Joint pathologies require a comprehensive course of treatment using different methods - medication and physiotherapy, exercise therapy and special diets. All this allows you to relieve exacerbation and reduce the risk of relapse to the maximum. But sometimes joint pain is difficult or slow to relieve, and then intra-articular injections come to the rescue. Such procedures ensure the delivery of the drug directly to the inflammatory focus, resulting in rapid relief.
Injections for joints are prescribed for arthralgia - joint pain - of various origins and impaired mobility. They are used in the treatment of arthrosis and arthritis, gout, synovitis and bursitis. Thanks to the injection of drugs, damage to ligaments, tendons, knee menisci and cartilage is successfully treated.
Glucocorticosteroids (hormonal)
Hormones have a strong anti-inflammatory effect, due to which pain goes away and swelling subsides. Such drugs are prescribed in tablets and ointments, and are also injected intramuscularly. But intra-articular injections work much faster and better. An additional advantage of steroids is the low risk of systemic adverse reactions, since they enter the blood in a negligibly small volume. Painkilling injections for joint pain are given with medications such as:
- flosterone;
- diprospan;
- kenalog;
- hydrocortisone;
- celeston.
Hormones are administered either individually or in combination with vitamins and local anesthetics (Lidocaine).
Attention! Steroids are useless and even dangerous for septic – infectious – arthritis. It is treated with antibiotics, which are administered only after the joint has been washed.
Treatment of arthrosis of the knee joints - treatment of gonarthrosis
Treatment of arthrosis of the knee joints, treatment of gonarthrosis is, to put it mildly, not the easiest task. Therefore, before you begin your difficult fight against this disease, be sure to find a good doctor, get examined by him and draw up a treatment plan with him.
Never try to diagnose yourself!
The fact is that joint lesions resembling arthrosis occur in many other diseases, and uninformed people very often make mistakes in determining the diagnosis. It is better not to save time and money on a medical consultation, because a mistake can cost you much more in all respects.
But this does not mean that you are obliged to blindly trust any doctor and should not delve into the essence of his recommendations, comprehending the mechanism of action of the medications that are prescribed to you. The patient must understand the meaning of medical prescriptions and imagine why certain medical procedures are carried out.
Thus, during the therapeutic treatment of gonarthrosis, it is important to combine a number of therapeutic measures in such a way as to solve several problems at once:
- eliminate pain;
- improve nutrition of articular cartilage and accelerate its recovery;
- activate blood circulation in the area of the affected joint;
- reduce pressure on damaged joint areas of bones and increase the distance between them;
- strengthen the muscles surrounding the sore joint;
- increase joint mobility.
Below we will look at how this or that treatment method helps achieve your goals:
Video: Treatment of arthrosis of the knee joint, part 2:
Non-steroidal anti-inflammatory drugs:
Non-steroidal anti-inflammatory drugs - NSAIDs: diclofenac, piroxicam, ketoprofen, indomethacin, butadione, meloxicam, Celebrex, nimulide and their derivatives.
For arthrosis, non-steroidal, that is, non-hormonal, anti-inflammatory drugs are traditionally used to eliminate pain and inflammation of the joint, since against the background of severe pain it is impossible to begin normal treatment. Only by eliminating acute pain with anti-inflammatory drugs can you subsequently move on, for example, to massage, gymnastics and those physiotherapeutic procedures that would be intolerable due to pain.
However, it is undesirable to use drugs from this group for a long time, as they can “mask” the manifestations of the disease.
After all, when the pain decreases, a deceptive impression is created that healing has begun. Arthrosis, meanwhile, continues to progress: NSAIDs only eliminate individual symptoms of the disease, but do not cure it.
Moreover, in recent years, data have been obtained indicating the harmful effects of long-term use of non-steroidal anti-inflammatory drugs on the synthesis of proteoglycans. Proteoglycan molecules are responsible for the entry of water into cartilage, and disruption of their function leads to dehydration of cartilage tissue. As a result, cartilage already affected by arthrosis begins to deteriorate even faster. Thus, pills that a patient takes to relieve joint pain may accelerate the destruction of that joint.
In addition, when using non-steroidal anti-inflammatory drugs, it is necessary to remember that they all have serious contraindications and can cause significant side effects with long-term use.
Read more about anti-inflammatory drugs here*
***
Chondroprotectors - glucosamine and chondroitin sulfate:
Chondroprotectors - glucosamine and chondroitin sulfate - are substances that nourish cartilage tissue and restore the structure of damaged joint cartilage.
Chondroprotectors are the most useful group of drugs for the treatment of arthrosis.
