On the plantar side of the metatarsophalangeal joint of the first toe, in the structure of the flexor apparatus there are two small bones smaller than a pea. Despite the fact that the bones are very small in size, they play a huge role during walking, running, jumping and other stress on the foot. If the sesamoid bones are involved in any pathological process, they become a source of severe pain, significantly worsening the patient’s quality of life.
Sesamoid bone problems
Sesamoid bones (from Latin Sesamum) are bones located deep within the tendons and usually lying on the surface of other bones.
Sesamoids are noted in areas where tendons pass over joints (eg, wrist, knee, foot). The sesamoid bones provide protection to the tendons and keep the tendons some distance from the center of the joint, increasing the leverage of force. Most bones in the human body are connected to each other through joints. However, there are also bones that do not directly articulate with other bones. Instead, they are located deep within the muscles or tendons. Such bones are called sesamoids. The largest of them is the patella (kneecap).
Sesamoid bones act as blocks. They form a smooth surface along which the tendon slides, increasing the moment of force developed by the corresponding muscle. The sesamoid bones in the forefoot area are also involved in distributing the load exerted by the body weight when walking and are involved in the movements of 1 toe.
- Pain localized under the first toe on the plantar surface of the foot. With sesamoiditis, pain may develop gradually, while with a fracture, pain occurs immediately after the injury.
- Swelling and hemorrhages, which may not exist.
- You may also experience pain and difficulty bending and straightening 1 finger.
During a clinical examination, the doctor will specifically examine the sesamoid bones for tenderness in this area. The doctor may also carefully evaluate the movements of 1 finger and ask you to bend and straighten it. When dorsiflexing 1 finger, you may notice increased pain.
To make a diagnosis, your doctor will order an x-ray. For many people, the sesamoid bone located toward the center of the foot (the medial sesamoid bone) consists of two parts. The edges of such fragments of sesamoid bone are usually smooth, whereas the edges of the fragments during a fracture are sharp, jagged, so radiography usually makes it possible to make the correct diagnosis.
Treatment of injuries and diseases of the sesamoid bones is usually conservative. However, if this treatment is ineffective, you may be advised to undergo surgery to remove the sesamoid bone.
Sesamoiditis
- Stopping those types of physical activity that lead to increased pain
- Taking aspirin or ibuprofen for pain relief
- Rest and application of ice to the plantar surface of the foot. Do not apply ice directly to the skin. It is better to use an ice pack or wrap the ice in a towel.
- Wearing shoes with soft soles and low heels. Wearing shoes with hard soles can also be more comfortable.
- Using a soft shock-absorbing pad to relieve the sesamoid bones.
- Return to physical activity should be gradual and continued use of dense foam rubber pads. Activities that place stress on the forefoot should still be avoided.
- Taping 1 finger to give and hold it in a position of some plantar flexion.
- To reduce swelling and inflammation, your doctor may recommend a local injection of glucocorticoid.
- If the symptoms of the disease persist, the doctor may recommend immobilizing the foot with a removable splint, as for a fracture, for a period of 4-6 weeks.
- Wearing shoes with hard soles or immobilization with a short splint.
- Taping of 1 metatarsophalangeal joint to limit the movements of 1 finger.
- To relieve the sesamoid bones while the fracture heals, you may be advised to wear a special “J” shaped pad.
- You may also be advised to take painkillers such as aspirin or ibuprofen.
- Discomfort after a sesamoid bone fracture can persist for up to several months.
- Often, various shock-absorbing pads and other orthopedic devices are used during the healing period of a fracture.
Rehabilitation
Rehabilitation after conservative treatment
If the pain syndrome is mild, the doctor may allow you to continue your daily activities immediately, but with the condition that you use shoes with hard soles. If the disease is moderate, you will need to use crutches and not put any weight on your leg for a period of several days to two to three weeks. If the pain is severe, you will need to walk on crutches without putting any weight on your leg for several weeks. Typically, full recovery should not be expected until four to six weeks.
Physical therapy can help reduce pain and swelling. If there are no contraindications, then ultrasound and thermal procedures are prescribed. Sometimes the use of anti-inflammatory ointments and creams is combined with physiotherapy.
