Composition and release form
The medicine is available in several forms:
- pills;
- ointment;
- gel;
- candles;
- children's oral suspension.
The active substance is ibuprofen.
Auxiliary components in the tablets: potato starch, magnesium stearate, beeswax, sucrose.
Additional gel ingredients: ethanol, lavender oil, water.
Excipients in the ointment: macrogol.
Additional components of candles: solid fat.
History of ibuprofen
Of all the anti-inflammatory drugs, what is remarkable about ibuprofen is that it was discovered as part of the search for a treatment for rheumatoid arthritis (a joint disease).
In the 1950s, steroids—hormonal drugs—were the only way to relieve symptoms and reduce inflammation. Then the young scientist Stuart Adams was given an ambitious goal - to find a new alternative to steroids that could compete with them in effectiveness, but at the same time have a higher safety profile in terms of side effects.
After a thorough ten-year research search, only a few chemical compounds were approved for clinical trials by a team of scientists led by Stuart Adams. Among them was a substance that we know today as ibuprofen. Research into the substance began in the UK in 1953, and 16 years later it was approved as a prescription drug to reduce pain and inflammation in rheumatoid arthritis. Since the 80s of the last century, ibuprofen began to be used to relieve fever and fever, in 1983 it received over-the-counter status and went on mass sale as an anti-inflammatory, antipyretic and analgesic drug.
When to take medicine
The medicine in tablet form is effective for the following conditions:
- inflammatory processes in the spine and joints;
- moderate pain of various origins (menstrual, headache, toothache, pain after surgery);
- fever caused by a cold infection.
Gel and ointment should be used in the following cases: osteoarthritis, arthritis, gout and other diseases of the musculoskeletal system.
Suppositories and syrup are usually prescribed to children to reduce body temperature, for various childhood infections and to reduce pain (in the head, throat, ear).
Ibuprofen in the practice of a general practitioner: possibilities for relieving pain syndromes
Pain syndromes of various origins are often encountered in the daily practice of a general practitioner, which determines the growing need for effective painkillers. According to the independent research center DSM Group, an analysis of the pharmaceutical market in 2012 showed that painkillers were one of the most popular groups of pharmaceuticals [1]. Analgesics are the most widely demanded category of drugs in the pharmaceutical market [2].
The feeling of pain is familiar to every person. There are probably no people who would not experience a feeling of pain during their lives. The variety of causes of pain determines the high frequency of patients visiting a doctor for this reason. It should be noted that the prevalence of pain syndromes in recent years, despite the development of pharmacy, has not decreased at all [3], on the contrary, there is even a tendency towards its increase, especially for chronic pain [4].
Verification of the cause of pain is one of the keys to its successful treatment. Among pain syndromes, the largest percentage is headaches, the prevalence of which reaches 90% in the population. Among them, tension headaches (up to 60%) and migraines (up to 23%) undoubtedly dominate. A global health survey conducted in 54 countries with 27,000 respondents found that headaches were the most common reason for seeking medical care and taking medications (Figure 1). The prevalence of primary headache in Russia (2725 respondents from 35 cities) reaches 62.9% with some predominance in the urban population, and more than 10% have headaches for more than 15 days a month. 68.1% of respondents indicated self-use of over-the-counter medications [5]. Headaches are the most common health complaint among drug users around the world.
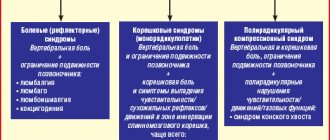
The top ten complaints, along with headaches, also include back pain, sore throat and other types of pain. About 20% of the adult population suffers from recurrent back pain lasting more than three days, of which 20% have pain that lasts more than a month and is chronic. An equally acute problem is muscle pain, which generally occurs in 30–85% of the population. In this case, myalgia can accompany vertebrogenic back pain (in 60% of patients), but can also be primary [6].
The increase in the prevalence and incidence of pain syndromes is associated with both lifestyle changes and the general aging of the population (Fig. 2).
The main trend in patient preferences is the possibility of self-medication, i.e., independent choice of anesthetic. Therefore, as data from epidemiological studies show, most patients with the most common forms of pain syndromes remain outside the attention of specialists. Thus, only about 10% of patients with back pain seek help from specialists. A similar situation occurs with headaches. Thus, among patients with one of the most common forms of cephalgia - migraine - only 1/6 of them turn to specialists, the rest of the patients are outside their field of vision, preferring to be treated independently [6].
Economic burden of pain syndromes
The increasing prevalence of pain syndromes in the population is a significant burden for workers, employers and society, leading to loss of profits and additional costs and payments [8]. A paradox in the pharmacoeconomics of pain is that cost is a potential barrier to optimal pain management, with even suboptimal pain management showing an increase in overall healthcare costs [9].