Unlike non-steroidal anti-inflammatory drugs (NSAIDs), chondroprotectors do not so much eliminate the symptoms of arthrosis as act on the “base” of the disease: the use of glucosamine and chondroitin sulfate helps restore the cartilaginous surfaces of the hip joint, improve the production of joint fluid and normalize its “lubricating” properties.
Such a complex effect of chondroprotectors on the joint makes them indispensable in the treatment of the initial stage of arthrosis. However, there is no need to exaggerate the capabilities of these drugs.
Chondroprotectors are not very effective in the third stage of arthrosis, when the cartilage is almost completely destroyed. After all, it is impossible to grow new cartilage tissue or return the deformed bones of the knee to their previous shape with the help of glucosamine and chondroitin sulfate.
And even in the first and second stages of gonarthrosis, chondroprotectors act very slowly and do not immediately improve the patient’s condition. To get a real result, you need to undergo at least 2-3 courses of treatment with these drugs, which usually takes from six months to one and a half years.
Read more about chondroprotectors here*
***
Therapeutic ointments and creams:
Medicinal ointments and creams cannot in any way heal arthrosis of the knee joints (even if their advertising claims otherwise). But nevertheless, they can alleviate the patient’s condition and reduce pain in the sore knee. And in this sense, ointments are sometimes very useful.
Thus, for arthrosis of the knee joint that occurs without symptoms of synovitis, I recommend warming ointments to my patients in order to improve blood circulation in the joint.
For this purpose, Menovazin, Gevkamen, Espol, Nicoflex-cream, etc. are used. The listed ointments usually cause the patient a feeling of pleasant warmth and comfort. They rarely give any side effects.
Ointments based on non-steroidal anti-inflammatory substances (Indomethacin, Butadionic, Dolgit, Voltaren-gel, Fastum) are used in cases where the course of gonarthrosis is aggravated by symptoms of synovitis. Unfortunately, they do not act as effectively as we would like - after all, the skin allows no more than 5-7% of the active substance to pass through, and this is clearly not enough to develop a full anti-inflammatory effect.
***
Products for compresses:
Compress products have a slightly greater therapeutic effect compared to ointments.
Of the topical agents used in our time, in my opinion, three drugs deserve the greatest attention: dimexide, bischofite and medical bile.
Dimexide is a chemical substance, a liquid with colorless crystals, which has a good anti-inflammatory and analgesic effect. Moreover, unlike many other substances for external use, dimexide is actually able to penetrate skin barriers. That is, dimexide applied to the skin is actually absorbed by the body and works within it, reducing inflammation at the site of the disease. In addition, dimexide has a resolving property and improves metabolism in the area of application, which makes it most useful in the treatment of arthrosis that occurs with the presence of synovitis.
Bishofite is an oil derivative, a brine obtained during oil drilling. It gained its fame thanks to drillers who were the first to pay attention to its therapeutic effect on arthrosis. While working in oil wells, drillers experienced resorption of arthrosis nodules on their hands due to constant contact with oil brine. Later it turned out that Bishofite has a moderate anti-inflammatory and analgesic effect, and also has a warming effect, causing a feeling of pleasant warmth.
Medical bile is natural bile extracted from the gall bladders of cows or pigs. Bile has a resolving and warming effect and is used in the same cases as bischofite, but has some contraindications: it cannot be used for pustular skin diseases, inflammatory diseases of the lymph nodes and ducts, febrile conditions with increased body temperature.
***
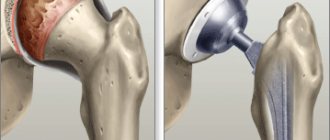
Intra-articular injections (injections into the joint):
Intra-articular injections are often used to provide emergency treatment for arthrosis of the knee joint. In many cases, intra-articular injection can actually alleviate the patient's condition. But at the same time, injections into the joint for arthrosis are done much more often than is actually necessary. It is about this incorrect, in my opinion, trend that I would like to talk in more detail.
Most often, corticosteroid hormone preparations are injected into the joint: Kenalog, Diprospan, hydrocortisone, flosterone, celeston .
Corticosteroids are good because they quickly and effectively suppress pain and inflammation due to synovitis (edema and swelling of the joint). It is the speed with which the therapeutic effect is achieved that is the reason why corticosteroid injections have gained particular popularity among doctors.
But this led to the fact that intra-articular injections of hormones began to be carried out even without a real need. For example, I have more than once encountered the fact that hormones were injected into a patient’s joint for prophylactic purposes in order to prevent the further development of arthrosis.
However, the problem is that it is arthrosis itself that corticosteroids do not and cannot treat. This means they cannot prevent the development of arthrosis! Corticosteroids do not improve the condition of articular cartilage, strengthen bone tissue, or restore normal blood circulation.
