Why do my joints hurt?
Limited mobility and pain can develop due to poor nutrition and destruction of articular cartilage.
This happens gradually: with age, the process of self-healing of the cartilage tissue of the joint slows down and the amount of intra-articular fluid decreases. This process is accelerated by diabetes, thyroid disease, injuries and bruises. There is also evidence of hereditary predisposition1. The cartilage becomes dehydrated, becomes thinner and is easily injured: this causes the processes of bone tissue degeneration to begin. To reduce pressure on painful areas, the body forms growths on the bones, and joint deformation occurs. Inflammation of the synovium leads to morning stiffness and shooting pain1,2.
Since all these processes occur slowly, people only become concerned when the disease has progressed too far and requires drug treatment.
Treatment of knee pain
If pain occurs in the knee, it is necessary to limit the motor mode in order to protect the joint and prevent the pathological process from intensifying. Under no circumstances should you “walk through” the pain. You can use anti-inflammatory ointments and elastic bandages on your own, but you should not forget about the need to see a doctor who will prescribe physical therapy, shock wave therapy, massage or, in rare cases, a surgical procedure.
If an inflammatory process has begun in the knee, it can lead to swelling of the joint and the need for a puncture to remove fluid. This is an unpleasant procedure that can be avoided with timely initiation of treatment. You should also promptly exclude the possibility of oncological pathologies.
Modern medicine has a wide range of effective methods for treating diseases of the knee joints, most of which help to avoid surgical intervention and are limited to a combination of drug and hardware treatment.
What medications should I take for joint pain?
Treatment with non-steroidal, anti-inflammatory drugs of different groups for pain in muscles and joints is aimed at:
- reduction of pain and inflammation in the joint (first group);
- restoration of cartilage tissue1, (second).
The first group includes glucocorticosteroids and non-steroidal anti-inflammatory drugs, which are used during an exacerbation in the form of ointments, injections and tablets. This is a symptomatic treatment that leads to a rapid development of the effect - a reduction in pain and inflammation. As a rule, tablets and injections are not prescribed for a long time, because such drugs may be unsafe, especially in older people. Therefore, they are used in short courses in low doses3.
The second direction is the prescription of chondroprotectors, which include glucosamine and chondroitin sulfate. They act more slowly, but are better tolerated by the body. Chondroprotectors help restore cartilage tissue, reduce pain and restore joint mobility4.
Application of Sirdalud in rheumatological practice
About the article
11233
0
Regular issues of "RMZh" No. 24 dated November 27, 2005 p. 1586
Category: General articles
Author: Badokin V.V. 1 1 Federal State Budgetary Educational Institution of Further Professional Education RMAPO Ministry of Health of the Russian Federation, Moscow
For quotation:
Badokin V.V. Application of Sirdalud in rheumatological practice. RMJ. 2005;24:1586.
The main clinical manifestations of a wide range of inflammatory and, to a lesser extent, degenerative diseases of the joints and spine are pain, stiffness and limited mobility. All these manifestations are closely interconnected and actively influence each other. In particular, the functional insufficiency of the musculoskeletal system (at least in the early period of development of these diseases) is significantly influenced not only by the severity of pain, but also by the severity of morning stiffness.
