The stoller method for diagnosing and classifying meniscal injuries is a modern method based on MRI of the knee joint. New and still expensive, it allows you to obtain maximum information about changes in cartilage tissue and select treatment that will be most effective in a particular case.
Damage to the meniscus can be traumatic or degenerative in nature. Both damages are determined accurately by stoller. Depending on the degree of injury, the patient will be prescribed conservative or surgical treatment. Other methods of detecting pathology cannot accurately reflect the level of cartilage damage.
Causes of meniscus damage according to Stoller
The causes of damage vary. Degenerative meniscus defects are most often observed in older people, in whom the problem appears due to disorders in the knee joint. Also, degenerative changes are caused by the following reasons:
- rheumatism;
- gout;
- chronic microtrauma of the knee - observed when a person constantly overloads the joint, which as a result does not have time to fully recover and gradually begins to collapse.
Traumatic injury according to Stoller occurs much more often. It occurs from a direct blow to the knee area or against the background of significant unnatural loads. Such dangerous impacts include: prolonged walking on toes, high jumping and landing on a hard surface, forced knee extension, or sudden movement of the leg after it has been in one position for a long time.
Regardless of what caused the disease, it is necessary to carry out a full diagnosis, classify the damage and undergo full treatment. At the Sinai Clinic, patients are given the opportunity to diagnose and classify meniscus lesions according to Stoller at the most favorable price for them.
Conservative therapy
Once a medial meniscus tear has been diagnosed, treatment without surgery is prescribed only on the basis of certain criteria, which include the location, characteristics and severity of the damage. The medical specialist must take into account the cause of the pathological condition.
It is usually possible to prescribe conservative measures if small changes have been identified that do not extend beyond the surface of the cartilage. An incomplete meniscal tear can be treated without surgery using medications, physical therapy, and rehabilitation measures. During treatment, the knee is provided with functional rest, which is achieved by immobilization (immobilization) using tight bandages or a plaster splint.
Types of meniscal tears according to Stoller
Meniscal tears are classified by location and shape. Determining these indicators is very important for proper treatment of pathology. Injuries vary by location:
- anterior horn;
- bodies;
- posterior horn.
Depending on the form of damage, the classification is as follows:
- horizontal gap - observed in the case of cystic degeneration;
- oblique radical or longitudinal - occurs on the border of the posterior third of the cartilage and the middle;
- combined - occurs in the posterior horn.
Depending on the damage, the location of the source of the main pain changes somewhat, as well as the position of the leg in which it intensifies.
How to forget about joint pain forever?
Have you ever experienced unbearable joint pain or constant back pain? Judging by the fact that you are reading this article, you are already familiar with them personally. And, of course, you know firsthand what it is:
- constant aching and sharp pain;
- inability to move comfortably and easily;
- constant tension in the back muscles;
- unpleasant crunching and clicking in the joints;
- sharp shooting in the spine or causeless pain in the joints;
- inability to sit in one position for a long time.
Now answer the question: are you satisfied with this? Can such pain be tolerated? How much money have you already spent on ineffective treatment? That's right - it's time to end this! Do you agree? That is why we decided to publish an exclusive interview in which the secrets of getting rid of joint and back pain are revealed. Read more.
What is Stoller classification
The technique was developed by Doctor of Medical Sciences, Professor David Stoller, who is the director of the National Center for Visualization of Musculoskeletal System Structures in Orthopedics in the USA. The accuracy of the study and the possibility of layer-by-layer scanning of tissues, as well as visualization of affected tissue areas and joints, have increased significantly with the advent of MRI technology. The method proposed by Stoller is based on the fact that during scanning a signal of increased intensity appears, indicating the presence of degenerative changes in the area that occur when the meniscus is damaged. The professor has developed a system that uses criteria for the intensity of the received signal, as well as the area of its localization and propagation.
When classifying a lesion, indicators of criteria for the severity of pathology and its severity are taken into account. The classification is based on the intensity of the signal: the higher it is, the more serious the tissue damage and the more severe the degenerative process.