Rehabilitation after surgical treatment
After surgery, most patients are advised to use crutches and avoid putting weight on the leg. For those who have undergone restoration of the flexor apparatus of the first toe or bone grafting, immobilization with a plaster or plastic splint is recommended. After this, it is recommended to wear shoes with hard soles until complete recovery. The results of bone grafting of the sesamoid bone can be assessed after 2 months by performing an MRI.
Physical therapy exercises are required. Depending on the operation performed, exercises begin at different times after the operation, gradually increasing the load and complexity. Therapeutic exercise is necessary to restore and maintain muscle tone of the lower leg and foot.
Treatment of arthrosis with folk remedies
Treatment of the condition depends on the underlying pathology. Inflammatory diseases should be treated with antibiotics, hormonal drugs and NSAIDs. Arthritis of rheumatoid etiology can be cured only with basic therapy. With the development of degenerative destruction, chondroprotectors are selected, and hyaluron preparations are injected into the joint cavity.
The structure of the knee joint is important to consider when removing pathological inclusions. Surgical correction is prescribed for fractures and ruptures of connective tissue elements. Malignant processes can be cured with chemotherapy and radiation therapy. Functional treatment of the knee joint and postoperative rehabilitation includes exercise therapy, taping, physiotherapy methods, the use of orthopedic shoes and body weight correction.
Arthrosis is a disease that often occurs in older people, athletes, heavy industry workers and simply people who load their joints for a long time. It occurs gradually as the cartilage tissue of the joints becomes thinner and deformed. The first manifestations are pain when moving, inflammation and swelling.
At your first visit to the doctor, examinations are prescribed that must be completed as soon as possible:
- X-ray;
- magnetic resonance, computed tomography;
- blood test (general, biochemical).
These examination methods help determine the stage of arthrosis, differentiate it from diseases with similar symptoms (arthritis), and prescribe the correct treatment.
For arthrosis, the doctor prescribes comprehensive treatment for joints
Drug therapy:
- anti-inflammatory drugs;
- painkillers;
- chondroprotectors.
Physiotherapy:
- massages;
- electrophoresis;
- magnetic, laser therapy;
- physiotherapy.
Surgery in the late stages of arthrosis, with irreversible deformation of the cartilage, without the results of drug treatment.
Treatment at home:
- folk remedies for arthrosis;
- self-massage.
In human anatomy[edit]
Sesamoid bones can be located in any joint area, including:
- knee joint - patella (in the thickness of the quadriceps tendon)
- hand - two sesamoid bones are located in the distal parts of the first metacarpal bone. There is usually also a sesamoid bone in the distal portion of the second metacarpal. The pisiform bone of the wrist is also, in fact, a sesamoid, located in the tendon of the flexor carpi ulnaris. [1]
- foot - two sesamoid bones in the area where the first metatarsal bone joins the first toe (inside the tendon of the flexor hallucis brevis). [2]
All sesamoid bones play the role of blocks. They regulate and direct muscle force during movements. The patella is part of the extensor apparatus of the leg. The role of the kneecap is as follows.
- Increases the strength of the quadriceps femoris muscle (block function).
- Stabilizes the knee joint. The concave inner surface of the patella keeps the ends of the bones from moving laterally.
- Protects the knee from injury. We tested this on ourselves more than once in childhood: repeatedly skinned knees did not in any way affect the health of our knee joints.
Tendon bursae reduce the friction of the tendons on the surface of the bones and allow the patella to slide up and down freely. When the knee flexion angle does not exceed 90 degrees, only the lateral femoral condyle is in contact with the patella. With further flexion, the medial articular surface comes into contact with the medial condyle.
The structure of the femoral-patellar joint in many people differs from the classic one. The patella may be made up of two, three, or even four separate bones. There are cases when the kneecap is flattened or its inner surface is irregular in shape. There is an irregular structure of the bones of the leg and thigh, for example, the condyles of the femur are too small.
Surgical treatment
Sesamoid bone removal
Your doctor may suggest removing part or all of the sesamoid bone. When the sesamoid bone is partially removed, the other sesamoid bone is able to provide a fulcrum for the flexors. However, if both bones are removed, the flexors will not be able to function normally and the first toe will become claw-shaped. Therefore, surgeons usually avoid removing both sesamoid bones.
