Aceclofenac, 100 mg, film-coated tablets, 20 pcs.
The frequency of side effects listed below was determined according to the following (World Health Organization classification): very common (more than 10%), common (more than 1% and less than 10%), uncommon (more than 0.1% and less than 1%), rare (more than 0.01% and less than 0.1%), very rare (less than 0.01%), including isolated reports; frequency unknown (cannot be estimated from available data).
From the gastrointestinal tract:
often - nausea, vomiting, diarrhea, epigastric pain, intestinal colic, dyspepsia, flatulence, anorexia, constipation; in rare cases, the occurrence of erosive and ulcerative lesions, bleeding and perforation of the gastrointestinal tract (bloody vomiting, melena), stomatitis (including aphthous), pancreatitis was noted.
From the nervous system:
rarely - headache, dizziness, sleep disturbances (insomnia or drowsiness), agitation; in some cases, sensory disturbances were noted,
disorientation, memory impairment, vision, hearing, taste, tinnitus, convulsions, irritability, tremor, depression, anxiety, vertigo. aseptic meningitis, paresthesia.
Allergic reactions:
uncommon - skin rash; rarely - urticaria, bronchospasm, systemic anaphylactic reactions; very rarely - vasculitis, pneumonitis, Stevens-Johnson syndrome and Lyell's syndrome, anaphylactic shock, discoid lupus erythematosus; Isolated cases of eczema, erythema multiforme, and erythroderma were noted.
From the kidneys and urinary tract:
rarely - peripheral edema; very rarely - acute renal failure, interstitial nephritis, nephrotic syndrome, hematuria, proteinuria.
From the liver and biliary tract:
Rarely - hepatitis; very rarely - fulminant hepatitis.
From the hematopoietic organs:
very rarely - leukopenia; Isolated cases of thrombocytopenia, agranulocytosis, hemolytic anemia, aplastic anemia, and neutropenia have been described.
From the cardiovascular system:
Isolated cases of tachycardia, arterial hypertension, congestive heart failure, and coronary heart disease (CHD) were noted.
Respiratory system disorders:
rarely - shortness of breath, pulmonary edema;
very rarely bronchospasm.
Musculoskeletal and connective tissue disorders:
There have been isolated cases of leg cramps,
Laboratory indicators:
often - transient increase in transaminase activity in the blood; uncommon - increased concentrations of urea and creatinine in the blood; very rarely, increased levels of alkaline phosphatase in the blood.
ACECLOFENAC
Interaction
No drug interaction studies have been conducted with the exception of warfarin.
Aceclofenac is metabolized by the cytochrome P450-CYP2C9 system, and in
vitro
indicate that aceclofenac may be an inhibitor of this enzyme. Therefore, there is a possible risk of pharmacokinetic interaction with phenytoin, cimetidine, tolbutamide, phenylbutazone, amiodarone, miconazole and sulfaphenazole.
As with other NSAIDs, there is a risk of pharmacokinetic interaction with drugs that are metabolized in the liver, such as methotrexate and lithium preparations.
Aceclofenac is almost completely bound to plasma proteins, and, therefore, it is necessary to consider the possibility of substitution with other drugs that are highly bound to plasma proteins.
Due to the lack of pharmacokinetic interaction studies, the following information is based on information obtained with other NSAIDs:
The following combinations should be avoided
NSAIDs inhibit tubular secretion of methotrexate, and a metabolic interaction may also occur leading to decreased clearance of methotrexate. Therefore, during treatment with large doses of methotrexate (more than 20 mg/week), NSAIDs should always be avoided.
Some NSAIDs inhibit the renal excretion of lithium, resulting in increased serum lithium concentrations. This combination should be avoided unless frequent monitoring of serum lithium concentrations is possible.
NSAIDs inhibit platelet aggregation and damage the gastrointestinal mucosa, which may increase the activity of anticoagulants and increase the risk of gastrointestinal bleeding in patients taking anticoagulants.