Drug treatment
Medicines, their dosage and regimen of use are determined by a medical specialist individually for each patient, necessarily taking into account various factors, such as the person’s age, gender, location and severity of damage. Drug therapy primarily includes the use of drugs from several pharmacological groups:
- Non-steroidal anti-inflammatory drugs - drugs are used to reduce the severity of inflammation of moderate intensity. Usually tablet or injectable dosage forms are prescribed in combination with drugs for external use (cream or ointment).
- Glucocorticosteroids are hormonal drugs that are prescribed for severe long-term inflammation, in particular against the background of an autoimmune reaction.
- Chondroprotectors are a group of drugs that reduce the rate of destruction of cartilage tissue and also promote its restoration.
- Vitamins - allow you to speed up the process of tissue regeneration, as well as improve the general condition of the patient.
As an alternative method of conservative therapy, intra-articular administration of platelet mass (a biological preparation that is a suspension of platelets in physiological solution) is possible. It contains biologically active compounds “growth factors” that stimulate regeneration processes in cartilage and connective tissue.
Classification
The Stoller classification divides the condition of the meniscus into 4 stages. Depending on which of them is identified, the presence or absence of meniscus pathologies is determined.
- Stage 0 according to Stoller. The examination does not reveal foci of pathological changes in the tissues. The condition of the meniscus is assessed as completely healthy.
- Stage 1 according to Stoller. MRI reveals a signal of increased intensity, which is focal in nature and clearly localized. At the same time, it does not reach the surface of the cartilage tissue. Treatment most often in this case is not yet required or, if the need for treatment is nevertheless identified, it is carried out using conservative methods, mainly of a preventive nature.
- Stage 2 according to Stoller. The intensity of the signal received from the tissues is increased, but its character changes to linear. Similar to the first stage, it does not reach the upper layer of the meniscus (cartilage). If horizontal damage to the meniscus is detected, it means that the cartilage tissue is partially destroyed, but there are no changes in its structure. Treatment is mandatory. It can be predominantly conservative. Stoller grade 2 meniscal damage is the most common reason for seeking medical help.
- Stage 3 according to Stoller. The signal is recorded linear with significantly increased intensity. It clearly reaches the top layer of cartilage. The patient exhibits a pronounced violation of the anatomical structures of the meniscus. This means the presence of medial meniscus tears. Also, with such a lesion, displacement of some areas of injured cartilage cannot be ruled out. This condition is diagnosed as a complete tear of the meniscus with displacement. Treatment is required and is usually carried out surgically. Stoller grade 3 meniscal damage is the most severe.
Since diagnosing and classifying a lesion according to Stoller is only possible with a magnetic resonance imaging device, this service is not available in all medical institutions. Today, the stoller method determines the degree of meniscus damage most accurately.
DIAGNOSTICS
Diagnosis of meniscal damage includes taking a medical history, clinical examination by a specialist, and instrumental research methods. To exclude damage to bone structures and clarify the relationship between the components of the joint, as a rule, an X-ray examination is performed (damage to the menisci is not visible on the images, since the menisci are transparent to X-rays). To visualize the menisci and other intra-articular structures, the most informative non-invasive method currently is magnetic resonance imaging (MRI). Computed tomography (CT) and ultrasound diagnostics (US) are also used.
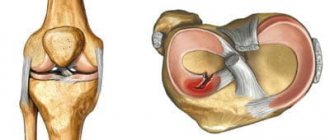
1 intact meniscus. 2 Damage to the posterior horn of the meniscus.
Traumatic injuries to the menisci are often combined with damage to other structures of the knee joint: cruciate ligaments, collateral ligaments, cartilage, and capsule of the knee joint.
The most accurate and complete diagnosis is carried out during the initial stage of arthroscopic surgery, during examination and revision of all parts of the joint.
Clinical picture according to Stoller (according to Stoller) - classification
The clinical manifestations of the pathology according to the classification also vary depending on the stage of the lesion. They additionally allow us to assess the patient’s condition.
- Stage 0 according to Stoller. Since there are no pathologies of the cartilage and its integrity is not compromised, there are no symptoms of pathology.
- Stage 1 according to Stoller. Minimal changes in the joint lead to periodic pain in it. They usually appear in the evening and are more intense in people who have to seriously overload their joints during the day. There may also be a noticeable crunching sound when the knee bends.