Thus, in the USA alone, annual costs aimed at pain relief, as well as legal costs and compensation associated with pain syndrome, are estimated at almost 100 billion US dollars [10]. And, for example, in Sweden, the average annual cost of treating diseases associated with chronic pain syndrome (n = 840,000) is 6,400 euros per patient. The majority of costs (59%) are indirect costs (sick leave payments and early retirement), while the cost of analgesics is only about 1%. Overall, the socioeconomic burden of diseases associated with chronic pain syndrome in Sweden alone reaches 32 billion euros per year [11].
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Practical experience shows that NSAIDs are most often used to relieve subjective pain. The presence of universal mechanisms of pain makes it possible to use drugs from this group in various clinical situations. In Europe, NSAIDs are prescribed by 82% of general practitioners and 84% of rheumatologists in polyclinics; in hospitals they are used in 20% of patients [12].
Thanks to the studied analgesic, anti-inflammatory, and antipyretic mechanisms of action, various representatives of NSAIDs have found wide practical use.
NSAIDs are able to relieve pain of various localizations - in the musculoskeletal system, headaches, dental pain, menstrual pain. In addition, all NSAIDs have antipyretic and anti-inflammatory properties. The variety of therapeutic effects of NSAIDs, as well as the high prevalence of clinical situations in which they are effective, make drugs in this group the most frequently prescribed to patients. The need for NSAIDs is especially increasing in older people, who often have concomitant diseases.
The main effects of NSAIDs are associated with the mechanism of suppression of the activity of cyclooxygenase (COX), an enzyme that regulates the conversion of arachidonic acid into prostaglandins, prostacyclin and thromboxane. Differences in the severity of anti-inflammatory, analgesic effects and toxic effects of drugs of this class are associated with their different ability to influence two isoforms of COX - COX-1 and COX-2. The analgesic and anti-inflammatory effects are mainly associated with the inhibition of COX-2, and the development of side effects is associated with the suppression of COX-1. Therefore, the choice of a specific representative is determined by its ability to predominantly influence COX-2.
Analgesic efficacy profile of ibuprofen
One of the most well-known representatives of the NSAID class is ibuprofen, which has been successfully used in clinical practice for more than 30 years and for more than 10 years in over-the-counter form (Nurofen). The high clinical effectiveness of this drug is confirmed by the high demand for it among consumers. Thus, only in the last six months, in terms of share of sales value in Russia, the drug Nurofen has moved from 8th to 3rd place, while occupying a leading position in Moscow [13].
The analgesic effectiveness of ibuprofen has been convincingly proven in various models of pain: toothache [14–16], headache [17–23], sore throat [14], musculoskeletal pain [14–16], etc.
Toothache is well recognized and sensitive enough to evaluate the analgesic effect of drugs. Ibuprofen at a dosage of 200–400 mg is the “gold standard” for the treatment of moderate pain in postoperative dental pain [14]. A meta-analysis demonstrated that ibuprofen was more effective than placebo across 72 studies. Ibuprofen significantly reduced pain in all patients by at least 50%, for an average of 4.7 hours. Repeated analgesia was required in only 48% of patients taking ibuprofen at a dose of 200 mg and in 42% of patients taking ibuprofen at a dose of 400 mg [15]. Another meta-analysis, based on 33 studies, found an advantage of ibuprofen (400 mg) in relieving pain after tooth extraction compared to paracetamol (1000 mg), as well as a combination of paracetamol (600-650 mg) and codeine (60 mg) [ 16].
For headaches, ibuprofen as a first-line drug is included in the list of analgesics recommended by WHO, as well as the European Federation of Neurological Societies (EFNS) for the treatment of mild to moderate migraine attacks (class A) [17, 18]. The effectiveness of ibuprofen in the treatment of cephalgia has been proven in many placebo-controlled clinical trials, as well as several meta-analyses, including in children and adolescents [19–23].
For sore throat due to tonsillopharyngitis, a double-blind, randomized, multicenter study compared the analgesic efficacy of ibuprofen (400 mg) or paracetamol (1000 mg). The severity of pain when swallowing, difficulty swallowing, and changes in pain intensity were assessed every 6 hours after taking the first dose of drugs. Ibuprofen, compared with paracetamol, was significantly more effective in influencing the severity of pain and difficulty swallowing, while the effect of ibuprofen began significantly earlier than that of paracetamol. Treatment tolerability was comparable in both groups, and no serious side effects were observed during the study. Thus, the study showed that ibuprofen is a more effective alternative to paracetamol in the treatment of sore throat [24].
Ibuprofen, having high efficiency and low toxicity, is widely used in the long-term treatment of various inflammatory and degenerative diseases of the musculoskeletal system.