The combination of aceclofenac with oral anticoagulants of the coumarin group, ticlopidine, thrombolytics and heparin should be avoided unless carefully monitored.
The following combinations may require dose adjustment and precautions:
The possible interaction of NSAIDs and methotrexate must be taken into account, especially in patients with renal failure. When taking both drugs, monitoring of kidney function is necessary. Precautions should be taken when taking NSAIDs and methotrexate simultaneously within 24 hours, because methotrexate concentrations may increase, resulting in increased methotrexate toxicity. It is believed that taking NSAIDs with cyclosporine or tacrolimus increases the risk of nephrotoxicity due to decreased renal prostacyclin synthesis. Therefore, when taking drugs simultaneously, it is important to monitor renal function. Concomitant use of acetylsalicylic acid and other NSAIDs may increase the incidence of adverse reactions and, therefore, caution is required when taking them together.
NSAIDs may reduce the diuretic effect of furosemide, bumetanide and the hypotensive effect of thiazide diuretics. Simultaneous treatment with potassium-sparing diuretics may be associated with an increase in the concentration of potassium in the blood serum, therefore monitoring the potassium level in the blood is necessary.
NSAIDs may also reduce the effect of some antihypertensive medications. Angiotensin-converting enzyme inhibitors or angiotensin II receptor antagonists in combination with NSAIDs can lead to renal failure. The risk of developing acute renal failure, which is usually reversible, may be increased in some patients with impaired nocturnal function, such as elderly patients or patients who are fluid-depleted. Therefore, the combination of such drugs with NSAIDs should be used with caution, patients should receive sufficient fluids with food, and renal function should be monitored.
There was no effect of aceclofenac on blood pressure when it was taken concomitantly with bendroflumethiazide, although interaction with other antihypertensive drugs such as beta-blockers cannot be ruled out.
Other possible interactions
Isolated cases of hypoglycemia and hyperglycemia have been reported. Therefore, for aceclofenac it is necessary to adjust the dose of drugs that cause hypoglycemia. When used simultaneously with the drug Aceclofenac;
— digoxin, phenytoin or lithium preparations -
Plasma concentrations of these drugs may increase;
- diuretics and antihypertensive drugs -
the effect of these medicines may be weakened;
- potassium-sparing diuretics -
may lead to the development of hyperglycemia and hyperkalemia;
- other NSAIDs or glucocorticosteroids -
the risk of side effects from the gastrointestinal tract increases;
-
selective serotonin reuptake inhibitors
(citalopram, fluoxetine, paroxetine, sertraline) - increases the risk of gastrointestinal bleeding;
- cyclosporine -
the toxic effect of the latter on the kidneys may increase;
- hypoglycemic
agents -
can cause both hypo- and hyperglycemia. With this combination of drugs, blood sugar control is necessary;
— acetylsalicylic acid -
the concentration of aceclofenac in the blood decreases;
— antiplatelet agents and anticoagulants -
the risk of bleeding increases (regular monitoring of blood clotting indicators is necessary);
-
zidovudine -
increases the risk of hematological toxicity.
The use of aceclofenac in patients with acute back pain - effectiveness and safety
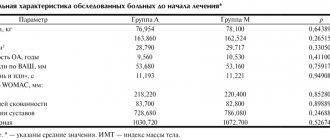
Kamchatnov P.R., Radysh B.B., Mikhailova N.A., Kutenev A.V.
Low back pain (LBP) is an extremely common clinical syndrome. Depending on factors such as body weight, the nature and regularity of physical activity, age, etc., LBP occurs in 70-90% of adults. There are nonspecific LBP, compression of the spinal root (radiculopathy), as well as LBP caused by specific lesions of the spine. Depending on the duration, there are acute (lasting less than 4 weeks), subacute (from 4 to 12 weeks) and chronic (lasting more than 12 weeks) LBP.
