What is ankle bursitis?
Inflammation of the ankle joint occurs due to overuse
The ankle joint is exposed to stress every day during movement. Any injuries and bruises of this joint are potentially dangerous for the development of bursitis of the ankle joint - inflammation in the bursa or synovial bursa.
There are 4 of them in the ankle - two of them are in the area of the heel bone, one is located at the junction of the Achilles tendon with the heel bone, and one is located directly on the sole. The exact name of ankle bursitis depends on the location of the inflammatory process. In the vast majority of cases, people experience inflammation of the Achilles tendon or heel bursa, since these areas are most susceptible to injury during movement.
With ankle bursitis, the symptoms are quite specific, which allows for self-diagnosis. Having noticed the symptoms of the disease, you should immediately begin treatment and not delay it, as the disease greatly impairs the quality of life and can lead to complications.
Causes and predisposing factors
There are many reasons for the development of ankle bursitis. For example, these may be chronic diseases, against the background of which the shell of the joint capsule loses its strength and is more easily damaged under the most ordinary circumstances (for example, when changing shoes).
But more often, pathology occurs as a result of injury (impact, bruise) or penetration of infectious pathogens (through a wound or through blood vessels, from distant foci).
The main reasons for the development of pathology:
- Traumatic tissue damage (impacts, bruises, cuts).
- Defects in the structure of the foot (flat feet, weakness of the ligaments).
- Infections (syphilis, streptococcal and staphylococcal infections).
- Joint diseases (psoriatic, gouty, rheumatoid arthritis, arthrosis).
- Purulent inflammation of adjacent tissues (osteomyelitis, abscess).
- Metabolic disorders (diabetes mellitus, gout).
- Systemic connective tissue diseases (scleroderma).
Sometimes the cause of bursitis cannot be determined, and it is considered idiopathic (arising for unclear reasons).
Predisposing factors play an important role (they weaken the bursa tissue and increase the likelihood of damage):
- poor posture and structural defects of the musculoskeletal system (spinal deformity, shortening of one leg);
- natural aging of tissues (after 60 years);
- excess weight;
- allergy;
- weakened immunity;
- poisoning with toxins and drugs (chronic alcohol intoxication, long-term use of corticosteroids);
- physical and household stress;
- uncomfortable shoes;
- profession (dancers, athletes);
- hypothermia (hypothermia).
Flat feet (pictured) may be one of the reasons for the development of bursitis
Reasons for development
The ankle is subject to constant stress and is often injured
The main reason for the development of bursitis of the ankle and foot is excessive stress on the joints. This happens in the following cases:
- being overweight;
- intense sports activities;
- standing work.
All these factors disrupt the normal distribution of load on the ankle and foot and can lead to the development of bursitis. Also, pathology often develops against the background of injuries and bruises. In this case, the cause of the disease is a violation of metabolic processes in the joint capsule, which leads to the accumulation of synovial fluid and the development of the inflammatory process.
Bursitis can be a complication of other joint pathologies. It accompanies arthritis and arthrosis. Post-traumatic bursitis of the Achilles tendon or heel bursa is observed in professional athletes involved in jumping.
- Most often, ankle bursitis is associated with wearing ill-fitting shoes. Narrow high-heeled pumps, flat-soled ballet shoes, shoes made of low-quality fabrics or small sizes - all this compresses the bursa and leads to an inflammatory process.
Separately, infectious bursitis is distinguished. They develop due to infection of the synovial bursa. This happens in two ways - when an infection enters the bursa through the bloodstream, or when the tissue around the bursa is damaged and becomes infected.
Infectious bursitis can be specific or nonspecific. Nonspecific inflammation is caused by opportunistic microorganisms. These can be staphylococci, streptococci, less often - Escherichia coli and Pseudomonas aeruginosa, yeast fungi. Infection occurs due to the presence of a chronic focus of infection.
Purulent bursitis or abscess of the bursa is most often caused by Staphylococcus aureus.
Infection often occurs against the background of damage to the integrity of the skin around the bursa, or due to chronic infectious diseases. Purulent bursitis can be caused by boils on the skin of the feet and legs.
Specific inflammatory processes in the bursa develop with gonorrhea, syphilis or tuberculosis. Inflammation is associated with the penetration of pathogens of these diseases into the joint capsule; infection occurs through the hematogenous route. Such forms of the disease are very dangerous, since without treatment, pathogenic agents will continue to move throughout the body, affecting more and more bursae, joints and even bones.