All they can do is reduce the body’s inflammatory response to this or that damage in the joint cavity. Therefore, it is pointless to use intra-articular injections of hormonal drugs as an independent method of treatment: they should be used only in the complex therapy of arthrosis.
For example, a patient has stage II gonarthrosis with swelling of the joint due to the accumulation of fluid in it. The accumulation of fluid (synovitis) makes it difficult to carry out medical procedures: manual therapy, gymnastics, physiotherapy. In such a situation, the doctor performs an intra-articular injection of a hormonal drug to eliminate synovitis, and a week later begins other active treatment measures - this is the right approach.
Now let's imagine a different situation. The patient also has stage II gonarthrosis, but without fluid accumulation and joint swelling. Is it necessary to inject corticosteroids into the joint in this case? Certainly not. No inflammation - no “point of impact” for corticosteroid hormones.
But even if intra-articular injection of corticosteroids is really necessary, a number of rules must be followed. Firstly, it is undesirable to do such injections into the same joint more often than once every 2 weeks. The fact is that the administered medicine will not “work” in full force immediately and the doctor will be able to finally assess the effect of the procedure just after 10 - 14 days.
You should also know that usually the first injection of corticosteroids brings more relief than subsequent ones. And if the first intra-articular injection of a drug does not produce results, it is unlikely that the second or third injection of the same drug in the same place will. If the first intra-articular injection is ineffective, you need to either change the drug, or, if changing the drug does not help, choose the injection site more accurately.
If after this the injection of a corticosteroid into the joint does not give the desired result, it is better to abandon the very idea of treating this joint with hormonal drugs. Moreover, it is generally extremely undesirable to inject hormones into the same joint more than four or five times, otherwise the likelihood of side effects increases significantly.
Unfortunately, in practice we have to deal with excessive “singleness” of doctors who inject corticosteroids into the same joint over and over again, without achieving at least a minimal effect with the first three injections. Two similar cases struck me more than others.
One of the patients received “only” ten injections of Kenalog, and the procedure was carried out daily, even without the required ten-day break necessary to evaluate the results of the injection. And the second patient was injected with hormones inside the knee joints, observing an interval (though only 3 to 5 days), but during the course of treatment the poor fellow received twenty to twenty-five injections of corticosteroids into one joint!
It would seem that the doctor “went too far” a little - no big deal. Could there be any harm from such treatment? It turns out it can!
Firstly, with each injection, the joint, albeit slightly, is injured by the needle. Secondly, with intra-articular injection there is always some risk of infection in the joint. Thirdly, frequent injections of hormones provoke disruption of the structure of the joint ligaments and surrounding muscles, causing relative “looseness” of the joint.
And most importantly, frequent injections of corticosteroids worsen the condition of those patients whose joint damage is combined with diabetes mellitus, high blood pressure, obesity, renal failure, gastric or intestinal ulcers, tuberculosis, purulent infections and mental illness. Even when administered exclusively into the joint cavity, corticosteroids have an effect on the entire body and can aggravate the course of these diseases.
hyaluronic acid preparations into the knee joint affected by arthrosis (another name for hyaluronic acid is sodium hyaluronate). They went on sale about 15 years ago.
Hyaluronic acid (sodium hyaluronate) preparations are also called “liquid prostheses” or “liquid implants” because they act on the joint like healthy synovial fluid - that is, as a natural “joint lubricant”.
Hyaluronic acid preparations are very useful and effective medicines: sodium hyaluronate forms a protective film on damaged cartilage, protecting cartilage tissue from further destruction and improving the sliding of contacting cartilage surfaces.
In addition, hyaluronic acid preparations penetrate deep into the cartilage, improving its firmness and elasticity. Thanks to hyaluronidase, cartilage that has dried out and become thinner due to arthrosis restores its shock-absorbing properties. As a result of weakening the mechanical overload, pain in the sore knee joint decreases and its mobility increases.
At the same time, when administered correctly into the joint cavity, hyaluronic acid preparations have virtually no side effects.
Treatment with hyaluronic acid preparations is carried out in courses: in total, a course of treatment requires 3-4 injections into each sore knee, the interval between injections is usually from 7 to 14 days. If necessary, the course is repeated after six months or a year.
From my point of view, the main and only serious drawback of hyaluronic acid preparations is their high price. Thus, in 2021, hyaluronic acid is represented on our market mainly by imported drugs Synvisc , Fermatron , Ostenil , Duralan , etc.
On average, each injection with these drugs costs the patient no less than 3,000 - 5,000 rubles.
But returning to the issue of savings, I would like to note that despite the relatively high cost of hyaluronic acid preparations, their use made it possible to literally “put back on their feet” many patients who previously, before the advent of these drugs, would have definitely had to undergo surgery.