Nonspecific LBP is caused by osteoarthritis, osteochondrosis, and changes in periarticular tissues. It usually has a benign course and regresses or decreases significantly within 4-6 weeks [30]. The most common cause of root compression is a herniated disc. Rarely (less than 1%) LBP is caused by compression fractures due to osteoporosis, ankylosing spondylitis, tumors, and infectious processes.
Establishing a diagnosis is helped by a detailed clarification of the anamnesis - the peculiarities of the occurrence of pain, the factors that provoke its appearance and ensure its reduction, the identification of concomitant somatic diseases that can lead to damage to the spine, spinal cord membranes, and nervous structures [3].
Radiological examination (CT and MRI) is the main method of instrumental diagnosis of LBP. Tomographic examination is indicated to exclude specific causes of pain in patients with increasing pain, in the presence of neurological deficits, and in cases of severe somatic diseases. Radiography does not allow obtaining reliable information about the presence and size of a herniated intervertebral disc, the true size of the spinal canal in case of stenosis, etc. If indicated, radioisotope scintigraphy is used, which makes it possible to identify local accumulation of radiopharmaceuticals in the lesions, densitometry, and ultrasound examination.
Treatment
Complete and early elimination of pain is desirable in order to actively involve the patient in the process of treatment and rehabilitation, explain to the patient the benign nature of the disease, and teach him methods of preventing exacerbation. Ensuring an optimal level of daily physical activity is important. Excessive immobilization is undesirable not only in patients with isolated LBP, but also in most patients with radiculopathy. Early activation of the patient is of exceptional importance in preventing the development of depressive disorders and the formation of pain behavior [38].
In accordance with European recommendations for the treatment of patients with acute LBP, the first-line drug for its relief is paracetamol. In terms of analgesic effect, it is equivalent to acetylsalicylic acid and is comparable to or slightly inferior to most nonsteroidal anti-inflammatory drugs (NSAIDs). The anti-pain effect is realized due to the inhibition of cyclooxygenase activity in peripheral tissues and the central anti-inflammatory effect.
Experimental study of aceclofenac
NSAIDs are widely used - non-selective cyclooxygenase (COX) inhibitors, which have high analgesic and anti-inflammatory activity. This group includes aceclofenac (Aertal), a derivative of phenylacetylic acid (2-[2,6 - dichlorophenyl) amino] phenylacetoacetic acid), which is close in structure to diclofenac. In addition to inhibition, COX inhibits the expression of cell adhesion molecules (in particular, L-selectin), suppresses the adhesion of neutrophils to the endothelium, providing a pronounced anti-inflammatory effect [16], also due to the activation of the synthesis of interleukin-1 receptor antagonists and the suppression of the formation of nitric oxide [27].
Aceclofenac itself has a moderate inhibitory effect on COX types 1 and 2, however, under conditions of local inflammation by polymorphonuclear leukocytes and monocytes, aceclofenac is partially metabolized into diclofenac and 4-hydroxydiclofenac, due to which COX activity is inhibited [43].
Aceclofenac is able to prevent the degeneration of cartilage tissue. In the experiment, it demonstrated chondroprotective properties, providing interleukin-1-mediated suppression of the production of metalloproteinases, which stimulated the synthesis of proteoglycans by chondrocytes [4]. In a culture of cartilage tissue cells from patients with osteoarthritis, the use of aceclofenac was accompanied by an increase in the synthesis of proteoglycans and hyaluronic acid [6]. Aceclofenac, while ensuring the preservation of cartilage tissue, does not significantly affect the proliferation of tendon cells, without causing their hyperplasia.
Clinical effectiveness of aceclofenac
To date, considerable experience has been accumulated in the use of aceclofenac in patients with articular pathology. Analysis of the effectiveness of the drug in inflammatory diseases and in relieving pain syndromes allowed us to establish its anti-inflammatory effect, equivalent to ketoprofen, indomethacin and diclofenac in patients with rheumatoid arthritis, diclofenac and piroxicam for osteoarthritis of the knee joint, and indomethacin and naproxen for ankylosing spondylitis.