The effectiveness of ibuprofen and its benefits have been repeatedly demonstrated in large-scale studies. An illustrative example is the multicenter randomized IPSO (Ibuprofen, Paracetamol Study in Osteoarthritis) study conducted in 2004 involving 222 patients suffering from osteoarthritis (OA) of the hip (30% of patients) or knee (70%) joint. For two weeks, the WOMAC (Western Ontario and McMaster Universities osteoarthritis index) scale assessed the effect of ibuprofen (400–1200 mg/day) and paracetamol (1000–3000 mg/day) on the severity of pain and joint syndromes. The results of the study showed a greater reduction in pain in the first 6 hours after taking the drug and a more pronounced further reduction within 14 days in the ibuprofen group compared to paracetamol. The authors concluded that ibuprofen with a single (400 mg) or multiple (up to 1200 mg) dose has a better efficacy/safety ratio than paracetamol [25]. The greater effectiveness of NSAIDs, including ibuprofen, compared with paracetamol in the treatment of OA was also demonstrated in a Cochrane review [26].
According to current recommendations, the use of NSAIDs as symptomatic treatment is recommended for all patients with rheumatoid arthritis (RA). Patients with OA are recommended to take NSAIDs only during periods of increased pain and in lower dosages than for inflammatory arthritis [27, 28].
Ibuprofen can be used both in monotherapy and as part of combination therapy in combination with other drugs. Thus, adding the centrally acting muscle relaxant tizanidine to ibuprofen can not only increase the effectiveness of therapy, but also reduce the incidence of adverse events from the use of NSAIDs. Tizanidine has a protective effect on the gastric mucosa from the effects of NSAIDs [29]. This effect was convincingly demonstrated in the work of Berry H. et al., which studied the addition of tizanidine 4 mg to ibuprofen 400 mg three times daily in patients with acute low back pain. The overall effectiveness of treatment in both groups was almost the same, but the safety of treatment was higher with the combined use of ibuprofen and tizanidine. Patients receiving ibuprofen/tizanidine combination therapy reported significantly less gastrointestinal (GIT) side effects compared to the placebo/ibuprofen group (p < 0.002) [30].
Topical forms of ibuprofen
The high demand for ibuprofen drugs is also due to the variety of its dosage forms. In patients with acute or chronic muscular-articular pain, especially with local damage to the musculoskeletal system and traumatic lesions of soft tissues, local use of NSAIDs in the form of gels and ointments is possible, which reduces the systemic effect and, consequently, adverse reactions.
The effectiveness of this dosage form is not inferior to the tablet form. A number of studies have shown that ibuprofen, regardless of the dosage form, is a highly effective NSAID with a good safety profile.
The widespread use of topical forms of ibuprofen is due to the fact that in patients taking oral forms of NSAIDs for a long time, erosive and ulcerative lesions of the gastrointestinal mucosa, including perforation and bleeding, can develop in 22–68% of cases. Moreover, up to 30% of additional costs in the treatment of arthritis can be attributed to the treatment of gastrointestinal side effects caused by taking oral NSAIDs [31, 32]. Given that topical NSAIDs are as effective as oral NSAIDs, their more favorable tolerability profile makes them preferable in certain clinical situations, such as knee pain. Thus, administration of oral and topical forms of ibuprofen has an equivalent effect on knee pain over the course of a year. Due to a more favorable tolerability profile, topical forms of NSAIDs can be prescribed as an alternative to oral forms [33]. Based on the results of a Cochrane review of 47 studies, the authors concluded that when using topical forms of NSAIDs, there is a good effect compared to enteral use and a significantly lower number of complications [34].
The same effectiveness of using a topical form of ibuprofen (5% gel) and oral ibuprofen 400 mg (1200 mg per day) has also been proven for acute soft tissue injury for at least 7 days. In both groups, complete improvement was observed between days 3 and 6 of therapy. It should be noted that the treatment was well tolerated in both groups (the identified cases of adverse events were not related to the treatment) [35].
While topical ibuprofen costs slightly more than oral ibuprofen, overall treatment costs are reduced by reducing the incidence of side effects, as shown in the TOIB study (Topical or oral ibuprofen for chronic knee pain in older people) [36]. .
Safety profile of ibuprofen therapy
The main concern for patients with chronic pain is the safety of the drug used over long-term use. It's no secret that the main serious side effect of all NSAIDs is gastrointestinal bleeding (GI bleeding). Many studies indicate that low dose ibuprofen use (up to 1200 mg/day) causes only minimal damage to the gastrointestinal mucosa, even with long-term use. Ibuprofen, as a drug with well-studied pharmacological effects, is considered the “gold standard” for safety of use, which is especially important in the treatment of patients with chronic pain syndromes. Ibuprofen in low doses (800–1200 mg per day) is approved for over-the-counter use in many countries and has a good safety profile comparable to paracetamol.
