Antibiotics are substances of biological or semi-synthetic origin. They are used in medical practice to combat pathogenic microbes and viruses. Before the advent of these medications, typhoid fever, dysentery, pneumonia, and tuberculosis had the status of incurable diseases. Today, treatment of infectious diseases is possible with the use of 1-6 generations of antibiotics.
At this moment, the pharmacological industry produces more than 2000 varieties of drugs of this type. Doctors have described the effects of about 600 positions, and about 120-160 drugs are used in medical practice.
Important! For any disease, it is recommended to take antibiotics after consulting a doctor. Otherwise, antibiotic resistance may develop (decreased sensitivity of pathogenic microorganisms to antibacterial agents).
Infectious arthritis - what is it?
Infectious arthritis is characterized by an inflammatory process occurring inside the joint. This may be caused by bacteria, viruses, parasites or fungi.
This type of arthritis can affect absolutely any joint.
. A characteristic feature of the disease is that in addition to local manifestations (swelling, pain and joint immobility), there are also general symptoms (fever, chills, signs of intoxication).
Infectious arthritis refers to a group of diseases caused by various types of infectious agents that penetrate specifically into the structure of the tissues that form the joint.
According to existing statistics in the field of rheumatology and traumatology, arthritis of this type is diagnosed in every third patient.
The most common site of infectious arthritis is the joints of the upper and lower extremities
.
Spectrum of action
There are antibacterial agents:
Causes of infectious arthritis
The most likely cause of infectious arthritis is the metastatic route of joint damage, which involves direct penetration of infection into the joint tissue through the blood or lymph.
Another route of infection can be injury or an open wound, as well as the spread of pathogens from nearby foci of another disease, for example, osteomyelitis.
Arthritis caused by infectious pathogens in childhood is usually provoked by staphylococcus, enterobacteria or Haemophilus influenzae. However, at the same time, other arthritis, quite specific for this age category, may occur, caused by tuberculosis, gonorrhea or syphilis.
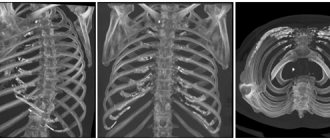
Degrees of arthrosis of the ankle joint
The most widely used classification is that of Kellgren and Lawrence:
- Zero stage. There are no signs of arthrosis.
- First stage. The radiograph raises doubts among the doctor. Darkening is visualized in places of tissue changes.
- Second stage. The image shows minimal changes in the structure of the joint.
- Third stage. Signs of pathology are pronounced and are clearly visualized on an x-ray. Changes in cartilage and bone are determined.
- The material is sent for analysis for differential diagnosis with inflammatory arthritis, gout, and infection.
Signs and symptoms of infectious arthritis
The key symptom of infectious arthritis is considered to be an acute manifestation, accompanied by a large number of symptoms.
Among the main signs and symptoms of infectious arthritis, general symptoms include fever, chills, excessive sweating and a constant feeling of weakness. As an additional symptom, children may experience nausea and vomiting.
Considering the local signs of infectious arthritis, it is worth highlighting:
- sharp pain during palpation/performing movements;
- local redness of the skin, swelling, fever.
It is also worth noting that the clinical picture of arthritis of infectious origin directly depends on the causes of its occurrence. Thus, septic arthritis is often localized in large joints, arthritis of gonococcal etiology is accompanied by multiple rashes, and tuberculous arthritis corresponds to a chronic course.
Particular attention should be paid to the symptoms of viral arthritis: short-term course, the possibility of restoration of articular tissues, without negative consequences
.
Stages of development of infectious arthritis
In order to understand how to treat infectious arthritis and what measures will be most effective, it is important to understand at what stage the disease is.
In total, it is customary to distinguish 4 main stages of arthritis:
- Stage 1
– accompanied by the development of osteoporosis (chronically progressive decrease in bone density of the joint), without destructive changes; - Stage 2
– the initial stage of destruction of cartilage tissue, reduction of the joint space, the occurrence of single usurs (destructions on the surface) of the bone; - Stage 3
– significant damage to articular tissues, pronounced reduction in the joint space, the presence of subluxations and deviations (deviations from the norm) of the bones; - Stage 4
– symptoms of stage 3 + complete immobility of the joint.
Causes of ankle arthrosis
The development of degenerative processes is most often provoked by injuries, inflammation, and congenital disorders of the musculoskeletal system.