It is believed that the analgesic activity of 100 mg of aceclofenac in its duration of action exceeds that after taking 650 mg of paracetamol [8].
The authors of a review devoted to the analysis of the use of aceclofenac for the relief of acute pain syndromes (pathology of the ENT organs, dental, gynecological diseases, LBP) noted the high effectiveness of the drug [24]. The results of a double-blind, randomized study of the effectiveness of aceclofenac (200 mg/day) and paracetamol (3000 mg/day) in patients with osteoarthritis of the knee joint (168 patients included, treatment duration - 6 weeks) showed greater effectiveness of aceclofenac with better tolerability [5 ].
A multicenter, randomized, double-blind study was devoted to a comparative study of the effectiveness of aceclofenac (200 patients received 100 mg 2 times a day) and diclofenac (197 patients, 50 mg 3 times a day) for osteoarthritis of the knee joint [42]. As a result of a 12-week course of treatment in both groups, there was significant significant relief of pain and an increase in range of motion in the affected joints. However, a more pronounced effect and early normalization of joint mobility were recorded with the use of aceclofenac. A larger number of patients noted improvement after taking aceclofenac (71 and 59% after taking diclofenac), while the frequency of side effects with its use was significantly lower (1.0 and 6.6%). Similar results were obtained in a comparative multicenter study of aceclofenac and diclofenac in a similar group of patients with osteoarthritis of the knee joint [12]. The differences in the effectiveness of the drugs were not so pronounced, however, the frequency of side effects when taking aceclofenac was 5.9%, diclofenac - 11.5%, and an increase in the level of aminotransferases, which caused drug withdrawal, was observed in 0.6% of patients receiving aceclofenac, and in 3.0% of patients taking diclofenac.
A 12-week randomized, multicenter, double-blind study compared the effectiveness of aceclofenac (100 mg 2 times/day, 190 patients) and naproxen (500 mg 2 times/day, 184 patients) in patients with osteoarthritis of the knee joint [23]. There were no significant differences in the effectiveness of the drugs between the groups, however, the frequency of side effects was lower in the group of patients receiving aceclofenac (34 cases in 24 patients - 12.6%) compared to patients receiving naproxen (43 cases in 30 patients - 16.6%). 3%), and the differences also concerned gastrointestinal complications. A comparison of the effectiveness of aceclofenac (100 mg 2 times / day, 123 patients) and piroxicam (20 mg / day, 117 patients) was carried out in patients with osteoarthritis of the knee joint [31] during an 8-week randomized, multicenter, double-blind study. The effectiveness of the drugs turned out to be comparable, but the effect of using aceclofenac occurred earlier (in the 2nd week) compared to piroxicam (in the 4th week). Side effects were observed in 24 and 33 patients, respectively, despite the fact that detection of occult blood in feces was half as common after taking aceclofenac.
As part of a 6-month multicenter, double-blind study, 170 patients received aceclofenac (100 mg 2 times/day) and diclofenac (50 mg 3 times/day) [29]. Reduction of pain and improvement of movements occurred in both groups, however, motor disorders were relieved to a greater extent in patients receiving aceclofenac (17 and 22%, respectively).
Data from clinical studies (pronounced analgesic effect, good tolerability), as well as the unique effect of the drug on inflammatory mediators, speaks in favor of considering aceclofenac as the drug of choice for long-term therapy of patients with osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, and some other chronic degenerative lesions joints [33].
The pronounced anti-inflammatory and analgesic effects of aceclofenac led to the study of its effectiveness in patients with LBP. One of the first such studies was devoted to comparing the effectiveness of aceclofenac (135 patients, 100 mg 2 times a day) and tenoxicam (138 patients, 20 mg once a day) in patients with ankylosing spondylitis [39]. The study was multicenter, double-blind and lasted 12 weeks. Both drugs demonstrated high efficacy and comparable tolerability.