Increasing the recommended doses (up to 1800–2400 mg per day) is used in the long-term treatment of rheumatic and some other diseases of the musculoskeletal system. Based on a meta-analysis of observational epidemiological studies from 2000–2008. The influence of various NSAIDs on the risk of bleeding from the upper gastrointestinal tract has been established. As initially expected, the lowest incidence of GI bleeding was observed in the coxibs group (hazard ratio (RR) 1.88; 95% confidence interval (CI) 0.96–3.71), among non-selective NSAIDs, the best results were obtained with ibuprofen ( RR 2.69; 95% CI 2.17–3.33), the greatest risk was observed with ketorolac (RR 14.54; 95% CI 5.87–36.04) and piroxicam (RR 9.94; 95% CI 5.99–16.50). The authors concluded that the frequency of bleeding depends on several factors: the selectivity of the drug with respect to COX, the dosage and duration of use, as well as the half-life or use of a prolonged form of the drug [37]. Similar results were demonstrated in a number of earlier meta-analyses, according to which ibuprofen was characterized by the lowest risk of GI bleeding compared with diclofenac, naproxen, indomethacin, piroxicam and ketoprofen [37–40].
The dose-dependent effect of ibuprofen on the occurrence of serious gastrointestinal complications has been confirmed in a number of other studies. The risk of serious gastrointestinal adverse events with NSAIDs is relatively low, occurring in 1% of patients per year, primarily when used in high doses for long-term treatment of chronic conditions. The incidence of side effects when using ibuprofen in recommended doses in children and adults is comparable to that of paracetamol. Of all NSAIDs, ibuprofen appears to have one of the best gastrointestinal safety profiles [41, 42].
We can clearly conclude that ibuprofen has the best safety profile in relation to the gastrointestinal tract among non-selective NSAIDs, as well as a relatively low risk of developing cardiovascular complications with long-term use.
In accordance with existing recommendations, no advantages in the effectiveness of various NSAIDs, including selective ones, have been reliably identified in the treatment of rheumatic diseases, therefore the choice of drug should be made based on its safety profile and the individual characteristics of the patient. Coxibs are contraindicated in patients at high risk of cardiovascular complications. To reduce the risk of gastrointestinal complications, it is recommended to use misoprostol or proton pump blockers in conjunction with non-selective NSAIDs.
Currently, the first large randomized trial (n = 20,000 patients) is being conducted to establish the safety profile of celecoxib, ibuprofen and naproxen in patients suffering from OA or RA at high risk of developing cardiovascular complications [43]. This study will provide clearer recommendations regarding administration in these patients.
Conclusion
Thus, clinical experience with the use of ibuprofen for the most common forms of pain syndromes demonstrates its effectiveness not only as a means for relieving painful episodes, but also for the course treatment of chronic pain. An additional advantage of this drug is its existence in several dosage forms.
The use of ibuprofen (Nurofen) meets modern standards of pain therapy. Ease of use, variety of dosage forms of the drug and its availability determine high patient compliance with the prescribed therapy, which is the key to successful treatment.
More than 50 years of successful use of ibuprofen in widespread clinical practice in more than 80 countries as an over-the-counter drug serves as a clear example of its high profile of effectiveness and safety [44].
Literature
- Pharmaceutical market of Russia. May 2012 DSM Group. Available at: https://www.dsm.ru/content/file/cpravka_may_2012.pdf.
- Global Healthcare Calls for Target Marketing. Available on: https://blog.nielsen.com/nielsenwire/consumer/global-healthcare-calls-for-target-marketing/.
- Friessem CH, Willweber-Strumpf A., Zenz MW Chronic pain in primary care. German figures from 1991 and 2006 // BMC Public Health. 2009; 9:299.
- Breivik H., Collett B., Ventafridda V., Cohen R., Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment // Eur J Pain. 2006; 10: 287–333.
- Ayzenberg I., Katsarava Z., Sborowski A. et al. The prevalence of primary headache disorders in Russia: a countrywide survey // Cephalalgia. 2012; 32 (5): 373–381.
- Tabeeva G.R. Ibuprofen in the treatment of neurogenic pain syndromes // Consilium Medicum. 2006; 8 (2): 28–32.
- Blyth FM, March LM, Brnabic AJ, Jorm LR, Williamson M., Cousins MJ // Pain. 2001; 89 (2–3): 127–134.
- Patel AS, Farquharson R., Carroll D. The Impact and Burden of Chronic Pain in the Workplace: A Qualitative Systematic Review // Pain Pract. 2012.
- Chandler S., Payne R. Economics of unrelieved cancer pain // Am J HospPalliat Care. 1998; 15 (4): 223–226.
- National institute of health. The NIH Guide: new direction in pain research I. Washington (DC): US Government Printing Office; 1998.
- Gustavsson A., Bjorkman J., Ljungcrantz C. Socio-economic burden of patients with a diagnosis related to chronic pain - register data of 840,000 Swedish patients // Eur J Pain 2012; 16(2):289–299.
- Topchiy N.V., Toporkov A.S. Optimization of the use of non-steroidal anti-inflammatory drugs in general medical practice // RMJ. 2011; 19 (2): 27–32.
