee joint are considered to be “Ketanol” and “Nimesulide”.
Antispasmodics for osteoarthritis of the knee
Prescribed as active assistance. A key area of focus is the fight against spasms.
The active substances included in the preparations help relax the muscle frame and provide pain relief.
Among the frequently prescribed ones, it is worth highlighting Mydocalm.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Treatment of arthrosis of the knee joint with drugs of this type not only eliminates pain, but also slows down and completely eliminates the progress of pathological processes.
Regular use of medications allows you to observe a constant concentration of active components, which guarantees a positive effect.
Artradol is considered to be the most effective NSAID.
Chondroprotectors for arthrosis of the knee joint
The main assistants in the treatment of arthrosis of the knee joint are chonroprotectors.
The active effect of chondroprotectors for arthrosis of the knee joint is aimed at restoring motor ability, which is due to the microelements included in the composition, which are an integral component in the process of building cartilage tissue.
The peculiarity of the principle of action of drugs involves a rather long, but at the same time effective process of getting rid of osteoarthritis of the knee joint.
Among the most effective and affordable drugs, it is worth highlighting Artracam, Structum and Chondroxide.
Diet and general nutritional recommendations for arthrosis of the knee joint
A diet for arthrosis of the knee joint is necessary for patients with excess body weight. A low calorie diet and a wealth of nutrients will ensure weight loss and accelerate the recovery process of affected joints.
Nutrition for arthrosis of the knee joint should first of all be balanced. The daily diet should contain dishes enriched with beneficial vitamins and microelements necessary for the regeneration of joint tissues and maintaining the balance of the entire body.
It is recommended to give up not only bad habits (alcohol abuse and smoking), but also such dishes as:
- store-bought semi-finished products;
- fatty, spicy and overly salty foods;
- sweet carbonated drinks.
For convenience and competent planning of the diet, when treating knee arthrosis, it is recommended to keep a food diary, which disciplines and helps facilitate the process of restructuring the usual lifestyle.