A multicenter, randomized, double-blind study compared the effectiveness of aceclofenac (100 mg 2 times/day) and diclofenac resinate (75 mg 2 times/day) in patients with acute nonspecific LBP [36]. The study included 227 patients; the course of treatment was 10 days. The timing and quality of pain relief were comparable in both groups, however, the use of aceclofenac was characterized by a significantly lower number of side effects.
Portability
Widespread, especially long-term, use of non-selective COX inhibitors is associated with a high risk of gastric bleeding. Due to the relatively low risk of gastrointestinal complications, the possibility of using selective COX-2 inhibitors is of great interest. A number of large randomized clinical trials performed in a double-blind manner have convincingly proven that selective COX-2 inhibitors have a significantly lower risk of gastrointestinal damage compared to non-selective drugs. Convincing results were obtained in the CLASS and VIGOR studies [7,37]. Aceclofenac inhibits the formation of COX-2 to a greater extent, as a result of which the incidence of serious gastrointestinal complications with its use is significantly lower than that of other NSAIDs (piroxicam, indomethacin, tenoxicam and ketoprofen) [19].
The tolerability of aceclofenac was studied in a 12-month prospective, open-label, multicenter study, SAMM [20]. Of 10,142 patients suffering from rheumatoid arthritis, ankylosing spondylitis and osteoarthritis, 2 groups were formed: the first (n=7890) consisted of patients receiving aceclofenac (100 mg 2 times a day), the second (n=2252) - diclofenac (according to 75 mg 2 times/day). The duration of treatment was 168 and 170 days, respectively. The total number of side effects, as well as the number of patients who stopped treatment due to intolerance, turned out to be significantly lower in the group receiving aceclofenac. The incidence of gastrointestinal reactions was 10.6 and 15.2%, respectively. The incidence of nausea, abdominal pain and diarrhea leading to discontinuation of treatment was 46, 65 and 41% lower, respectively, in the group of patients taking aceclofenac.
A slightly later Pan-European study included 23,407 patients with inflammatory and degenerative joint diseases [25]. Significant improvement, according to both patients and treating physicians, occurred in 84% of patients receiving aceclofenac, while 90% of them remained adherent to treatment. The results of the study made it possible to recommend aceclofenac for the relief of both acute and chronic pain syndromes.
Almost at the same time, a review of the results of studying the effectiveness of aceclofenac was published, obtained in the course of studies of different designs with various comparator drugs (diclofenac, naproxen, piroxicam, indomethacin, tenoxicam and ketoprofen) - a total of about 150 thousand patients [13]. The drug was noted to be sufficiently effective for relieving pain or inflammation with a course of treatment lasting from 2 to 6 months. along with a low incidence of side effects.
A large-scale study was carried out in the UK to establish the incidence of gastrointestinal and other complications due to the use of non-steroidal anti-inflammatory drugs [34]. The authors compared the risk of developing various complications due to oral administration of aceclofenac (200 mg/day), meloxicam (7.5 and 15 mg/day) and rofecoxib (25 mg/day). It was found that the frequency of side effects (number of cases/106 daily doses of the drug sold in the country) was 8.7 for aceclofenac (CI 6.1 - 12.0), 24.8 for meloxicam (CI 23.1-26.6) and 52.6 (CI 49.9-55.4) for rofecoxib. The use of aceclofenac was associated with a significantly lower incidence of gastrointestinal bleeding and abdominal pain. When taking aceclofenac, a significantly lower number of gastrointestinal complications, cases of abdominal pain, and hepatotoxicity were observed compared with rofecoxib. In general, it turned out that the best tolerability was observed with aceclofenac.