- Pharmaceutical market of Russia. May 2012 DSM Group. Available at: https://www.dsm.ru/content/file/cpravka_may_2012.pdf.
- Derry C., Derry S., Moore RA, McQuay HJ Single dose oral ibuprofen for acute postoperative pain in adults // Cochrane Database Syst Rev. 2009, Jul 8; (3): CD001548. Review. PubMed PMID: 19588326.
- Hersh EV, Kane WT, O'Neil MG, Kenna GA, Katz NP, Golubic S., Moore PA Prescribing recommendations for the treatment of acute pain in dentistry // Compend Contin Educ Dent. 2011, Apr; 32 (3): 22, 24–30; quiz 31–2. PubMed PMID: 21560740.
- Ahmad N., Grad HA, Haas DA, Aronson KJ, Jokovic A., Locker D. The efficacy of nonopioid analgesics for postoperative dental pain: a meta-analysis // Anesth Prog. 1997, Fall; 44 (4): 119–26. PubMed PMID: 9481955; PubMed Central PMCID: PMC2148941.
- Aids for management of common headache disorders in primary care 2007 www.who.int/entity/mental_health/neurology/who_ehf_aids_headache.pdf.
- Evers S., Afra J., Frese A., Goadsby PJ, Linde M., May A., Sandor PS European Federation of Neurological Societies. EFNS guideline on the drug treatment of migraine — revised report of an EFNS task force // Eur J Neurol. 2009, Sep; 16(9):968–981. PubMed PMID: 19708964.
- Rabbie R., Derry S., Moore RA, McQuay HJ Ibuprofen with or without an antiemetic for acute migraine headaches in adults // Cochrane Database Syst Rev. 2010, Oct 6; (10): CD008039. Review. PubMed PMID: 20927770.
- Verhagen AP et al. Treatment of tension type headache: paracetamol and NSAIDs work: a systematic review // Ned Tijdschr Geneeskd. 2010; 154:A1924. Review. Dutch. PubMed PMID: 20699021.
- Suthisisang C., Poolsup N., Kittikulsuth W., Pudchakan P., Wiwatpanich P. Efficacy of low-dose ibuprofen in acute migraine treatment: systematic review and meta-analysis // Ann Pharmacother. 2007, Nov; 41 (11): 1782–91. Epub 2007 Sep 18. Review. PubMed PMID: 17878396.
- Silver S., Gano D., Gerretsen P. Acute treatment of pediatric migraine: a meta-analysis of efficacy // J Paediatr Child Health. 2008, Jan; 44 (1–2): 3–9. Epub 2007, Sep 14. Review. PubMed PMID: 17854415.
- Damen L. et al. Symptomatic treatment of migraine in children: a systematic review of medication trials // Pediatrics. 2005, Aug; 116(2):e295–302. Review. PubMed PMID: 16061583.
- Boureau F., Pelen F., Verriere F. et al. Evaluation of lbuprofenvsParacetamol analgesic activity using a sore throat pain model // Clin Drug Invest. 1999; 17 (1): 1–8.
- Boureau F., Schneid H., Zeghari N., Wall R., Bourgeois P. The IPSO study: ibuprofen, paracetamol study in osteoarthritis. A randomized comparative clinical study comparing the efficacy and safety of ibuprofen and paracetamol analgesic treatment of osteoarthritis of the knee or hip // Ann Rheum Dis. 2004 Sep; 63 (9): 1028–34. PubMed PMID: 15308513; PubMed Central PMCID: PMC1755112.
- Towheed TE, Maxwell L, Judd MG, Catton M, Hochberg MC, Wells G. Acetaminophen for osteoarthritis. Cochrane Database Syst Rev. 2006, Jan 25; (1): CD004257. Review. PubMed PMID: 16437479.
- Rheumatology. Clinical recommendations / Ed. E. L. Nasonova. M.: GEOTAR-Media, 2008. 288 p.
- Zhang W. et al. EULAR evidence based recommendations for the management of hand osteoarthritis: report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT) // Ann Rheum Dis. 2007, Mar; 66(3):377–388. Epub 2006 Oct 17. PubMed PMID: 17046965; PubMed Central PMCID: PMC1856004
- Watanabe K., Watanabe H., Maeda Hagiwara M. et at. Influence of a muscle relaxant, tizanidine, on gastric acid secretion and ulcers in the rat // Folia Pharmacol Jpn. 1983; 82:237–245.
- Berry H., Hutchinson DR Tizanidine and ibuprofen in acute low-back pain: results of a double-blind multicentre study in general practice // J Int Med Res. 1988; 16 (2): 83–91.
- Aabakken L. NSAID-associated gastrointestinal damage: methodological considerations and a review of the experience with enteric coated naproxen // Eur J Rheumatol Inflamm. 1992; 12 (2): 9–20.
- Russell RI Non-steroidal anti-inflammatory drugs and gastrointestinal damage-problems and solutions // Postgrad Med J. 2001; 77 (904): 82–88.