When the sesamoid bone is fractured, surgery is performed to remove non-functional fragments and restore the integrity of the flexor apparatus. For stress fractures in athletes, when the most complete recovery is needed, surgery can be performed using bone grafts. To remove the sesamoid bones, an incision is made on the inside of the foot. Sometimes it becomes necessary to perform this operation from an incision along the plantar side of the foot between the heads of the first and second metatarsal bones.
Anatomy and structure
The knee joint is considered the largest and most complex in structure. It is this joint that has the greatest range of motion when walking and is subject to great functional load and pressure. The articulation is formed by the tibia and femur, covered by the patella. The joint contains numerous connective tissue structures that act as shock absorbers.
The knee joint is a complex and complex joint. The articulation is a condylar device; its structure contains a head in the shape of a rounded ellipse-shaped process. The knee is designed in such a way that there are no muscles in front, but at the back they form a diamond-shaped depression where nerve bundles and vascular networks pass. The anatomy of the knee joint includes the femoral condyles, the superior surface of the tibia, and the anterior patella.
The tibial plateau is formed by the lateral and medial condyle, the superior side of the tibia. The articulation includes a special part - the sesamoid bone - the patella. The structure of the human knee contains a layer of cartilage that serves as a shock absorber and reduces friction when moving. The skeleton of the knees is covered from above by its own fascia. A knee injury is a serious injury that eliminates the load on the leg as a whole.
The patella and quadriceps are connected by a tendon that continues with the patellar ligament. The patellar ligaments keep the bones stable relative to each other during movement and prevent them from moving too much. The cruciate ligaments are located inside the knee joint. To prevent forward displacement of the tibia, the anterior region of the tibia is attached to the femur by fibers of the anterior ligament.
The posterior cruciate ligament bands of the knee prevent the calf from moving too far back. As a result of rupture of these structures, voluntary movements of the injured leg, for example, the left, are blocked. Cartilaginous structures separate the femur from the tibia. Each of them in cross-section looks like a crescent-shaped triangular disk. Intra-articular menisci evenly distribute a person's weight and stabilize the knees.
Joint capsule
Fibrous connective tissue covers the knee joint and protects it from damage and penetration of pathogenic agents. The main function of the joint capsule is protection. Since the tension level of the tight case is low, movement occurs in all planes. Topographic anatomy of the bursa:
- The synovial ball is internal, lining the joint from the inside and producing synovium. Lubricant nourishes the cartilage. The shell increases the mobility of the joint and protects the knees from mechanical stress. The layer is formed by villi.
- The fibrous capsular ball covers the outside of the knee joint.
Synovial bursae
The slit-like spaces formed by the articular membrane contain lubricant. The joint space capsules are considered an auxiliary muscle apparatus. The following knee joint capsules are distinguished, such as:
- patellar - the gap is located between the femur and the tendon;
- the infrapatellar is present under the patella;
- prepatellar - can be found between the skin and the patella;
- “crow's foot” is localized between the fibers of the semimembranosus and gastrocnemius muscles;
Epiphyses of bones
The distal end of the femur on top and the epiphysis of the tibia below form the knee. The surfaces correspond to each other as closely as possible, which ensures the possibility of movement. The thickenings of the femur are convex, and the tibial condyles are concave. However, since the ends are not completely identical, menisci are located between them.
The blood supply to the knee is provided by the vascular network, which is formed by the femoral, deep femoral, anterior tibial and popliteal arteries. A total of 13 joint networks have been described. Penetrating the fascia balls, branches of the arteries penetrate into the articular capsule. The femoropopliteal canal (also called Günter's canal) is the site of passage of the neurovascular bundle.
Innervation of the knee is provided by the sciatic and branches of the popliteal nerve. They conduct all types of sensation into the spinal cord. The tibial branch passes at the bottom of the popliteal fossa, which has a diamond-shaped outline, and the fibular bundle is located on the anterior surface. Nerve endings run along the edges of the cartilage.
Joint cavity
The internal space of the knee joint is a closed cavity. The normal volume when folded is about 35 ml, but when moving it increases to 200 ml. The walls of the gap are the synovial membrane, the sides of the femur and tibia. The cavity is divided into communicating chambers, forms the inversions of the knee joint and the upper and lower floors, which communicate through slits in the center.