There are also risk factors that increase the likelihood of arthrosis:
- Age. Natural aging of the body is accompanied by a slowdown in metabolic processes. Articular cartilage is gradually destroyed, regeneration resources are no longer enough to compensate for natural wear and tear. Tissue trophism is also reduced. As a result, the joint space narrows and osteophytes form. The first signs of arthrosis of the ankle joint can be noticed after 40 years.
- Overweight. The joints of an obese person experience increased stress. The fact of the relationship between excess weight and the formation of arthrosis has been clinically proven.
- Injuries and operations on the joint. Ligament ruptures, dislocations, sprains, and cartilage damage disrupt the functioning of the joint. Even if the injury did not have obvious clinical manifestations, post-traumatic arthrosis of the ankle joint can form over time.
- Genetic predisposition. The tendency to arthrosis is inherited from parents to children.
- Hormonal imbalance. The level of sex hormones matters. With insufficient secretion, the rate of cartilage regeneration decreases. Under load, the joint becomes thinner and osteophytes form.
- Excessive loads. Among professional athletes and people engaged in physically demanding jobs, arthrosis is a common disease. Signs of joint destruction from overuse can occur at a young age.
- Arthritis. Neglected or poorly treated inflammation is a serious risk factor. Arthrosis can be caused by rheumatoid arthritis and other pathologies.
Types of arthritis of infectious origin
Considering the etiology of the disease, it can be noted that all infectious arthritis have several varieties, including:
- bacterial;
- viral;
- fungal;
- parasitic
.
At the same time, depending on the identified type of disease, the following subtypes of arthritis are also distinguished:
- septic
(pyogenic/purulent); - gonorrheal
; - syphilic
, etc.
Causes of pathology
The main cause of ankle arthrosis is metabolic failures in cartilaginous tissues. Factors contributing to the occurrence of pathology are:
- high loads;
- injury to the joint and its structures;
- overweight;
- wearing high-heeled shoes;
- ankle surgery;
- rheumatic diseases;
- purulent arthritis;
- gout and other pathologies that arise against the background of metabolic failures;
- diseases accompanied by disruption of the musculoskeletal system of the leg and foot (lumbar osteochondrosis, hernias, etc.);
- living in regions with poor environmental conditions;
- genetic factors.
In rare cases, the disease develops against the background of congenital joint abnormalities, syphilitic or tuberculosis infection.
Diagnosis of infectious arthritis
Before determining how to treat infectious arthritis, it is important to understand what its etiology is.
(causes of occurrence) and
forecasts
. All the information necessary for this can be determined diagnostically.
Diagnosis of infectious arthritis is carried out by specialists in the field of surgery, traumatology and rheumatology. If necessary, you can also consult an infectious disease specialist or venereologist for advice.
Among the measures used to clarify the diagnosis, it is worth highlighting:
- ultrasound examination of the affected area (ultrasound);
- X-ray examination;
- CT/MRI of the joint.
The disease is diagnosed in people of different ages: from infants to the elderly.
Treatment of infectious arthritis
The primary treatment for arthritis of any type is pain relief
,
antibiotic therapy and
,
of course
,
fever reduction
.
In order to achieve the most effective results, both medicinal and non-medicinal methods can be used as treatment.
All
measures
included in the treatment plan for various types of arthritis
are determined exclusively by the attending physician
, based on the results of a diagnostic examination. In most cases, treatment of infectious joint inflammation is carried out inpatiently.
IMPORTANT! Self-medication can cause the situation to worsen and the consequences to become irreversible.
Physiotherapy as a method of treating infectious arthritis
Physiotherapy
is a unique treatment that can be used both at the treatment stage and for rehabilitation purposes after radical measures.
Among the most effective measures it is customary to highlight:
- magnetic therapy;
- use of amplipulse or sinusoidally modulated currents;
- electrophoresis (introduction of drugs into joint tissues through exposure to electric current);
- laser or ultrasound therapy;
- local exposure to paraffin or ozone.
Massage as a method of treating infectious arthritis
Massage
– a great way to improve/restore blood circulation to the affected joint. Despite its usefulness, you should resort to this method only after consultation with your doctor.
To treat various types of arthritis, the following types of massage can be used:
- local
– concentrated on a specific area of the human body;
- general
– the use of massage techniques is distributed throughout the body.