Ankle: injuries, treatment, orthopedics
The ankle joint plays an important role in the static-dynamic balance of a person, concentrating on itself the entire weight of the body’s support.
The ankle is a movable joint of three bones: the tibia, fibula and talus. This structurally complex joint takes on a significant load, so pain and injuries associated with the ankle are common. Most often, ankle problems occur in people of working age and athletes. According to the International Olympic Committee, ankle joint injuries account for one fifth of all sports injuries of the lower limb and rank third in frequency among athletes, along with injuries to the shoulder and lower leg.
You can injure your ankle while playing sports, or simply by slipping on ice, tripping, or unsuccessfully leaning on your leg. Injuries, dislocations, and repeated subluxations can lead to the formation of chronic instability of the ankle joint, which significantly reduces a person’s quality of life. Traumatologists, physiotherapists and rehabilitation specialists from all over the world pay great attention to the problem of treating injuries to the ankle joint.
Types of Ankle Injuries
The ankle joint is surrounded by a complex system of ligaments and tendons. Their function is to stabilize the ankle joint, as well as to direct movement in it.
You can damage your ankle ligaments if you exercise too intensely. Such injuries often accompany athletes (football players, basketball players), paratroopers (at the moment of landing), and dancers. In everyday life, you can damage your ankle when you place your foot poorly, fall, or get hit. Ankle sprains can occur, for example, due to frequent walking in high heels. In this case, excessive supination of the foot occurs - overstrain of the muscles of the foot and lower leg due to a shift in the center of gravity.
The ligaments of the ankle joint have low elasticity and during an injury there is not stretching, but rather tearing of their fibers to varying degrees, up to complete rupture. The diagnosis of ankle joint injuries is made based on the nature and mechanism of the injury, the clinical picture, and a mandatory x-ray.
Three degrees of ligament damage:
Damage I degree
Stretching (microscopic tears) of the ligament, causing local pain and minimal swelling; joint mobility in this type of injury is slightly impaired, stability is preserved. In this case, the load with body weight is bearable, and there are no deviations from the norm on radiographs.
Damage II degree
A severe sprain and partial tear of the ligament that causes significant tenderness, moderate swelling and pain with exercise, and loss of stability and mobility of the joint. Radiographs in standard projections are not very informative. However, when the position of the foot changes, a loss of ligament function is detected, which is determined by the abnormal position of the talus in the joint.
Damage III degree
Complete ligament rupture. The patient is unable to bear weight; There is pronounced swelling, which causes joint contracture and severe instability in the first hours after injury. Severe pain or loss of nerve function. Standard radiographs reveal a violation of the relationship of the talus in the articular fork.
Rehabilitation
For the treatment of ankle pathologies, two types of treatment are used: conservative and surgical treatment. The most commonly used is so-called conservative treatment.
Treatment consists of three phases:
Acute phase (protection)
In this phase, inflammation, swelling and pain are observed. Therapeutic measures are: control of edema, inflammation, pain, hardware physiotherapy, immobilization (plaster, orthosis), passive movements and massage (subject to restrictions for this type of injury), static muscle tension.
Movement recovery phase
Inflammation and pain are reduced. For rehabilitation, they carry out: control of edema, hardware physiotherapy, functional orthotics, development of range of motion, transverse massage, muscle retraining, balance and coordination training, activation of local muscles of the foot, strengthening and increasing endurance of key muscles.
Functional phase
There is no inflammation, pain is present only at the end of the range of motion. To complete the treatment, the following is carried out: control of swelling after exercise, muscle stretching, functional orthotics during exercise, physical therapy exercises, exercises.
Types of ankle orthoses
Fixation of the ankle joint is an essential part of rehabilitation therapy. To support the damaged joint in the correct position, special products are used - orthoses.
There are orthoses with light, medium and high degrees of fixation. Light fixation orthoses are used for mild injuries, when returning to sports after surgery, as well as for preventive purposes. Orthoses with a high degree of fixation are used for combined and severe trauma, or after complex operations, including suture of the Achilles tendon. Medium fixation orthoses are universal and suitable for most situations where protection of the capsular-ligamentous structures of the joint is required.