Knee muscles
Movements of the knee joint are made in such planes as:
- vertical - extension and flexion;
- frontal - removal;
- horizontal - physiological movements are made exclusively with a bent leg;
- rotation.
Type of movement Normal inclination angle, ° Flexion 40 Extension 180 Rotation 40
The knee works only when all elements function in harmony. The dynamic stabilizer of the patella is the quadriceps, which extends the leg. The semitendinosus and semimembranosus muscles prevent the development of anterior drawer syndrome, protect the menisci and the posterior region of the fibrous bursa.
The cartilage discs are tightly fused to the ligaments, which strengthens the capsule on the posterior side and prevents excessive rotational forces. The cruciate ligaments, which produce movements in the frontal plane, provide rolling and gliding when bending. The medial collateral ligament stabilizes the knee during abduction, and the lateral ligament prevents excessive expansion of the joint spaces.
The knee is one of the large joints of the human body. Due to the size of the joint, the knee can withstand maximum loads. The structural features of the joint allow a person to move and walk.
The anatomical structure of the knee joint is quite complex, and therefore the knee is very vulnerable, susceptible to mechanical injuries and pathological processes.
Anatomy of the knee
The basis of the structure of the knee joint is the articulation of two main bones - the femur and the tibia. The thickened ends of the bones are called condyles. The condyles are covered with smooth hyaline cartilage, which facilitates the sliding of bones in the joint. The third bone of the knee joint is the patella (kneecap), located in the thickness of the tendon of the femoral muscle.
The bone elements are surrounded by a cartilaginous plate. This is a formation whose thickness is 5-6 mm. The structure of cartilage is smooth and elastic, resulting in ideal conditions for ensuring the functionality of the joint.
All bony parts of the joint are held together by ligaments. There are many of them, they are located both in the articular cavity and outside it. Main ligaments of the knee joint:
- collateral (tibia and fibula);
- popliteal (arcuate and oblique);
- medial;
- lateral;
- patellar ligament;
- cruciform (front and back).
Ligaments unite the elements of the joint into a single whole, at the same time making the joint not a monolith, but a movable joint.
Outside, the joint is surrounded by a connective tissue capsule, which has 2 membranes: outer (fibrous) and internal (synovial). The inner membrane forms folds and turns (bursae) in several places in the articular cavity. The bursae produce joint fluid, which provides lubrication and nutrition to the cartilage.
The anatomy of the knee joint bursa is complex, but thanks to it, a person has the ability to walk, jump and sit down.
Menisci
The structure of the human knee joint also includes menisci - cartilages that ensure uniform distribution of body weight. The location of the menisci is between the ends of the femur and tibia.
Meniscus tissue is more elastic than hyaline cartilage tissue. In fact, the meniscus is a kind of pad that ensures the full functioning of the knee.
Muscle corset
Movements in the knee joint are impossible without the participation of muscles. The muscles of the knee joint provide the main function of the leg - walking. All muscles adjacent to the knee are divided into 4 groups.
- Group that provides flexion of the lower leg: biceps, semimembranosus and semitendinosus muscles of the thigh; tailoring; gastrocnemius; popliteal; thin.
- Extensor muscle group: quadriceps femoris; rectus, intermedius, lateral and medial muscles of the thigh.
- Group performing pronation (inward rotation of the hip): popliteus muscle; tailoring; thin.
- Group providing hip supination (outward rotation): biceps femoris muscle; partially calf muscle.
The coordinated activity of all these muscles is made possible by the innervation of the knee joint.
Innervation of the knee joint, that is, the provision of all its cells and tissues with nerve fibers, is carried out with the participation of the following nerves:
- The ischial, popliteal, tibial and fibular joints perform the function of maintaining the sensitivity of the knee joint.
- The popliteal nerve is divided into the peroneal and tibial nerves.
- The tibial nerve runs along the back of the knee and is attached by branches of the knee joint.
- The peroneal nerve is located on the front of the kneecap.
- The nerve fibers of the meniscus intertwine with the blood vessels of the knee. Pass through the entire cartilaginous body.
Pathology of the sesamoid bones of the foot
A common foot disease among dancers is sesamoiditis. There are also bifurcated sesamoid bones, which can be either congenital or post-traumatic.
