Anyone who experiences constant pain in the back and joints knows how pain hinders movement and normal human activities are limited.
The pain is repeated day after day, the use of all kinds of ointments and tablets brings relief for a while or does not give at all.
It's time to go to a medical facility, undergo an examination, establish an accurate diagnosis and begin the correct treatment.
If you have been diagnosed with vertebrogenic pain syndrome, know that pain occurs not only due to problems in the back, it is a problem of the whole body. This is not a separate disease, but a consequence of disorders in the spine, surrounding tissues and ligaments. It is necessary to identify the cause of the disease and then begin treatment.
Classification and causes
Vertebrogenic pain syndrome is not common; it affects about 10% of patients with disorders of the spinal trunk.
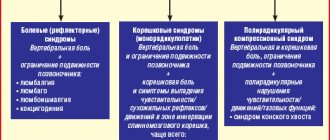
Types of classification of vertebrogenic pain:
- Non-mechanical pain. These pains are associated with immobility, the joints seem to be stiff and move poorly. Pain can also occur at rest. These are algic and dysgemic types.
- Pain of a mechanical nature occurs when a nerve root is compressed, muscle spasm, this is a compression type.
- The defixation type of pain is caused by an unstable joint in the segment responsible for movement. The pain may increase with bending and movement.
Risk factors for the occurrence of vertebrogenic pain syndrome include:
- osteochondrosis in the development stage;
- the patient is overweight;
- presence of metabolic diseases;
- being in stressful situations and overexertion;
- abuse of physical activity, alcohol, smoking;
- heredity.
Men and women aged 30-50 years, whose work involves stress on the spine, are at risk.
The reasons can be divided into three groups:
- If there are congenital pathologies: bends of the vertebral trunk, tortuosity.
- Acquired diseases that reduce the lumen in blood vessels: atherosclerosis, thrombosis.
- If external pressure is applied to the blood artery: stage III-IV osteochondrosis, curvature of the spine, muscle spasms, spinal injuries, neoplasms in the spinal column.
Many experts attribute predisposing factors to the causes of the development of pain syndrome: diseases of the throat and nose organs of the chronic stage, bronchi and lungs, injuries to the skull and brain, poor blood clotting if blood circulation is impaired.
And yet, the first place in the causes of pain is occupied by diseases and inflammation of the spine.
Vertebral artery syndrome
One of the most important features of the structure of the cervical spine is the presence of holes in the transverse processes of the VI-II cervical vertebrae. These openings form a canal through which the main branch of the subclavian artery passes - the vertebral artery with the sympathetic nerve of the same name (Frank's nerve).
Irritation of the efferent sympathetic fibers of the plexus causes vascular spasm - a compression-irritative version of the syndrome is formed. If a spasm occurs in response to irritation of receptors in the area of the affected SMS, i.e., by a reflex, it speaks of reflex angiospastic cerebral syndrome.
With the compression-irritative variant, a narrowing of the vessel is possible not only as a result of its spasm, but also as a result of a mechanical effect on its wall - compression of the artery. With the appearance of organic disturbances in brain function, they speak of the organic stage of the syndrome, and in their absence - of the functional stage.
The functional stage of vertebral artery syndrome is characterized by three groups of symptoms: headache (and accompanying autonomic disorders), cochleovestibular disorders, visual disorders. Headache, pulsating or cerebral, aching, burning, constant and intensifying in paroxysms, especially when moving the head, with its prolonged forced position, spreading from the back of the head forward to the forehead.
The patient, showing this zone on himself, makes a movement with his palm, as if removing a gas mask - a symptom of removing a helmet. The pain is reproduced or intensified with pressure and especially with tapping at the point of the vertebral artery. On the sore side, other vascular points are also painful - the external carotid artery, especially the temporal branch, the orbital branches along the inner-superior corner of the orbit. The scalp is often painful even with a light touch or combing the hair.
Cochleovestibular disorders also in the form of paroxysmal non-systemic dizziness (feeling of instability, swaying) or systemic dizziness. They can be combined with paracusia (tinnitus), mild hearing loss and give rise to confusion with Meniere's disease.