Orthoses are divided according to the degree of fixation:
Easy fixation
Orthoses made of special elastic fabric without stiffeners or inserts. Similar bandages are used for bruises, sprains, dislocations, and they are also used in sports to reduce the load on the joint. The elastic bandage is invisible under clothing, does not require changing shoes and can be worn around the clock, including by children.
Medium fixation
Products made of elastic material with stiffening ribs. They are used by people with chronic ankle instability, for moderate injuries and during the rehabilitation period after surgery. In addition to moderate stabilization, such orthoses will have massage and compression (warming) effects, which contribute to the restoration of the joint.
Semi-rigid fixation
An elastic and durable product with stiffening ribs and additional fixing inserts. Fixation is adjusted depending on individual parameters and can change during the rehabilitation period. For this, lacing or Velcro fasteners are used. Semi-rigid ankle orthoses are used for injuries, severe ankle instability, flaccid foot paralysis and other pathologies.
Rigid fixation
Provides complete immobilization of the foot. For this degree of fixation, a rigid base made of medical plastic, rigid inserts, and a lining (in the form of a boot) are used. The basis of such orthoses is carefully thought out. The design contains recesses that help adjust the orthosis to the user and create additional air exchange.
The linings are made of soft materials with good breathability, so that the user feels comfortable even when wearing the orthosis for a long time. The covers are removable - easy to put on and convenient to clean.
Thanks to the presence of a hinge, you can set the flexion-extension angle at the ankle joint in a selected range. The rubber outsole provides stability and anti-slip protection.
Symptoms of ankle bursitis
Tendon swelling, redness and pain are signs of bursitis
The main symptom of any bursitis is pain. When the ankle joint is affected, the specific manifestations of the disease will depend on the exact localization of the inflammatory process.
When the Achilles tendon becomes inflamed, the following occurs:
- severe swelling of the tendon;
- pain when walking;
- redness of the skin in the area of inflammation;
- local increase in epidermal temperature.
As a rule, pain with achillobursitis intensifies while walking. This occurs due to compression of the swollen bag by the heel of the shoe. During movement, the foot rises slightly, and the inflamed area rubs against the shoe, which increases inflammation and aggravates the pain.
Symptomatic manifestations of articular bursitis of the ankle joint under the heel are severe pain. The swelling is not visible outwardly, since the bursa is hidden behind the bone. The pain intensifies with any load on the foot. The same symptoms are characteristic of inflammation of the bursa on the sole.
Treatment for ankle bursitis depends on the type of inflammation and symptoms. With purulent bursitis, severe swelling and pain when pressed are observed. The skin temperature in the inflamed area increases significantly, the pain syndrome is acute, pulsating, and does not go away at rest. With an abscess and purulent inflammation, body temperature also rises, there are symptoms of intoxication, severe headache and fatigue. This form of the disease is very dangerous and requires timely treatment.
Why is bursitis dangerous?
Thickening of the bursa can lead to disruption of local metabolic processes
Bursitis can become chronic. This is accompanied by a temporary subsidence of symptoms, however, with any stress or compression of the bursa, the pain will return. Chronic inflammation is dangerous due to the thickening of the bursa, which leads to disruption of local metabolic processes. Against this background, the functionality of the joint deteriorates, degenerative-dystrophic changes in the cartilage and inflammation in the joints may develop. When the walls of the bursa are thickened, surgical excision of the altered tissues or complete removal of the bursa is practiced.
Infectious arthritis is especially dangerous because pathogenic microbes can spread to the joints and surrounding tissues. With purulent inflammation or an abscess, there is a risk of infection of the entire body due to the entry of purulent masses into the general bloodstream, which leads to sepsis.
Diagnosis of bursitis
There are several methods for diagnosing bursitis.
A characteristic sign of ankle bursitis, the symptoms and treatment of which depend precisely on the location of the inflammation, is swelling, noticeable in the photo, and pain is always present. The appearance of these two signs should force the patient to urgently consult a doctor.
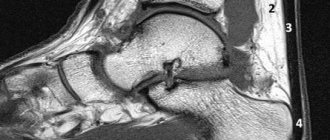
To make a diagnosis:
- visual inspection;
- palpation of the diseased area;
- radiography of the joint;
- MRI;
- puncture.