On the plantar side of the metatarsophalangeal joint of the first toe, in the structure of the flexor apparatus there are two small bones smaller than a pea. Despite the fact that the bones are very small in size, they play a huge role during walking, running, jumping and other stress on the foot. If the sesamoid bones are involved in any pathological process, they become a source of severe pain, significantly worsening the patient’s quality of life.
Anatomy
At the base of the first toe is the first metatarsophalangeal joint, which is important from a functional point of view. Two small sesamoid bones are located on the plantar side of this joint: one is located on the inside, the other on the outside. The sesamoid bones are located inside the flexor tendons of the first finger.
These structures together form the flexor apparatus of the first toe. Since the first finger bears heavy loads, these loads are performed due to the flexion apparatus. Sesamoid bones increase the leverage of the flexor tendons on the phalanges of the first finger, and also reduce the force of friction between the tendons and soft tissues in the position of extension of the first finger.
Causes
Pain syndrome can develop for various reasons. One of the reasons is overload of the ligamentous apparatus of the sesamoid bones. This condition may be called sesamoiditis. Overload most often develops after excessive running or dancing.
Another cause of pain associated with the sesamoid bones is fractures. Fractures can occur when landing directly on the first metatarsophalangeal joint of the foot. So-called stress fractures of the sesamoid bones may also occur. Stress fractures occur due to constant exposure to large loads on the sesamoid bone apparatus. This is typical for athletes; athletes are most often affected.
Another reason is arthrosis of the joint between the head of the first metatarsal bone and the sesamoid bones. When the big toe moves, the sesamoid bones slide anteriorly and posteriorly along the plantar surface of the head of the first metatarsal bone. Like other joints in the body, this joint can develop arthrosis.
Arthrosis in this joint is typical for patients with a high longitudinal arch of the foot. With a high longitudinal arch of the foot, the apparatus of the sesamoid bones is under greater tension and the joints of the sesamoid bones are subject to greater load. Eventually, the cartilage of the sesamoids and the head of the first metatarsal begins to deteriorate.
https://www.youtube.com/watch?v=8-kQ8OHfTYg
A rare cause is a disruption of the blood supply to the sesamoid bones, resulting in disruption of the bone structure. This condition is called avascular necrosis of the sesamoid bone. In this case, calcium deposits may additionally form in the soft tissues around the first metatarsophalangeal joint.
Sometimes pain from the plantar surface comes from additional soft tissue formations under the big toe. For example, plantar keratosis can cause pain on the plantar aspect of the first metatarsophalangeal joint.
Symptoms
Patients with pathology of the sesamoid bones usually feel aching pain from the plantar surface of the metatarsophalangeal joint of the first toe. When touched from the plantar side, the pain intensifies. Movement in the thumb joint is often limited. Patients notice that when walking, the pain intensifies before the foot pushes off for the next step.
Diagnosis
The doctor will ask many questions about the development of the disease. You will be asked about your current complaints and past foot problems. The doctor will examine your feet. The examination may be a little painful, but it is necessary to identify painful points and check the movements of the fingers. The patient may be asked to walk around the room.
It is mandatory to take an x-ray (x-ray). Several projections are performed. One of them is the axial one, on which the sesamoid bones are clearly visible. This projection requires special placement and the X-ray beam comes at an angle.
An x-ray may reveal that the sesamoid bone is composed of two or more separate bones, as if it were a fracture, but the boundaries between them are smooth. This is normal and can occur in every tenth person. The x-ray evaluates the position of the sesamoid bones, as well as the space (articulation) between the metatarsal head and the sesamoid bones. The joint space normally appears uniform on x-ray. Narrowing and unevenness indicate pathology.
If it is difficult to judge the presence of a sesamoid fracture from a plain X-ray, a scan may be ordered. This is a test in which a special solution, a contrast agent, is injected intravenously. The contrast agent accumulates in the bone tissue in a certain way. By scanning the human skeleton with X-rays, special images are created that reflect the accumulated X-ray contrast agent.
If there is a pathological focus in the bone tissue, then the pattern of accumulation of the contrast agent will look different. Each pathological process has its own unique pattern of contrast agent accumulation. In this way, a fracture can be distinguished from a congenital separation of the sesamoid bone.
To obtain the most complete picture of the disease, magnetic resonance imaging (MRI) may be necessary. Using MR images, you can study the relationships between the anatomical structures of the foot and exclude other pathological processes, including infection.