Visual disturbances are limited to disturbances: darkening in the eyes, a feeling of sand, sparks and other photopsies, slight changes in the tone of the fundus vessels.
In conditions of prolonged and intense vascular spasms, the development of foci of persistent ischemia is possible - the organic stage of vertebral artery syndrome.
The organic stage of the vertebral artery is manifested by transient and persistent circulatory disorders in the brain and spinal cord. Transient circulatory disorders in the vertebrobasilar system are possible, as with this kind of non-vertebrogenic disorders: short-term ataxic disorders, nausea, articulation disorders and other loss of function from the IX-X or other cranial nerves. There are, however, forms of transient cerebral ischemia, most often observed with vertebrogenic lesions of the vertebral arteries. They often occur when turning or tilting the head. These are, firstly, attacks of sudden falling while maintaining consciousness and attacks of fainting. The first last for one to two minutes, the second last longer. The return of consciousness occurs faster in a horizontal position. After the attack, in addition to general weakness, headaches are observed; tinnitus, photopsia, severe autonomic lability. The attacks are caused by paroxysmal ischemia of the brain stem, its reticular formation (during syncope attacks) and in the area of the intersection of the pyramids (during attacks of falling).
In case of persistent circulatory disorders in the vertebrobasilar system, the symptoms of brain stem and cerebellar pathologies remain persistently, at least for longer than a day.
Although the clinical manifestations of both forms of vertebral artery syndrome are similar, reflex angiospastic syndrome still has its own distinctive features. It is characterized by:
- Bilaterality and diffuseness of cerebral vegetative-vascular disorders;
- The predominance of vegetative manifestations over focal ones;
- Relatively less connection between seizures and head rotation;
- Compression-irritative syndrome is more common in pathologies of the lower cervical spine and is combined with brachial pectoral syndromes; reflex syndrome occurs when the upper and middle cervical levels are affected.
Difficult to treat. Prone to chronic process.
Mechanism of occurrence and development options
Our spine consists of vertebrae, intervertebral discs, joints and ligaments. It is surrounded by blood vessels, muscles and nerve endings.
With osteochondrosis, when the discs wear out and destroy, the vertebrae shift away from the main trunk, protrusions and hernias form, blood vessels and nerve roots are compressed.
This is how vertebrogenic pain syndrome arises, characterized by acute pain at the site of injury.
There are two variants of the development of the syndrome:
- Compression of the nerve trunk. It occurs when the cervical and thoracic regions are affected; pain in this case is of low or medium intensity and can spread to the upper limbs or encircle the torso. When the cervical spine is affected, the upper limbs become numb and may even become atrophied.
- Compression of the nerve roots. These pains are observed with pathologies in the lumbar and sacral regions; they are more intense and cutting. Localization of these pains occurs in the lower extremities and perineum. Venous and arterial blood flow worsens.
Vertebrogenic syndrome occurs most often in the last stages of osteochondrosis, when an intervertebral hernia forms.
The most common causes of compression (squeezing) of the vertebral arteries
1. Manifestations of degenerative-dystrophic lesions (osteochondrosis) of the cervical spine: bone growths (osteophytes), arthrosis of uncovertebral joints, medial herniated intervertebral discs.
2. The presence of an atypical variant of the origin of the vertebral artery from the subclavian artery.
3. The presence of anomalies (structural features) of the cranio-vertebral junction (Kimmerly's anomaly, accessory cervical rib).
4. Severe spasm of the neck muscles (including the inferior oblique muscle of the head, covering the vertebral artery in the suboccipital area).
Symptoms of vertebrogenic syndrome
The main sign that changes are occurring in the spine is pain.