The use of selective COX-2 inhibitors is associated with an increased risk of cardiovascular complications, primarily acute myocardial infarction and an increase in systemic blood pressure [28,44]. However, this property of the drugs has not been confirmed in all studies. Thus, an observation of more than 30 thousand patients with osteoarthritis and rheumatoid arthritis who received diclofenac (150 mg/day) or eotricoxib (60-90 mg/day) established an almost identical risk of thrombotic complications when taking them [9]. The study cited above [34] recorded a significantly lower incidence of thrombotic complications and cases of increased blood pressure compared to meloxicam and rofecoxib.
Pharmacokinetics of aceclofenac
When administered orally, aceclofenac is quickly and completely adsorbed in the intestine and after 1.5-2 hours reaches its maximum concentration in the blood. The drug does not have cumulative activity, and its pharmacokinetics does not depend on the age of the patients. Prescribed orally 100 mg 2 times/day.
Contraindicated in case of exacerbations of gastric and duodenal ulcers, a history of the “aspirin triad,” or hematopoietic disorders of unknown etiology. The drug should not be used in the third trimester of pregnancy; its use in the first and second trimesters of pregnancy, as well as during lactation, is possible after a careful assessment of the benefit-risk ratio. The use of aceclofenac in children and adolescents under the age of 18 is not recommended.
With the simultaneous use of other drugs with aceclofenac, it is possible to increase the plasma concentrations of digoxin, phenytoin, lithium and reduce the effectiveness of diuretics and antihypertensive drugs. When taking aceclofenac and corticosteroids or other NSAIDs, the risk of developing side effects from the gastrointestinal tract increases. When used with acetylsalicylic acid, a decrease in the concentration of aceclofenac in the blood plasma is possible. With the simultaneous use of indirect anticoagulants, the risk of bleeding increases.
The presented information about the effectiveness and tolerability of aceclofenac (Aertal) allows us to consider it as the drug of choice in patients with acute back pain.
Literature
1. Badokin V.V. Efficacy and safety of aceclofenac in patients with osteoarthritis. RMJ. 2007; 13: 392-397. 2. Neverov V.A., Kurbanov S.Kh. Restorative treatment of degenerative-dystrophic diseases of large joints. Vestn. hir. them. I.I. Grekova 2004;163(2):97-108. 3. Nikiforov A.S., Konovalov A.N., Gusev E.I. Clinical neurology. In 3 volumes - Moscow: “Medicine”, 2002. 4. Akimoto H, Yamazaki R, Hashimoto S et al. A major metabolite of aceclofenac 4'hydroxy aceclofenac suppresses the interleukin-1 induced production of promatric metalloproteinases and release of sulfated-glycosaminoglycans from rabbit articular chondrocytes. Eur J Pharmacol 2000; 401(3): 429-436. 5. Batlle-Gualda E., Roman Ivorra J., Martin-Mola E. et al. Aceclofenac vs paracetamol in the management of symptomatic osteoarthritis of the knee: a double-blind 6-week randomized controlled trial. Osteoarthritis Cartilage. 2007; 15(8):900-908. 6. Blot L., Marcelis A., Devogelaer J.-P., Manicourt D.-H. Effects of diclofenac, aceclofenac and meloxicam on the metabolism of proteoglycans and hyaluronan in osteoarthritic human cartilage. British Journal of Pharmacology 2000; 131: 1413 – 1421. 7. Bombardier C., Laine L., Reicin A. et al.. Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group. N Engl J Med 2000; 343:1520-8. 8. Brogden R., Wiseman L. Aceclofenac. A review of its pharmacodynamic properties and therapeutic potential in the treatment of rheumatic disorders and in pain management. Drugs. 