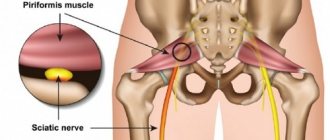
Pain and stiffness are most common in rheumatoid arthritis (RA), ankylosing spondylitis (AS) and other seronegative spondyloarthritis (SSA), as well as dorsopathies, including myofascial syndrome. Patients with RA experience pain of the inflammatory type, which is most pronounced in the morning, and these pains are usually accompanied by morning rigidity. In this disease, the intensity of morning stiffness and its duration adequately reflect the activity of the inflammatory process and make it possible to judge not only the severity of the laboratory activity of the disease, but also the activity of changes occurring in the tissues. Severe stiffness that persists for many months and does not improve with active anti-inflammatory therapy is an unfavorable prognostic factor and is often associated with the possible progression of structural changes in the joints. In patients with RA, the cause of joint pain, as well as stiffness, is an inflammatory process in the synovium (synovitis) and periarticular soft tissues (tenovaginitis, tenosynovitis, bursitis), stretching of the joint capsule with effusion, tunnel syndromes, and functional instability of the affected joints. Pain and rigidity are no less important in the polymorphic picture of AS and SSA. It is known that inflammatory pain in the spine (pain in the early morning hours for three or more months, which does not decrease with rest and weakens after physical activity) is included in the diagnostic criteria for AS. The dynamics of pain intensity is one of the indicators of response to therapy and a criterion for remission in this disease (ASAS response criteria and ASAS remission criteria) [1]. As for rigidity or stiffness, this symptom, as well as in RA, adequately reflects the activity of the inflammatory process in AS, and to a greater extent than laboratory tests such as ESR and C-reactive protein levels. The dynamics of the severity and duration of morning stiffness also allows us to judge the effectiveness of the therapy. For AS and other SSA, this is all the more important because in this group of diseases there is a dissonance in clinical and laboratory tests of disease activity and often a pronounced inflammatory process can occur with normal or subnormal laboratory values for a long period, and sometimes throughout the entire disease. Rigidity (stiffness) at the beginning of the development of AS is often localized only in the lumbar spine, gradually spreading throughout the entire axial skeleton. It is usually more pronounced in the early morning hours, but in some patients with high activity of the inflammatory process it lasts throughout the day. The intensity and duration of rigidity corresponds to the intensity of pain in the spine, emphasizing their common genesis. The presence of an inflammatory process in the spine causes reflex tension in the back muscles, which, in turn, leads to changes in posture and deformation of the spine (physiological lordosis in the lumbar spine is leveled, kyphosis in the thoracic spine is emphasized and hyperlordosis develops in the cervical spine). In advanced cases, a “petitioner” pose, characteristic of patients with AS, is formed with a positive Forestier symptom, high values of the Thomayer test and a significant impairment of the functional ability of the spine, and the limitation of mobility and deformation of the spine is supported not only by structural changes in the joints and ligaments of the spine, but also by hypertonicity of the muscles. The causes of pain in AS are inflammatory changes in the peripheral, root and sacroiliac joints, as well as in the spine. As is known, all structures of the spinal column, with the exception of bone tissue, contain nerve endings and can cause pain [2]. Free nerve endings that function as pain receptors have been identified in the capsules of the intervertebral joints, the posterior longitudinal and interspinous ligaments, the vertebral periosteum, the walls of arterioles and veins, the vessels of the paravertebral muscles, and the outer third of the fibrous ring of the intervertebral discs. Dorsalgia in this disease can be a manifestation of vertebrogenic radicular syndrome (radiculopathy) or reflex pain syndromes. Radiculopathy is based on compression of the nerve roots by inflammatory swelling of the intervertebral canal or a deformed spine. There are other possible causes of the development of dorsalgia, such as spondylolisthesis, spinal canal stenosis, osteoporosis, herniated intervertebral discs and, less commonly, posterior or anterior osteophytes, secondary arthrosis of the intervertebral (facet) joints, spondylosis. Often the basis of the pain syndrome is the failure of the structures that ensure the vertical position of the body. In addition to compression syndromes, with BD, reflex (muscular-tonic) syndromes are possible, which are caused by irritation of receptors in response to changes in the discs, ligaments and joints of the spine. Impulses from the receptors reach the motor neurons of the spinal cord, and this is accompanied by an increase in the tone of the corresponding muscles. Spasmed muscles lead to limited mobility of a certain segment of the spine, and also become a secondary source of pain, which triggers a vicious circle of “pain - muscle spasm - pain”. Such changes persist for a long time and contribute to the formation of myofascial syndrome [2]. It should be noted that hypertonicity of striated muscles also takes part in