An experienced doctor can make a preliminary diagnosis only based on examination and palpation. X-rays are necessary to exclude other articular pathologies, such as arthritis and arthrosis; MRI is done in order to obtain a complete picture of the condition of the soft tissues and bursa.
A puncture is performed to collect a sample of synovial fluid from the inflamed bursa.
The liquid is then examined under a microscope for pathogenic microorganisms. This method allows you to accurately determine the nature of inflammation.
Drug treatment
The medicine is prescribed after bacterial culture of the synovial fluid.
Drug treatment of ankle bursitis is carried out using the following drugs, which should be prescribed by the attending physician:
- non-steroidal anti-inflammatory drugs;
- decongestants;
- glucocorticosteroids;
- antibiotics.
Treatment begins with the prescription of non-steroidal anti-inflammatory drugs - Diclofenac, Ibuprofen or analogues. These remedies quickly relieve symptoms, reduce pain and inflammation. They are used in various dosage forms - tablets, injections, ointments. However, such drugs do not cure bursitis, but only relieve its symptoms.
For severe swelling, glucocorticosteroid therapy is used. These medications are administered by injection directly into the joint capsule; tablets are less commonly prescribed. Drugs in this group quickly and effectively relieve inflammation and eliminate swelling.
Antibiotics are prescribed only when the infectious nature of the inflammation is confirmed.
The choice of drug depends on the causative agent of the disease. The medicine is prescribed only after bacterial culture of the synovial fluid and determination of sensitivity to antibiotics.
Treatment of bursitis
Treatment for any bursitis depends on whether it is infectious or not. Septic bursitis requires treatment with antibiotics, often intravenously. Aspiration of fluid from the bursa may be necessary—removing fluid with a needle and syringe under sterile conditions.
In addition, septic bursitis requires further monitoring and treatment. Repeated aspirations, surgical drainage, and even, in rare cases, removal of the inflamed bursa (bursectomy) may be required.
With chronic bursitis, it is sometimes necessary to remove calcium deposits if they are large enough, cause constant discomfort or interfere with movements.
For non-infectious bursitis, corticosteroid injections into the bursa may also be used, sometimes at the same time as aspiration. But most often in this case, a rest regimen, anti-inflammatory and painkillers (if necessary) are recommended. For aseptic bursitis, ice compresses can be used. Sometimes, instead of cold, heat (a heating pad, warming ointment) or alternating cold and hot compresses helps better bursitis
The therapeutic anti-inflammatory analgesic patch NANOPLAST forte has shown high effectiveness in the treatment of bursitis - primarily in non-infectious bursitis.
Surgical methods of treatment
Antibacterial therapy prevents recurrence of infection
With an abscess in the ankle, therapy and treatment of ankle bursitis are aimed at cleansing the bursa from purulent masses. To do this, an incision is made and the bursa is thoroughly cleaned using special instruments. Antibacterial therapy is then carried out to prevent recurrence of the infection.
When the walls of the bursa are thickened due to chronic inflammation, surgical excision of tissue is practiced.
Prevention
The following measures to prevent the disease will help prevent the development of ankle bursitis:
- protection of the foot and ankle with braces and compression socks;
- warm-up exercises before exercise (before sports training, dance rehearsals, hard work);
- comfortable everyday shoes with low speed and sports shoes with a special shock-absorbing sole;
- getting rid of excess weight;
- treatment and prevention of diseases that can cause bursitis (chronic infections);
- daily relaxing ankle and foot massage;
- a set of physical therapy exercises (to strengthen and stretch the muscles of the joint).
Folk remedies
In addition to drug treatment, you can use traditional medicine recipes
For ankle bursitis, treatment with folk remedies can be used in addition to drug therapy. It is recommended to use such methods only after the approval of a doctor.
Traditional methods and folk methods for treating ankle bursitis:
- cold compresses with ice and improvised means;
- white cabbage leaves;
- propolis tincture for rubbing;
- propolis ointment.
Cold compresses help relieve swelling.
You can apply ice, frozen foods, or chilled glass to the affected area. The main condition is indirect exposure, that is, the cold object is first wrapped in a towel. Keep the compress for 15 minutes. You can do this 3-4 times a day.
White cabbage leaves are first kneaded with your fingers and applied to the sore joint overnight. To prepare propolis ointment, you need to slowly dissolve 10 g of the product in butter simmering in a water bath. The ointment should be applied twice a day.