- Stage 2 according to Stoller. The impairment in the condition of the joint is quite pronounced, causing the pain to become significant. Its intensity increases when a person moves his leg, using his knee. Also, the pain increases after a long stay in a standing position. In most cases, external manifestations of inflammation are also observed, such as redness of the skin and swelling of the tissues. A crunch in the joint appears with almost every movement.
- Stage 3 according to Stoller. Serious changes occur in the anatomical structure of the cartilage, which causes not only severe pain, but also severe limited mobility of the knee joint. The pain syndrome, as well as stiffness of movement, is greatest in this condition. The clinical picture of the pathology is acute.
The presence of symptoms in addition to MRI allows the patient's condition to be accurately determined. This is the only way the therapy will be most effective.
Symptoms
Damage to the internal meniscus of the knee in the form of a tear is characterized by the appearance of several main clinical signs:
- Pain localized mainly on the inside of the knee. Its intensity depends on the cause of the injury (after an injury the pain is acute, but during degenerative processes it develops gradually). It increases when trying to perform movements in the knee, as well as against the background of loads on the lower limbs.
- Limitation of mobility with a decrease in the range of movements in the knee, up to complete block, which occurs with a complete rupture of the meniscus, accompanied by a sharp onset of acute pain.
- Inflammatory signs include redness of the skin (redness), swelling of the soft tissue (edema), and increased pain that may be present at rest.
The severity of clinical symptoms depends on the location and severity of the pathological process. With the gradual destruction of cartilage tissue against the background of degenerative-dystrophic processes, signs appear gradually, they can intensify over a fairly long period of time.
How to prepare for the procedure
Special preparation is not required before MRI with further classification of the condition of the Stoller meniscus. The study is subject to the same contraindications as MRI, and primarily the presence in the body of metal elements and various electrical stimulators and insulin pumps, the operation of which can be affected by the magnetic field of the device.
There will be no pain or discomfort during the examination. The only thing that the patient needs to take into account is that the procedure is lengthy. If the patient is very nervous before the examination, it is recommended that he take valerian or another herbal sedative.
Surgery on the medial or lateral meniscus
For severe meniscus tears and/or associated knee ligament injuries, surgery is recommended.
For this type of meniscus tear, arthroscopy is used.
A camera, an arthroscope, is inserted into the knee, after which the condition of the cartilage layer is assessed. Since in most cases the “handle” is upside down, microtools are used to return the severed part to its normal position.
The trauma surgeon determines the further tactics of the operation: if it is possible to restore the integrity of the meniscus, then sutures are placed on it. If it is not possible to reconstruct the cartilage layer of the knee, a meniscectomy is performed. A meniscectomy is an operation during which the entire meniscus or only part of it is removed. This article will help you learn about all the details of knee surgery.
Rehabilitation and return to training after a meniscus injury takes 4-6 months or more.
Surgery on the medial or lateral meniscus
For severe meniscus tears and/or associated knee ligament injuries, surgery is recommended.
For this type of meniscus tear, arthroscopy is used.
A camera, an arthroscope, is inserted into the knee, after which the condition of the cartilage layer is assessed. Since in most cases the “handle” is upside down, microtools are used to return the severed part to its normal position.
The trauma surgeon determines the further tactics of the operation: if it is possible to restore the integrity of the meniscus, then sutures are placed on it. If it is not possible to reconstruct the cartilage layer of the knee, a meniscectomy is performed. A meniscectomy is an operation during which the entire meniscus or only part of it is removed. This article will help you learn about all the details of knee surgery.
Rehabilitation and return to training after a meniscus injury takes 4–6 months or more.
REHABILITATION.
After the operation, the patient is given an aseptic bandage on the wounds and compression stockings are put on for the purpose of thromboprophylaxis and swelling reduction for a period of 3 weeks.
All patients are recommended to wear the orthosis for 4 weeks. The next day after surgery, patients are allowed to begin moving the joint and walking with partial support. The sutures are removed 12-14 days after surgery. Full load on the operated joint is allowed no earlier than 8 weeks, physical exercise and sports – 4 months after surgery. Patients also undergo physiotherapeutic treatment to improve blood supply to the rupture area and accelerate regeneration.