- Underwood M., Ashby D., Cross P. et al. Advice to use topical or oral ibuprofen for chronic knee pain in older people: randomized controlled trial and patient preference study // BMJ. 2008; 336 (7636): 138–142.
- Tiso RL, Tong-Ngork S., Fredlund KL Oral versus topical Ibuprofen for chronic knee pain: a prospective randomized pilot study // PainPhysician. 2010; 13 (5): 457–467.
- Whitefield M., O'Kane CJ, Anderson S. Comparative efficacy of a proprietary topical ibuprofen gel and oral ibuprofen in acute soft tissue injuries: a randomized, double-blind study // J Clin Pharm Ther. 2002; 27 (6): 409–417.
- Castelnuovo E. et al. TOIB study team. Cost-effectiveness of advising the use of topical or oral ibuprofen for knee pain; the TOIB study Rheumatology (Oxford) 2008; 47(7):1077–1081.
- Masso Gonzalez EL et al. Variability among nonsteroidal antiinflammatory drugs in risk of upper gastrointestinal bleeding // Arthritis Rheum. 2010 Jun; 62(6):1592–1601. PubMed PMID: 20178131.
- Lewis SC et al. Dose-response relationships between individual nonaspirin nonsteroidal anti-inflammatory drugs (NANSAIDs) and serious upper gastrointestinal bleeding: a meta-analysis based on individual patient data // Br J Clin Pharmacol. 2002, Sep; 54(3):320–326. PubMed PMID: 12236853; PubMed Central PMCID: PMC1874428.
- Henry D. et al. Variability in risk of gastrointestinal complications with individual non-steroidal anti-inflammatory drugs: results of a collaborative meta-analysis // BMJ. 1996, Jun 22; 312(7046):1563–1566. PubMed PMID: 8664664; PubMed Central PMCID: PMC2351326.
- Richie F. et al. Time dependent risk of gastrointestinal complications induced by non-steroidal anti-inflammatory drug use: a consensus statement using a meta-analytic approach // Ann Rheum Dis. 2004, July; 63(7):759–766. Review. PubMed PMID: 15194568; PubMed Central PMCID: PMC1755051.
- Doyle G., Furey S., Berlin R. Gastrointestinal safety and tolerance of ibuprofen at maximum over-the-counter dose // Aliment Pharmacol Ther. 1999; 13(7):897–906.
- Bjarnason I. Ibuprofen and gastrointestinal safety: a dose-duration-dependent phenomenon // JR Soc Med. 2007; 100 Suppl 48:11–14.
- Becker MC et al. PRECISION Investigators. Rationale, design, and governance of Prospective Randomized Evaluation of Celecoxib Integrated Safety versus Ibuprofen Or Naproxen (PRECISION), a cardiovascular end point trial of nonsteroidal antiinflammatory agents in patients with arthritis // Am Heart J. 2009, Apr; 157(4):606–612. Epub 2009, Feb 25. PubMed PMID: 19332185.
- Rainsford KD Fifty years since the discovery of ibuprofen // Inflammopharmacology. 2011, Dec; 19(6):293–297. PubMed PMID: 22120888.
T. E. Morozova, Doctor of Medical Sciences, Professor S. M. Rykova, Candidate of Medical Sciences
GBOU VPO First Moscow State Medical University named after. I. M. Sechenova Ministry of Health of the Russian Federation, Moscow
Contact information for authors for correspondence
How to take Ibuprofen
Pills
Adults and children over 14 years of age can be given no more than 4 tablets per day. Depending on the condition, the dose can be adjusted and increased to 6 tablets (the dose is divided into several doses). When improvement is noted, the dose should be reduced to the original. The first tablet should be taken in the morning before meals with a glass of water. Then take 1 tablet after meals.
Without consulting a doctor, tablets can be used for no more than 5 days.
Candles
The suppositories are placed rectally. For pain and fever, the dose is determined taking into account the age and body weight of the baby. You can use no more than 10 mg per 1 kg at a time. Candles can be lit up to 4 times per day. The optimal duration of use is 3 days. If suppositories are used as an analgesic, they can be administered for 5 days.
If after the allotted time the fever has not disappeared, then you should consult your pediatrician.
Gel
You can use a 5-9 cm strip of gel at a time. Using smooth, light movements, rub the gel into the problem area until the composition is completely absorbed. It is allowed to use the gel no more than 4 times per day, with repeated use no earlier than after 4 hours.
The duration of the treatment course can be 15-20 days.
Ointment
The scheme for using the ointment is in all respects similar to applying the gel. The drug is rubbed into the problem area of the skin 3-4 times a day. Can be used within 15-20 days.
Children's suspension
Ibuprofen in the form of a suspension can be given to a child no more than 3 times a day. If your child is under one year old, you should definitely consult a specialist before use. If the fever appears as a result of vaccination, then the suspension is given 2 times a day. There should be a break of at least 6 hours between doses.