It is important to note that massage cannot be the only treatment for arthritis.
. Only an integrated approach, involving the use of drug treatment in tandem with physiotherapeutic methods, massage and specialized exercises, can give a chance for complete tissue restoration and elimination of the symptoms of the disease.
Exercise therapy as a method of treating infectious arthritis
Physiotherapy
– a special method of treating arthritis of various types, in particular those caused by infectious diseases.
Various types of exercises and static positions are an effective means of not only treating, but also preventing diseases of joint tissues.
A set of gymnastic exercises allows you to achieve stable remission and minimize pain, swelling and pathological tension of muscle tissue.
Signs of illness
Arthrosis progresses slowly, and symptoms may increase over several years.
When to see a doctor:
- There was pain. In the early stages, it may simply be discomfort, a pulling, aching sensation after a long walk. Gradually, the pain intensifies and disrupts the normal functioning of the joint.
- Lameness, change in gait. These are the consequences of pain syndrome. The person places his foot in the most comfortable position for him.
- Stiffness of movements. The symptom of arthrosis of the ankle joint is clearly visible in the morning, when after sleep you cannot move your leg. After some time, mobility is restored.
- Joint deformity. Visible changes develop in advanced cases and in the later stages of the disease. Osteophytes form on the articular surfaces, which deform the leg.
Use of drugs in the treatment of infectious arthritis
Drug therapy in the treatment of arthritis is a fairly effective method that has the desired effect on the patient’s body. In case of timely application of a well-chosen treatment plan, it can be stated that the prescribed therapy is successful
.
As part of treatment, taking into account the causes and characteristics of the course of the disease, various types of antibiotics
, as well as other groups of drugs. Let's look at some of them in detail.
Chondroprotectors in the treatment of infectious arthritis
Chondroprotectors
- This is a group of long-acting drugs, the use of which is necessary for several months.
Prescribing a course of drugs of the presented type allows you to create favorable conditions for the restoration of articular tissues, which significantly affects the patient’s quality of life, due to the restoration of the functionality of the affected joint
.
The most effective drug of the group of chondroprotectors is considered to be “ Structum”
».
Antispasmodics in the treatment of infectious arthritis
Use of antispasmodics
provides the opportunity to relieve patients from muscle pain that occurs as a result of joint damage.
Among the frequently prescribed ones, it is worth highlighting “ Drotaverine
».
Nonsteroidal anti-inflammatory drugs in the treatment of infectious arthritis
Nonsteroidal anti-inflammatory drugs
(NSAIDs) are excellent helpers in the treatment of arthritis. The action of drugs of this type allows the patient to get rid of pain.
The frequency, duration of use and dosage are determined by the attending physician, based on the existing clinical picture.
One of the most effective drugs of this type is “ Artradol
».
Reactive arthritis
What is reactive arthritis?
Reactive arthritis is an inflammatory non-purulent joint disease that develops after an acute intestinal or genitourinary infection.
How common is reactive arthritis?
Among rheumatic diseases, reactive arthritis is the most common disease. Its prevalence is 86.9 people per 100 thousand children. Teenage boys and young men are most often affected.
Why does reactive arthritis occur?
One of the most common causes of reactive arthritis is chlamydial infection. In childhood, chlamydial arthritis accounts for up to 80%. Children and adults can become infected with chlamydia through contact with people who are carriers of the infection, as well as from animals (cats, dogs), and birds. Infection occurs through airborne droplets, airborne dust, sexual contact, household contact, and also during the passage of the fetus through the infected birth canal of the mother.
The second most common causative agents of reactive arthritis are intestinal microorganisms. The causative agents of intestinal reactive arthritis include Yersinia, Salmonella, Shigella, and Campylobacter.
How does reactive arthritis manifest?
Usually, when questioning the patient, you can find out that 1-3 weeks before the onset of joint manifestations, the patient suffered from an acute respiratory infection, an intestinal disorder, or urinary disorders (pain, increased frequency of urination). Reactive arthritis itself begins acutely, the temperature rises, and the general condition worsens. Large joints of the lower extremities are affected - knees, ankles, heels, metatarsophalangeal and interphalangeal joints, and less commonly, hand joints.