the genesis of the development of contractures and muscle fibrosis. Some authors consider increased muscle tone as one of the risk factors for this disease and its poor prognosis. With osteoarthritis, stiffness is not as important as with inflammatory joint diseases. At the same time, with this degenerative disease, pain in the affected joints is sometimes persistent, and in some patients it occurs almost constantly. When the knee or hip joints are affected, which occur with reactive (secondary) synovitis, the pain transforms from a mechanical type to an inflammatory type with the natural appearance of morning stiffness, although its duration does not exceed 30 minutes. Pain and stiffness can be a symptom of a large group of conditions that are characterized by low back pain. These diseases are currently united by the term dorsopathies and include syndromes accompanied by back pain of vertebrogenic and non-vertebrogenic origin [3]. Among vertebrogenic causes are deforming dorsopathies, spondylopathies (spondyloarthrosis, ankylosing spondylitis), dorsalgia, instability of the spine with the formation of spondylolisthesis, and among non-vertebrogenic ones - muscular-fascial-ligamentous pain, which owes its development to prolonged muscle overstrain. Pain syndromes in the axial skeleton periodically occur in almost all people over the age of 40. In people under 45 years of age, pain in the lower back is the most common cause of temporary disability [4,5]. In degenerative diseases of the spine, the main pathogenetic factors in the development of such syndromes are compression mechanisms and reflex effects with the addition of inflammatory disorders, microcirculatory disorders and their combinations. The peculiarity of pain syndromes in the lumbar spine is a combination of reflex muscular-tonic and myofascial syndromes with changes in the emotional and personal sphere. The most common reflex pain syndromes encountered in clinical practice (about 85% of patients with back pain) [2]. They are caused by irritation of the receptors of the fibrous ring, muscle-articular structures of the spine and are usually not accompanied by neurological disorders. In such cases, muscle spasm develops early, which initially has the character of a protective physiological phenomenon, increasing the pain threshold and limiting the mobility of the affected part of the spine. Spasmed muscles are a secondary source of pain, and they trigger a vicious circle of “pain - muscle spasm - pain”, which contributes to the development of myofascial syndrome. In many rheumatic diseases, spasticity syndrome develops, although not in such a pronounced form as is observed in neurological practice. Spasticity is understood as a movement disorder accompanied by an increase in muscle tone and caused by damage to the corticospinal tract [6]. Spasticity syndrome is a manifestation of upper motor neuron involvement. A variety of symptoms of damage to these motor neurons, in addition to muscle rigidity, include muscle atrophy, the development of contractures and fibrosis. Regulation of muscle tone is carried out under the influence of both central and peripheral impulses of a-motoneurons of the spinal cord. These motor neurons, located in the anterior horns of the spinal cord, innervate muscle fibers [6]. The occurrence of spasticity is based on a violation of the inhibitory influences of the supraspinal regions on spinal motor and interneurons. These disorders at the spinal level lead to an imbalance in the processes of excitation and inhibition. Not only dysfunction of the central and peripheral nervous system is involved in the origin of spasticity. Of no less importance in this process is the organic and functional state of the striated muscles. To relieve increased muscle tone or reduce its intensity, muscle relaxants are most often used. Their use not only helps to significantly reduce hypertonicity, but also reduces the severity of pain, prevents the formation of contractures, improves the functional ability of the musculoskeletal system, facilitates the possibility of carrying out extensive rehabilitation measures, and preserves the patient’s ability to work and his activity in everyday life [6]. Muscle relaxants, by reducing the severity of muscle tone, lead to an increase in the range of motion in the spine and peripheral joints, which makes their use advisable. This group of drugs includes baclofen, tolperisone, Sirdalud, diazepam, tetrazepam and others. Tolperisone is a muscle relaxant with central anticholinergic action. It has a selective inhibitory effect on the caudal part of the reticular formation of the brain stem and thereby leads to a decrease in muscle relaxant activity. This drug has a membrane-stabilizing effect. It also blocks spinal mono- and polysynaptic reflexes. The structure of tolperisone is close to the structure of local anesthetics, especially lidocaine. This may explain its inherent analgesic effect. In addition, it has a weak antispasmodic and vasodilator effect. The implementation of the therapeutic effect of this drug is associated with a reduction in sodium current on the membrane of nerve fibers and cells. Treatment with tolperisone is usually carried out in case of severe morning stiffness or the presence of severe spastic syndrome, and the dose of the drug is 100–150 mg 2 times a day. A faster and more pronounced effect is observed with intramuscular administration of the drug (1 ml contains 100 mg of mydocalm) 2 times a day. Baclofen also