Symptoms of the development of vertebrogenic pain syndrome depend on the location where the destruction of the vertebrae and discs and pinching of the nerve roots occurred.
| Spine department | Symptoms of the syndrome |
| Cervical | Painful shooting sensations in the neck and back of the head. Neck muscle tension. Pain, numbness, tingling in the hands. Breathing is difficult, headache and dizziness. Pain increases when coughing, sneezing, or changing body position during sleep in the later stages of osteochondrosis. Sometimes the syndrome is accompanied by deterioration of vision and hearing. |
| Chest | The pain is concentrated in the back and lower back, in the area of the shoulder blades. During turns and bends of the body, the pain intensifies. Breathing is difficult, angina pectoris, and digestive system failure are noted. |
| Lumbar, sacral | Dull aching pain concentrated in the lower back and lower abdomen, numb toes, upset bowels, frequent urination |
An attack of vertebrogenic pain syndrome can last from 30 minutes and not subside for several hours. After using medicinal drugs, the pain subsides after 5-7 days.
Acute pain can last from one and a half to three months, after this period the chronic stage of the disease begins.
Treatment of osteochondrosis of the lumbar spine
If you experience acute lower back pain for the first time, you should definitely consult a doctor to establish a diagnosis in order to rule out an attack of renal colic, appendicitis, or any other disease that requires emergency medical care.
If the cause of back pain is known, and this is an exacerbation of osteochondrosis of the lumbar spine, first of all it is necessary to reduce the load on the spine as much as possible. You need to stay in bed for 3-7 days - sometimes this is the only way to significantly reduce pain. But to speed up recovery, proper, that is, effective, treatment is necessary. It should stimulate the human body’s own protective and healing processes. Treatment should take into account the localization of the lesion, the stage of the disease, the functional state of the body and its individual systems. Surgical treatment of this disease is indicated only in very severe cases. Most often, various methods of conservative treatment of osteochondrosis are used.
Conservative treatment of lumbar osteochondrosis
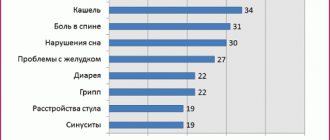
Conservative treatment methods are primarily drug treatment. In order to reduce pain, as well as to reduce inflammation, which is often the cause of vertebral syndrome, nonsteroidal anti-inflammatory drugs (NSAIDs) are prescribed in the form of tablets or, in acute cases, in the form of injections. Sometimes after an injection of an analgesic, the pain subsides and does not return even when the drug expires. This means that the vicious circle in which pain leads to muscle spasm, and muscle tension, in turn, increases pain, has been broken. However, if the pain continues for a long time, it is important to remember that NSAIDs usually have various side effects and, when taken for a long time, can cause unwanted complications - a decrease in the number of leukocytes in the blood, complications from the gastrointestinal tract.
Often, to improve the general condition of patients, sedatives (calming) drugs are prescribed for 1-3 weeks, as well as small doses of antidepressants. For osteochondrosis of the lumbar spine, novocaine blockades are performed if necessary. Recently, anticonvulsant drugs have been successfully used to relieve pain.
To reduce compression syndromes, manual therapy, traction treatment (spinal traction) and, in special cases, surgery are used.
When the fixation properties of the ligamentous-articular apparatus of the spine are weakened, it is recommended to use fixation devices - corsets, collars, bandages, etc. However, fixation devices can only be used for a limited time, since muscle weakening is observed when using them. And for patients with spinal osteochondrosis, it is extremely important to strengthen their own muscle corset in the future.
After relieving acute symptoms, the task of creating muscle fixation comes first, and then stimulating the processes of regeneration of damaged structures. For this purpose, therapeutic exercises, reflexology, and massage are used. For this purpose, chondroprotectors are used (drugs for restoring cartilage tissue). As well as drugs that improve the condition of blood vessels (angioprotectors), vitamins, primarily group B, calcium preparations that improve the condition of bone tissue.