Most often, the joints of the lower extremities become inflamed, especially the toes, where swelling also develops, spreading to the entire finger, and a bluish or purple-bluish coloration of the skin (the finger becomes like a sausage or radish). In addition to arthritis, the development of enthesopathies is characteristic - inflammation of the tendons at the places of their attachment to the bones, especially often in the heel area. Some patients may experience pain in the spine. In many cases, reactive arthritis is short-lived (from several days to several weeks) and goes away with treatment, but in some patients it can become chronic.
In Reiter's disease, a typical form of reactive arthritis, along with articular manifestations, there are signs of urethritis and eye damage (conjunctivitis and more severe forms).
Options for eye damage in Reiter's disease can be the following: conjunctivitis (inflammation of the conjunctiva of the eye) - most often not purulent, with a light discharge, quickly passing; recurrent iridocyclitis (inflammation of the iris and ciliary body) is a type of uveitis with a favorable course; panuveitis (inflammation of all layers of the choroid - iris, ciliary body, choroid) with retinal detachment, up to loss of vision.
Uveitis is characterized by redness of the eyes, photophobia, lacrimation, transient decrease or blurred vision, changes in eye color, changes in the shape and size of the pupil.
Extra-articular manifestations are characterized by damage to the skin, most often in the form of a rash, mucous membranes of the oral cavity (stomatitis), heart, peripheral nervous system (neuritis); skin (curatoderma).
Is reactive arthritis dangerous?
The prognosis for life and long-term functional ability is generally favorable.
Unfavorable prognosis factors for reactive arthritis are considered to be: frequent exacerbations of articular syndrome, hereditary predisposition to rheumatic diseases, carriage of the HLA-B27 antigen, ineffectiveness of anti-inflammatory and antibacterial therapy.
Deaths with reactive arthritis are rare; the main reason is the development of complications, in particular heart damage (carditis, myocarditis).
To reduce the risk of complications and prevent the transition of the acute course of reactive arthritis to chronic, timely and adequate treatment of the infectious process of the inflammatory process is necessary, which requires constant monitoring by a rheumatologist.
How is reactive arthritis diagnosed?
The diagnosis of Reiter's disease or reactive arthritis is made on the basis of data on a previous infection, analysis of the characteristics of the clinical picture, data from laboratory and instrumental examination methods and results for the presence of the pathogen.
What treatments are there for reactive arthritis?
The goal of treatment for reactive arthritis is to eliminate the infectious agent, cure or achieve stable clinical and laboratory remission.
Treatment of a patient with reactive arthritis should be carried out in a specialized hospital. Treatment of reactive arthritis is conservative and includes the use of antibacterial drugs, non-steroidal anti-inflammatory drugs, and glucocorticoids as indicated. During the period of subsidence of acute inflammatory phenomena, exercise therapy and massage are indicated.
One of the main methods of treatment is the prescription of antibacterial drugs. Since chlamydia is a microorganism with a special type of life activity, the choice of antibacterial drugs is limited. These antibiotics include macrolides, tetracyclines and fluoroquinolones.
However, tetracyclines and fluoroquinolones are quite toxic and have side effects that limit their use in pediatric practice. In this regard, macrolides are most often used to treat chlamydia in children. In children over 8 years of age, tetracyclines can be used.
Antibiotic therapy is more effective in the acute stage of Reiter's syndrome.
In case of protracted and chronic course of reactive arthritis, antibiotic therapy is not effective enough.
In patients with chronic reactive arthritis, the immune system functions inadequately, pathological reactions predominate over protective ones. Given these features, various immunomodulatory agents are used to treat chronic chlamydial arthritis. However, their use should be extremely careful, only as prescribed by a doctor.
For the treatment of reactive arthritis of chlamydial etiology in children, treatment regimens using Taktivin, glucosaminylmuramyl dipeptide, and N-hydroxy poly-1,4-ethylenepiperazine have also been developed. The administration of immunomodulators stimulates the body's protective properties and increases overall resistance.
Prescribing antibiotics and immunomodulators does not solve the general problem of treating reactive arthritis. Since the disappearance of chlamydia from the genitourinary organs does not mean a complete cure. The components (antigens) of microorganisms persist longer than the pathogen itself. Control studies are required one, two, three months after the end of treatment. If necessary, repeated courses of antibiotics and immunomodulators are possible. Only a doctor can decide whether a repeat course is necessary.