Detailed description of the study
There are a large number of different joint diseases. Among them are often found: rheumatoid arthritis, gout, post-infectious joint damage. Inflammation in the joints is manifested by swelling, tenderness, redness and a local increase in temperature in the affected area. Patients often experience pain and impaired joint mobility. In the future, their deformation, destruction of cartilage tissue, and narrowing of the joint space may occur. Some diseases, such as rheumatoid arthritis, also have systemic manifestations: a person notices pathological weakness, fatigue, weight loss, and fever.
It can be difficult to make a differential diagnosis of joint diseases due to similar symptoms. Laboratory tests help establish the correct diagnosis.
This study contains two tests necessary to identify the cause of joint inflammation:
- C-reactive protein;
- Uric acid.
C-reactive protein (CRP) is one of many molecules involved in immune responses. CRP is detected in the blood of patients during various inflammatory processes and is considered a marker of the acute phase of their course. An increase in CRP levels is observed within the first four hours after tissue damage and reaches a peak after 24–72 hours.
The content of CRP during inflammation can be increased by 20 times or more. The most common joint diseases that are accompanied by increased CRP are:
- Rheumatoid arthritis;
- Gout;
- Reactive arthritis.
CRP is also a marker of disease activity.
It should be noted that determining the level of CRP plays an important role in assessing joint inflammation, but is not a specific marker for this group of diseases. The indicator may reflect inflammation of another localization, including against the background of acute infections, injuries, and others.
Uric acid is one of the main products of protein metabolism in the human body. This substance is mainly excreted in the urine. When there is an excessive level of uric acid in the blood (hyperuricemia), deposition of its salts (urates) is observed with the formation of crystals. The latter are deposited in joints, subcutaneous tissue, and kidneys (where urates can form stones).
Gout is a systemic pathology, which is characterized by the accumulation of monosodium urate crystals in the joints, as well as other organs and tissues. An increase in uric acid levels suggests that joint inflammation is associated with the development of this disease.
Thus, this comprehensive study will help the doctor in differential diagnosis of the causes of joint damage and selection of therapy.
It is necessary to donate venous blood for analysis. Often the complex is prescribed in conjunction with other studies, such as general analysis and blood biochemistry, to check other organs and systems.
A detailed description of the studies and reference values are presented on the pages with descriptions of individual studies.
Contraindications and adverse reactions
Contraindications for all forms of medications include:
- stomach ulcers;
- problems with liver function;
- bearing a child (3rd trimester);
- internal bleeding;
- progressive kidney disease;
- chronic intestinal diseases;
- hypersensitivity to the constituent components.
It should be taken with caution for the following conditions and problems: liver cirrhosis, gastritis, stomach ulcers, problems with the cardiovascular system, liver and kidneys.
Children under 12 months can be given medicine only as prescribed by a doctor and under his supervision.
When using suppositories and tablets, the following adverse reactions may occur;
- irritation and dryness in the mouth;
- dyspnea;
- blurred vision;
- headache;
- confused thinking;
- disturbed sleep;
- high blood pressure;
- excessive sweating.
Chondroprotectors and intra-articular fluid substitutes
Artra, Dona, Structum, Teraflex, Chondroitin, Glucosamine, Adgelon, Piaskledin, Alflutop, Hyaluronic acid, Sinvisc, Ostenil, Noltrex, Sinocrom, Fermathron
Chondroprotectors are medications that heal joints. We use them if the nutrition of the joint is impaired (arthrosis, osteochondrosis, metabolic disorders), or the joint has been damaged by inflammation or injury. We begin full treatment with chondroprotectors after the inflammation has subsided.
Treatment with chondroprotectors for oral administration should be long-term : the effect usually begins after 3 months, and a stable effect - after at least 6 months. These medications are specifically designed for long-term use and are usually well tolerated.
Chondroprotectors for injection into a joint or intramuscularly have a faster effect, sometimes noticeable after 1 injection. In total, we perform from 1 to 5 intra-articular or 10-20 intramuscular injections per course, followed by a transition to taking drugs orally.
Injections create a high concentration of medication directly into the affected joint
Chondroprotectors help work and medications that improve blood circulation and metabolism .
Chondroprotectors for oral administration. Commonly used medications.
Piascledine is a herbal preparation that regulates metabolism in cartilage tissue. Contains unsaponifiable compounds from avocado and soybean oils. The drug helps slow down the development of the degenerative process in cartilage tissue, relieves pain (associated with this process) and restores the patient’s motor function. Stimulates the synthesis of proteoglycans and collagen. Promotes the restoration of cartilage tissue. Reduces collagenase production.
Chondroitin and/or Glucosamine are contained in the preparations Artra, Dona, Structum, Teraflex.