Treatment
Conservative treatment
As a rule, treatment begins with conservative methods. Typically, in this case, nonsteroidal anti-inflammatory drugs (NSAIDs), such as diclofenac, indomethacin, and ibuprofen, are recommended. These remedies usually relieve pain and inflammation well. You can try using special insoles that ease the load on the first metatarsophalangeal joint.
Be sure to avoid using high-heeled shoes. The higher the heel, the greater the load on the forefoot, and therefore on the painful metatarsophalangeal joint. In some cases, your doctor may suggest injecting a steroid into the painful area. This usually helps relieve severe pain.
If there is a sesamoid fracture without a rupture of the extensor apparatus, wearing a plaster or plastic splint for approximately six weeks is recommended. After this, the patient must wear hard-soled shoes. The rigid sole holds the toe in a straight position, preventing the foot from rolling, thus relieving the load on the flexion apparatus.
Stress fractures and aseptic necrosis of the sesamoid bone are less responsive to conservative treatment. Some doctors recommend a plaster or plastic splint for up to eight weeks without putting any weight on the leg. If after prescribing conservative treatment it does not get better within 8-12 weeks, then surgery is most likely necessary.
Surgical treatment
Removing the sesamoid bone Your doctor may suggest removing part or all of the sesamoid bone. When the sesamoid bone is partially removed, the other sesamoid bone is able to provide a fulcrum for the flexors. However, if both bones are removed, the flexors will not be able to function normally and the first toe will become claw-shaped. Therefore, surgeons usually avoid removing both sesamoid bones.
When the sesamoid bone is fractured, surgery is performed to remove non-functional fragments and restore the integrity of the flexor apparatus. For stress fractures in athletes, when the most complete recovery is needed, surgery can be performed using bone grafts.
Rehabilitation
Rehabilitation after conservative treatment If the pain syndrome is mild, the doctor may allow you to continue daily activities immediately, but with the condition of using shoes with hard soles. If the disease is moderate, you will need to use crutches and not put any weight on your leg for a period of several days to two to three weeks.
Physical therapy can help reduce pain and swelling. If there are no contraindications, then ultrasound and thermal procedures are prescribed. Sometimes the use of anti-inflammatory ointments and creams is combined with physiotherapy.
Rehabilitation after surgery After surgery, most patients are advised to use crutches and avoid putting weight on the leg. For those who have undergone restoration of the flexor apparatus of the first toe or bone grafting, immobilization with a plaster or plastic splint is recommended.
Physical therapy exercises are required. Depending on the operation performed, exercises begin at different times after the operation, gradually increasing the load and complexity. Therapeutic exercise is necessary to restore and maintain muscle tone of the lower leg and foot.
Symptoms
Patients with pathology of the sesamoid bones usually feel aching pain from the plantar surface of the metatarsophalangeal joint of the first toe. When touched from the plantar side, the pain intensifies. Movement in the thumb joint is often limited. Patients notice that when walking, the pain intensifies before the foot pushes off for the next step. From time to time, the first metatarsophalangeal joint may become stuck or click, which increases pain. After rest, the pain goes away or weakens. Some patients report numbness in the area of the first and second toes.
Notes[edit]
- ↑ Tim D. White, Human Osteology, 2nd edition (San Diego: Academic Press, 2000), 199, 205.
- ↑ White, Human Osteology, 2nd edition, 257–261.
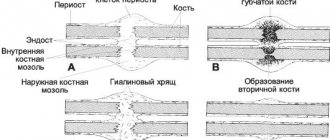
This is a draft article on anatomy. You can help the project by adding to it. Musculoskeletal system, connective tissue: bone and cartilage Cartilage Cartilaginous growth perichondrium, callus, epiphyseal plate Chondroblast cells, chondrocyte Types of cartilage tissue hyaline, elastic, fibrous Bones Ossification endesmal, endochondral Cells osteoblast, osteocyte, osteoclast Types of bone tissue spongy, compact Divisions subchondral bone, epiphysis, metaphysis, diaphysis Structure osteon, Haversian canals, Volkmann canals, endosteum, periosteum, bone marrow, pneumatization Form long, short, flat, sesamoid, mixed