Antibacterial therapy is advisable for all children with reactive arthritis in whom antibodies to coliform bacteria are detected in diagnostic titers or intestinal bacteria are cultured during bacteriological examination of stool. The drugs of choice are aminoglycosides.
In addition to therapy aimed at eliminating the infection, symptomatic therapy is prescribed.
Non-steroidal anti-inflammatory drugs. Prescribed to reduce pain in all patients. The drugs are prescribed for the acute period. The dose of the drug is calculated depending on the age and weight of the patient.
Steroid anti-inflammatory drugs. Glucocorticosteroids have the most powerful and rapid anti-inflammatory effect. They are the drugs of choice when it is necessary to quickly stop disease activity, pain, and developing complications. The main route of administration of glucocorticoids for reactive arthritis is intra-articular.
Immunosuppressive drugs. In case of continuous exacerbation of articular syndrome, the presence of enthesopathies, limited mobility of the spine (the child does not reach more than 15 cm with his fingertips to the floor), inflammatory changes in blood tests and the ineffectiveness of standard therapy, the prescription of immunosuppressive drugs is indicated. The drug of choice is Sulfasalazine. Prescribed and canceled only by a doctor. Treatment is carried out for a long time (years), under the control of general and biochemical blood tests to prevent the development of side effects.
Primary prevention has not been developed. The main focus is to prevent the development of the disease:
- Healthy lifestyle
- Sanitation of foci of infection.
- Maintaining personal hygiene rules
- Treatment of parents for chlamydia
- Immunogenetic counseling and identification of parents of HLA-B27 antigen carriers
- Family planning
Secondary prevention – prevention of relapse of the disease
- Healthy lifestyle
- Maintaining personal hygiene rules
- Seeing a doctor earlier
- Following the recommendations of a rheumatologist
- Do not self-medicate
Surgical method of treatment
In a situation where complex therapy is unable to cope with the existing degree of damage to the joint, radical methods come to the rescue, including surgery.
Surgical treatment of arthritis is used only in severe cases. Among the types of surgical intervention there are such measures as:
- arthroscopy
is a low-traumatic operation that involves the removal of bone processes; - endoprosthetics
– replacement of articular elements with implants; - arthrodesis
– absolute fixation of the joint; - osteotomy
- excision of part of the bone tissue of the affected joint in order to reduce pressure on it; - arthroplasty
is a complete replacement of the affected joint.
Forecasts and prevention of infectious arthritis
Considering the prognosis of the disease, it is worth noting that only one third of patients with arthritis of infectious origin at the end of treatment are faced with unpleasant residual effects, which are expressed by joint immobility.
The most dangerous types of the disease are septic arthritis, because despite fairly favorable prospects, the fatal outcome is 5-15%
.
The risk group for developing infectious arthritis includes people of different ages who have ailments such as:
- rheumatoid arthritis;
- osteoarthritis;
- bad habits;
- weakened immune system;
- obesity of varying degrees.
For the purpose of prevention, it is recommended to follow the basics of dietary nutrition, attend prescribed therapeutic events, promptly treat existing diseases and, of course, monitor the general health of the body.
Recommendations for infectious arthritis
To maintain the effectiveness of therapy, as well as achieve the most favorable results, it is important to follow a number of recommendations for infectious arthritis, including:
- Movement is an integral part of therapy.
- Maximum limitation of sudden movements and forces that create additional stress on the affected joints.
- Improving power sensations.
- Simplifying everyday processes through the use of modern technological solutions.
- Increasing personal safety by installing additional handrails in the apartment, using anti-slip mats, etc.
Features of nutrition during treatment and prevention of infectious arthritis
Therapeutic nutrition for arthritis of various types is aimed primarily at normalizing the immune response, as well as weakening inflammatory processes, in order to restore the range of motion of the affected joint.
Nutritional features depend on:
- stages of disease development;
- presence of concomitant diseases;
- severity of clinical manifestations.
Based on this, we can come to the conclusion that there is no single diet. However, there are a number of general principles for creating a diet, including:
- fractional meals;
- preference for certain types of culinary food processing (boiling/baking/steaming/stewing);
- food intake temperature – no more than 60°C;
- limiting salt and liquid intake;
- giving up bad habits;
- saturating the diet with vitamins.