1996; 52(1): 113-124. 9. Cannon C., Curtis S., FitzGerald G. et al. Cardiovascular outcomes with etoricoxib and diclofenac in patients with osteoarthritis and rheumatoid arthritis in the Multinational Etoricoxib and Diclofenac Arthritis Long-term (MEDAL) program: a randomized comparison. Lancet. 2006; 18; 368(9549):1771-1781. 10. Carrabba M., Paresce E., Angelini M. et al. A comparison of the local tolerability, safety and efficacy of meloxicam and piroxicam suppositories in patients with osteoarthritis: a single-blind, randomized, multicentre study. Curr Med Res Opin. 1995;13(6):343-55. 11. Clare J., Tate S., Nobbs M., Romanos M. Voltage-gated sodium channels as therapeutic targets. Drug Discov Today 2000; 5:506-520. 12. Diaz C., Rodriquez de la Serna A., Geli C., Gras H. Efficacy and tolerance of aceclofenac versus diclofenac in the treatment of knee osteoarthritis. A multicenter study. Eur J Rheumatol Inflamm 1996; 16: 17-22. 13. Dooley M., Spencer C., Dunn C. Aceclofenac: a reappraisal of its use in the management of pain and rheumatic disease. Drugs. 2001;61(9):1351-1378. 14. Dougados M., Gueguen A., Nakache J.-P. et al. Ankylosing spondylitis: what is the optimal duration of a clinical study? A one year versus a 6 weeks non-steroidal anti-inflammatory drug trial. Rheumatology 1999;38:235-244 15. Gilbert F, Grant A, Gillan M et al. Scottish Back Trial Group. Low back pain: influence of early MR imaging or CT on treatment and outcome-multicenter randomized trial. Radiology. 2004; 231: 343-351. 16. Gonzalez-Alvaro I., Carmona L., Diaz-Gonzalez F. et al. Aceclofenac, a new nonsteroidal antiinflammatory drug, decreases the expression and function of some adhesion molecules on human neutrophils. J Rheumatol. 1996; 23(4): 723-729. 17. Harreby M., Nygaard B., Jessen T. et al. Risk factors for low back pain in a cohort of 1389 Danish school children: an epidemiologic study. Eur Spine J. 1999; 8(6): 444-450. 18. Harris A. Handicapped and Impaired in Great Britain, Part I. London, England: Social Survey Division, Office of Population Census and Surveys. Her Majesty's Stationary Office; 1971. 19. Henrotin Y, De Leval H, Mathy-Hartet M et al. In vitro effects of aceclofenac and its metabolites on the production by chondrocytes of inflammatory mediators. Inflamm Res 2001; 50: 391-399. 20. Huskisson E., Irani M., Murray F. A large prospective open-label, multicentre SAMM study, comparing the safety of aceclofenac in patients with rheumatic disease. Eur J Rheumatol Inflamm 2000; 7:1-7. 21. Koes B., van Tulder W., Thomas S. Diagnosis and treatment of low back pain. BMJ 2006;332;1430-1434. 22. Koleck M. Mazaux, J. Rascle N. et al. Psycho-social factors and coping strategies as predictors of chronic evolution and quality of life in patients with low back pain: A prospective study. European Journal of Pain. 2006; 10:1-11. 23. Korsanoff D., Frerick H., Bowdler J., Montull E. Aceclofenac is a well-tolerated alternative to naproxen in the treatment of osteoarthritis. Clin Rheumatol 1997; 16 (1): 32-8. 24. Legrand E. Aceclofenac in the management of inflammatory pain. Expert Opin Pharmacother. 2004; 5(6): 1347-1357. 25. Lemmel E., Leeb B., De Bast J., Aslanidis S. Patient and physician satisfaction with aceclofenac: results of the European Observational Cohort Study (experience with aceclofenac for inflammatory pain in daily practice). Aceclofenac is the treatment of choice for patients and physicians in the management of inflammatory pain. Curr Med Res Opin. 2002;18(3):146-153. 26. Li Y., Gorassini M., Bennett D. Role of persistent sodium and calcium currents in motoneuron firing and spasticity in chronic spinal rats. Neurophysiology 2004; 91:767-783. 