Chondroitin , a drug that affects phosphorus-calcium metabolism in cartilage tissue , is a high molecular weight mucopolysaccharide. Slows down the destruction of bone tissue and reduces calcium loss, accelerates the process of bone tissue restoration, and inhibits the process of degeneration of cartilage tissue. Prevents compression of connective tissue and plays the role of a kind of lubricant of articular surfaces. When used externally, it slows down the progression of osteoarthritis. Normalizes metabolism in hyaline tissue. Stimulates the regeneration of articular cartilage.
Glucosamine is a drug that affects metabolism in cartilage tissue. Replenishes the natural deficiency of glucosamine, stimulates the synthesis of proteoglycans and hyaluronic acid in synovial fluid; increases the permeability of the joint capsule, restores enzymatic processes in the cells of the synovial membrane and articular cartilage. Promotes fixation of sulfur during the synthesis of chondroitinsulfuric acid, facilitates normal calcium deposition in bone tissue, inhibits the development of degenerative processes in joints, restores their function and reduces pain. With a single oral administration of an average therapeutic dose, the maximum concentration in plasma is achieved after 3-4 hours, in the synovial fluid - after 4-5 hours.
Injectable drugs and intra-articular fluid substitutes. Frequently used drugs.
Adgelon is a drug that stimulates the process of regeneration of cartilage tissue. The active substance of the drug is a glycoprotein isolated from cattle blood serum. The drug promotes the rapid accumulation of mass of young cartilage cells and their differentiation, which leads to more rapid formation of replacement cartilage tissue, restoration of a smooth articular surface in the area of damage and improved joint mobility. When using the drug, the damaged area is filled with young cartilage cells. With intra-articular injections , the basic substance produced by the cells of cartilage tissue has a more ordered structure: it becomes as dense as in normally functioning cartilage tissue.
Alflutop is an injection drug of natural origin. This is a bioactive concentrate from small sea fish Sprat (Sprattus sprattussprattus), Black Sea whiting (Odontogadus merlangus euxinus), Black Sea bellyfish (Alosa tanaica nordmanni), Black Sea anchovy (Engraulis encrassicholusponticus). The drug Alflutop regulates metabolism in cartilage tissue, consists of mucopolysaccharides, chondroitin sulfate, amino acids, peptides, sodium ions, potassium, calcium, magnesium, iron, copper and zinc. Alflutop prevents the destruction of macromolecular structures of normal tissues, stimulates restoration processes in interstitial tissue and articular cartilage tissue, which explains its analgesic effect. The anti-inflammatory effect of Alflutop and tissue regeneration are based on inhibition of hyaluronidase activity and normalization of hyaluronic acid biosynthesis. These effects are synergistic and cause activation of tissue restoration processes (in particular, restoration of metabolic processes in cartilage tissue).
100% synthetic polymer Noltrex does not contain substances of animal origin and is not a natural metabolite. Due to the presence of silver ions in the composition of the drug, Noltrex has antibacterial properties. When Noltrex is administered at the first stage, physical separation of the contacting and rubbing surfaces of the joint affected by osteoarthritis occurs as a result of an increase in the viscosity of the synovial fluid. Pain is reduced and joint mobility is improved. At the second stage, due to the unique properties of Noltrex, like a sponge, it absorbs joint fluid and water from the cartilage and subchondral bone, providing decompression of pain endings. At the third stage, biochemical fragments of the joint fluid - enzymes of inflammation and proteolysis - are adsorbed and inactivated on strictly oriented active centers of the polymer. At the same time, silver ions migrate to the surface of the joint, resulting in the suppression of endogenous infection. Noltrex is one of the most easily used means of combating arthrosis today. The entire process of using the drug comes down to a common and very widespread procedure - intra-articular injection, which does not require any additional skills from the doctor.
Substitutes for intra-articular fluid are hyaluronic acid preparations (Synvisc, Ostenil, Sinokrom, Fermatron). The therapeutic effect of Hyaluronic acid is associated with “replenishing the viscosity” of the intra-articular fluid of the affected joint. In addition, the action of sodium hyaluronate is based on the “trigger” effect - it directly restores the ability of the joint to produce hyaluronan and, thus, returns it to a state of biochemical equilibrium, which persists for several months. As accumulated clinical materials show, the following points occur when using sodium hyaluronate:
- restores synovial balance: increases the viscosity of synovial fluid, restoring its lubricating, shock-absorbing and filtering properties;
- protects articular cartilage from mechanical and chemical damage: restores the protective coating on the inner surface of the joint and increases the binding of free radicals;
- inflammation of the synovial membrane decreases and its protective functions are restored.
Slowing down the destruction of articular cartilage in combination with the processes of restoring the biochemical balance of the synovial fluid leads to rapid relief of pain symptoms and regression of the phenomena of limited mobility in the joint.
The beneficial effect of sodium hyaluronate appears gradually during the course and lasts for several months. After completing a full course of 5 injections, symptoms are usually relieved for a period of 6 to 12 months.