has a muscle relaxant effect. Like other drugs in this group, baclofen has moderate antispastic and analgesic activity. The drug is an analogue of g-aminobutyric acid (GABA). It binds to presynaptic GABA receptors, leading to a decrease in the release of excitatory amino acids (glutamate, aspartate) and suppression of mono- and polysynaptic activity at the spinal level, which causes a decrease in muscle tone. Baclofen is used to treat painful muscle spasms in patients with damage to the spinal cord and brain structures. A special place among other muscle relaxants is occupied by the imidazole derivative Sirdalud (tizanidine). Sirdalud is a centrally acting muscle relaxant and is a specific agonist of a2-adrenergic receptors. Its therapeutic effect is associated with inhibition of the release of excitatory neurotransmitters from presynaptic neural terminals [4]. It reduces muscle tone due to stimulation of monoaminergic nuclei of the brain stem, which, in turn, leads to inhibition of spinal motor neurons and, accordingly, to muscle relaxation, relief of muscle-tonic syndromes and spasticity (Table 1). The antispastic effect of Sirdalud is comparable to that of baclofen and diazepam, but it has a more favorable tolerability and safety profile [6]. The drug also has a distinct analgesic effect. The analgesic effect is due not only to the direct influence of Sirdalud on the antinociceptive system, but also indirectly - due to a decrease in pathologically increased muscle tone. The main indications for the use of Sirdalud are severe rigidity, painful muscle spasm, myofascial syndromes and skeletal muscle spasticity [7,8]. The drug is administered orally (initial dosage – 2 mg 1 time per day). For severe morning stiffness, it is advisable to prescribe an additional 2 mg at night. When selecting a dose to achieve maximum effect, it is possible to increase the dose to 2-4 mg 3 times a day. The therapeutic effect of Sirdalud is dose-dependent, and when prescribed, the effectiveness gradually increases, reaching its maximum already in the first three days from the start of therapy. For acute pain syndromes, the drug is prescribed for 5–7 days, and in the presence of chronic pain accompanied by spasticity, the duration of therapy is determined individually. For inflammatory diseases of the joints and spine, Sirdalud should be prescribed simultaneously with NSAIDs, and for myofascial syndromes with severe pain, it should usually be taken in combination with analgesics, although in some cases it can be used as monotherapy. To date, several dozen studies have been conducted to study the biological effects of Sirdalud. As a result of these studies, it was found that the drug reduces muscle tone, reducing only its tonic, and not the phasic component. This leads to the preservation (and in some cases, an increase) of muscle strength, which distinguishes it favorably from tolperisone and baclofen, which do not have these properties. Thanks to this feature and distinct analgesic effect, Sirdalud increases the daily activity of patients and improves their quality of life. The gastroprotective effect of the drug seems interesting, which is associated with its adrenergic activity and antispasmodic effect [9,10]. This property of Sirdalud is important, since patients with chronic joint diseases take NSAIDs for a long time, and some of them almost constantly, and this, in turn, contributes to the development of erosive gastritis and gastric and/or duodenal ulcers. Published experimental data suggest that Sirdalud reduces the incidence of gastrointestinal side effects caused by NSAIDs by reducing basal and induced secretion of hydrochloric acid in the stomach, as well as eliminating the imbalance of glycoproteins in the gastric mucosa and gastric secretions. In addition, this drug suppresses spontaneous motility of the ileum and slows down intestinal passage. Interestingly, clonidine, which is also an α2-adrenergic receptor agonist, has similar effects on the gastrointestinal tract. It follows from this that the antisecretory activity of Sirdalud is a characteristic property of the entire class of a2-adrenergic receptor agonists. The gastroprotective activity of Sirdalud has been confirmed in numerous clinical studies. It has been established that Sirdalud improves the tolerability of NSAIDs (in particular, diclofenac) and potentiates their analgesic effect [10]. In a multicenter, double-blind, placebo-controlled study based on a study of 405 patients with acute local pain syndromes and clinically significant muscle spasms, it was found that the Sirdalud-diclofenac combination was more effective than the placebo-diclofenac combination in most respects. [9]. For 7 days, patients took Sirdalud 4 mg/day. and 50 mg diclofenac (main group) or placebo and 50 mg diclofenac (control group). The frequency of gastrointestinal side effects in the main group was 12%, in the control group – 32%, and the frequency of a positive test result for occult blood – 5 and 11%, respectively. Not only the tolerance of the combination of sirdalud with Diclofenac is much better than a placebo with Diclofenac, but its therapeutic effectiveness turned out to be higher. According to the above study, a very good result of therapy was noted in 40% of patients with the control group and satisfactory - in 16%, and in the comparison group - in 27 and 28%, respectively. Similar data were obtained in another work, where Diclofenac was evaluated in combination with Sirdalud (4 mg/day) in a 2 -weekly controlled study in patients with pain in the lower back. It was possible to identify a more significant decrease in pain and improve the mobility of the spine in the group of patients who received combined therapy, compared with monotherapy, diclofenac, while the indicators of the survey questionnaires recommended for assessing the back pain have improved by 25%, and the severity of pain by visual analogue scale (yours) from 56 mm decreased to 34 mm. The same study notes good tolerance of such a combination. In the presence of muscle hypertonicity, it is better to combine the treatment of muscleroxants with an analgesic drug. Such combined therapy, of course, has a pathogenetic justification. As you know, muscle tension is a protective reaction to pain, and pain, in turn, is emotional stress and leads to an increase in muscle tone that determine the protective pose. In addition, the development of myofascial syndrome, due to the same muscle overload, is not excluded. The relief of the reflex tension of the muscles leads to an improvement in tissue blood supply, which helps to normalize metabolic disorders. Sirdalud in small doses rarely leads to undesirable reactions. In addition to drowsiness, inhibitance and reducing concentration of attention, dizziness, dry mouth, increased fatigue, intestinal dyspepsia (extremely rarely - an increase in liver aminotransferase) can be observed. Against the background of sirdalud, a moderate decrease in blood pressure is possible, especially since it is able to potentiate antihypertensive drugs. But in general, Sirdalud is characterized by good tolerance both with short -term and prolonged use, and the unwanted phenomena that are inherent and extremely rarely lead to its cancellation. It should be borne in mind that the cessation of therapy should take place gradually, since their sudden cancellation may be accompanied by a short -term increase in muscle tone, which is also observed with the rapid cancellation of other muscle relaxants. Thus, the symptom - the treatment of pain and rigidity for inflammatory and degenerative diseases of the joints and spine should be complex and aimed both at reducing the intensity of pain or their complete elimination and the elimination of rigidity. That is why in each case it is advisable to prescribe non -steroidal anti -inflammatory drugs in combination with muscle relaxants. Although the symptom -modifying therapy does not slow down the rate of development of the disease (in particular, the progression of structural changes) the appointment of NSAIDs and muscle relaxants significantly improves the quality of life, prevents the development of muscle atrophy and flexible contractures, and also helps to preserve the functional ability of the supporting and motor apparatus. Literature 1. Dougados m, dijrmans b, Khan M. et al. Sonventional Treatments for Ankylosing Spondylitis. Ann Rheum Dis 2002; 61, SUPPL. III: 40-50. 2. Alekseev V.V. Diagnosis and treatment of back pain. Coonsilium medicus 2002; 4 (2): 96–102. 3. Shostak N.A. The role of muscle relaxants in rheumatic diseases. Breast cancer 2005; 13 (8): 557–9. 4. Chen D - F, Bianchetti M, Weisendanger M. Motor Disturbances. Ed. R.Benecke et al. London, 1987. 5. Korthlas - de Bos I, Van Tulder M. Econonic Evalving and Randomized Trials in Spinal Disorders: Principiples and Methods. Spine 2004; 29: 442–8. 6. Damulin I.V. Spasticity syndrome and the main directions of its treatment. Journal of Neurology and Psychiatry 2003; 12: 4–9. 7. Derry H, Hutchinson Dr. A multrical Placebo - Controlled Study in General Practice to Evaluate the Efficacy and Safety of Tizanidine Low - Back Pain. J Intern Med Ress 1988; 16: 75–82. 7. Who Department of noncomunicable disseagement. Low back pain initiative. Geneve, 1999. 8. Emre M. The Gastroprotective Effects of Tizanidine: An OverView. Curr Therapeutic Res 1998; 59 (1): 2–12. 9. Sirdalud Ternilin Asia - Pacific Study Group. Efficacy and Gastroproprotective Effects of Tizanidine Plus Diclofenac Versus Plus Diclofenac in Painful Muscle Spasm. Curr Thes 1998; 59: 13–22. 10. COWARD DM Tizanidine: Neuropharmacology and Mechanism of Action. Neurology 1994; 44, 11 (SUPPL. 9): 6–11.
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
What are the advantages of drugs to improve cartilage regeneration?
Most patients who took chondroitin preparations as a joint medicine did not complain of side effects, and tests showed that their cartilage destruction stopped and the joint space stopped decreasing5.
To reduce joint pain, glucosamine and chondroitin sulfate, according to clinical studies, should be taken for at least 8-12 weeks continuously. During this time, active substances accumulate in cartilage and synovial fluid and trigger a cascade of reactions that1,5:
- increase the production of synovial fluid - the natural lubrication of the joint;
- increase the synthesis of protecoglycans - the main components of cartilage tissue;
- inhibit the activity of enzymes that destroy cartilage.
The effectiveness of the use of chondroitin and glucosamine in stimulating the regeneration of joint cartilage tissue has been confirmed in many clinical studies1,5.
A combination drug, Teraflex, was created based on chondroitin and glucosamine. It has proven effective as a drug that delays the progression of the disease1 and as a means of reducing the symptoms of osteoarthritis6. Taking Theraflex helped reduce the dose of painkillers and improve the well-being of patients when treating joint pain7.