Physiotherapeutic procedures are widely used to treat spinal osteochondrosis. They reduce pain and swelling of tissues, improve blood circulation, and stimulate muscle fixation. Procedures can be combined and alternated. Physiotherapeutic treatment methods that can be used include:
- darsonvalization of the affected area of the back and affected limbs;
- electrophoresis;
- low-energy laser radiation;
- ultrasound;
- exposure to a magnetic field;
- thermal procedures
In sanatorium conditions, mud, ozokerite, paraffin baths, radon, sulfide, hydrogen sulfide, turpentine and other baths are successfully used;
It must be remembered that the development of full regeneration requires a fairly long period of time; under favorable circumstances, it occurs in the sixth month. Therefore, treatment must be long-term. It should be carried out in combination, that is, combine medications with physiotherapy and exercise therapy.
Diagnosis of vertebrogenic syndrome.
To make a diagnosis and prescribe treatment, you must contact a neurologist.
The doctor will ask you in detail about the type and nature of pain, study your medical history, and ask about genetic abnormalities, lifestyle and work activity.
The doctor can determine the displacement of the vertebrae by feeling the spinal column.
Afterwards he will prescribe tests on the devices.
Criteria for diagnosis:
- pain in the cervical, thoracic, lumbar and sacral regions;
- if the pain intensifies with movement;
- if using a corset or lying down the pain decreases;
- if you have to provide support with your hands when standing up;
- if when walking the gait becomes swaying;
The studies that give the most effective results are considered to be computed tomography (CT), which studies the affected area in detail, and magnetic resonance imaging (MRI), which helps to detect the cause of blood flow disturbances.
If the case is not advanced, sometimes it is enough to take an x-ray.
Exercise therapy
Exercise therapy for vertebral artery syndrome is an effective method of eliminating the main pathological symptoms, the effectiveness of which is based on strengthening the muscular structures of the neck, which create a framework for the neurovascular bundle. With the help of special therapeutic exercises, it is possible to achieve a positive effect of therapy and prevent complications of the process. The doctor will tell the patient in more detail about the duration and scope of such treatment after studying the clinic’s problem, the extent of the disorders and the presence of complications.
Treatment and prevention of vertebrogenic pain syndrome
Experts advise treating pain syndrome in a comprehensive manner:
- Preventive methods . In the first few days it is better to stay in bed. Eliminate physical activity, sit less. Use orthopedic mattresses and pillows, wear special corsets and a collar.
- Medication methods. Use analgesics, non-steroidal and anti-inflammatory drugs: diclofenac, relanium, ketorol, ketoprofen, nimesulide, piroxicam. To block prolonged pain, nerve blockades are prescribed using lidocaine, novocaine, diprospan, hydrocortisone.
- Unconventional methods. These methods include the use of:
- manual therapy for realignment of vertebrae;
- osteopathy to correct and suppress the symptoms of pain and eliminate it;
- reflexology to relieve nerve tension;
- hirudotherapy, which relieves swelling;
- homeopathy to eliminate disturbances in the functioning of internal organs.
Physiotherapy, magnet and ultrasound therapy help prevent the development of exacerbation of pain syndrome.
If after using all treatment methods the pain does not go away, experts recommend surgery.
Remember that timely contact with specialists will help not only get rid of vertebrogenic pain syndrome, but also prevent its consequences, which may be irreversible.
Drug treatment
Drug treatment of vertebral artery syndrome with spinal osteochondrosis and other disorders of the cervical region includes a number of medications, the action of which is aimed at restoring lost functions, eliminating pathological symptoms and preventing the development of complications. For vertebral artery syndrome the following are prescribed:
- decongestants that help eliminate compression of blood vessels by neighboring tissues;
- muscle relaxants to relieve compression and tension of muscle tissue;
- drugs to improve brain nutrition;
- vascular dosage forms;
- neuroprotectors that protect nervous tissue from ischemia;
- drugs for the treatment of atherosclerosis;
- B vitamins to strengthen nerve fibers;
- antispasmodics that relieve headaches.
Medicines for vertebral artery syndrome can be taken only with the permission of the attending physician, without changing the dosages prescribed by the specialist and without exceeding the prescribed course. It is important to understand that any self-medication and ignoring the doctor’s recommendations has dangerous consequences, which often pose a threat to the patient’s life.