27. Maneiro E., Lopez-Armada M., Fernandez-Sueiro J. et al. Aceclofenac increases the synthesis of interleukin 1 receptor antagonist and decreases the production of nitric oxide in human articular chondrocytes. J Rheumatol. 2001; 28(12): 2692-2699. 28. Mukherjee D., Nissen S., Topol E. Risk of cardiovascular events associated with selective COX-2 inhibitors. JAMA. 2001; 286:954-9. 29. Pasero G., Marcolongo R., Serni U. et al. A multi-centre, double-blind comparative study of the efficacy and safety of aceclofenac and diclofenac in the treatment of rheumatoid arthritis. Curr Med Res Opin. 1995;13(6):305-315. 30. Pengel L., Herbert R., Maher C., Refshauge K. Acute low back pain: systematic review of its prognosis. BMJ. 2003; 327: 323-326. 31. Perez Busquer M., Calero E., Rodriguez M. et al. Comparison of aceclofenac with roxicam in the treatment of osteoarthritis. Clin Rheumatol 1997; 16 (2): 154-59. 32. Pincus T., Burton A., Vogel S., Field A. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine. 2002; 27: 109-120. 33. Reginster J., Paul I., Henrotin Y. What is the role of aceclofenac in the therapeutic arsenal against chronic osteoarthritis pathologies? Rev Med Liege. 2001; 56(7): 484-488. 34. Raber A., Heras J., Costa J. et al. Incidence of spontaneous notifications of adverse reactions with aceclofenac, meloxicam, and rofecoxib during the first year after marketing in the United Kingdom. Therapeutics and Clinical Risk Management 2007:3(2) 225-230 35. Rudwaleit M., Metter A., Listing J., Sieper J. Inflammatory back pain in ankylosing spondylitis: a reassessment of the clinical history for application as classification and diagnostic criteria. Arthritis Rheum. 2006; 54: 569-78. 36. Schattenkirchner M., Milachowski K. A double-blind, multicentre, randomized clinical trial comparing the efficacy and tolerability of aceclofenac with diclofenac resinate in patients with acute low back pain. Clin Rheumatol. 2003; 22(2): 127-135. 37. Silverstein F., Faich G., Goldstein J. et al. Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: a randomized controlled trial. Celecoxib Long-term Arthritis Safety Study. JAMA 2000; 284:1247-55. 38. van Tulder M., Becker A., Bekkering T. et al. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J (2006) 15(Suppl. 2):S169-S191. 39. Villa Alcazar L., de Buergo M., Rico Lenza H., Montull Fruitos E. Aceclofenac is as safe and effective as tenoxicam in the treatment of ankylosing spondylitis: a 3 month multicenter comparative trial. Spanish Study Group on Aceclofenac in Ankylosing Spondylitis. J Rheumatol. 1996; 23(7):1194-1199. 40. Von Korff M., Saunders K. The course of back pain in primary care. Spine. 1996; 21: 2833-7283. 41. Wang G., Russell C., Wang S. State-dependent block of voltage-gated Na-channels by amitriptyline via the local anesthetic receptor and its implication for neuropathic pain. Pain 2004; 110:166-174. 42. Ward D., Veys E., Bowdler JM, Roma J. Comparison of aceclofenac with diclofenac in the treatment of osteoarthris. Clin Rheumatol 1995; 14: 656-62. 43. Yamazaki R., Kawai S., Matsuzaki T. et al. Aceclofenac blocks prostaglandin E2 production following its intracellular conversion into cyclooxygenase inhibitors. Eur J Pharmacol. 1997; 329(2-3): 181-187. 44. Zhao S., Burke T., Whelton A. et al. Comparison of the baseline cardiovascular risk profile among hypertensive patients prescribed COX-2-specific inhibitors or nonspecific NSAIDs: data from real life practice. Am J Manag Care. 2001; 8(15 Suppl): S392-400. Key words of the article: aceclofenac, patients, effectiveness, Application, acute
SOURCE RMJ JANUARY 26, 2010, VOLUME 18, NO. SPECIAL