And taking into account the cost of joint surgery, it turns out that timely use of hyaluronic acid (even over several years) in any case and in every sense costs the patient much less than knee replacement surgery. Of course, provided that the doctor performing such injections knows the injection technique.
Note from Dr. Evdokimenko. This is important to know: hyaluronic acid preparations are instantly destroyed in the joint in which pronounced inflammatory processes occur. Therefore, they are practically useless to administer to those patients whose gonarthrosis occurs against the background of the active stage of arthritis. But they are useful to use in stable remission of arthritis for the treatment of secondary gonarthrosis.
With primary gonarthrosis, you also need to pay attention to similar points. For example, if a patient’s joint is “bursting” from the accumulation of excess, pathological fluid, it makes sense to first “extinguish” the symptoms of synovitis (inflammation) and remove excess pathological fluid by means of a preliminary intra-articular injection of hormones or taking non-steroidal anti-inflammatory drugs. And only then inject hyaluronic acid into the joint, freed from inflammatory elements.
In addition to corticosteroid hormones and hyaluronic acid preparations, attempts are being made to introduce various chondroprotectors into the joint, such as alflutop, chondrolone or the homeopathic drug Cel T.
But these drugs are several times less effective than hyaluronic acid drugs. They help at most 50% of patients, and it is impossible to predict in advance whether their use will have an effect or not. In addition, a course of treatment requires 5 to 20 injections into the joint, which, as we said, is fraught with possible injury to the joint and various complications.
***
Manual therapy and physiotherapy:
Manual therapy for gonarthrosis of stages I and II often gives excellent results. Sometimes several procedures are enough for the patient to feel significant relief. Manual therapy of the knee joints helps especially well if it is combined with joint traction, taking chondroprotectors and intra-articular injections of Ostenil.
This combination of treatment procedures, from my point of view, is much more effective than the numerous physiotherapeutic measures offered in any clinic. Let me give you one example from practice.
A case from the practice of Dr. Evdokimenko.
A 47-year-old woman came to the appointment with stage II arthrosis of the right knee joint. By the time we met, she had been ill for 5 years. Over the years, the woman managed to experience all the possible methods of physiotherapy that can only be offered in our regional clinics: laser, magnetic therapy, ultrasound, phonophoresis, etc. Despite all the efforts of the physiotherapists, the condition of the patient’s joints continued to deteriorate - and this is natural. , since, say, chondroprotectors were prescribed to a woman only once in a short course over the entire five years.
In complete despair, the woman decided to take extreme measures - she underwent a course of treatment using burning wormwood cigarettes according to the Eastern method. As a result, the knee was covered with scars from burns, but it did not move better. And it was unlikely that she could - despite all my respect for Eastern medicine, I understand that wormwood moxibustion cannot eliminate bone deformities and increase the distance between the bones articulated in the knee.
After numerous physiotherapeutic procedures and even burning with wormwood cigarettes did not help the woman, she practically agreed to surgical treatment. But then I changed my mind and decided to try the complex method I proposed.
The first treatment session was, as they say, “creaky” - we only managed to “stir” the joint a little with the help of manual mobilization. Therefore, we scheduled the next session after preliminary preparation: for 3 weeks the woman took chondroprotectors, did self-massage and compresses with dimexide. After 3 weeks, I started again with mobilization of the joint and then repositioned (“set”) the joint using manual manipulation. There was a click and suddenly the joint began to move much easier and more freely. The woman felt obvious relief.
In the next two sessions, we consolidated the achieved improvement using mobilization, after which we consolidated the success with two intra-articular injections of Ostenil. And after a month and a half from the start of our not very intensive treatment (after all, we only needed six meetings), the woman was finally able to throw away the stick that was boring her and began to move quite freely.
Two years have passed since then. Twice a year the patient takes a short course of chondroprotectors, and occasionally comes to me for a follow-up appointment, where I am pleased to note that the condition of the knee is only getting better from year to year. And now even the first stage of arthrosis would be very difficult to predict - the patient’s knee joint has been restored almost completely.
Thus, only six treatment sessions (manual therapy plus intra-articular injections of Ostenil) in combination with a course of chondroprotectors turned out to be more effective than five years of physical therapy.
From this story (and by no means the only one of its kind) it becomes clear why I consider physiotherapy important, but only an additional part of the treatment program for gonarthrosis. In this sense, more than other procedures, I like laser therapy, thermal treatment (ozokerite, paraffin therapy, therapeutic mud) and especially cryotherapy (treatment with local cooling).
More details about each individual method of physiotherapy are described in the book “Pain in the Legs”.
***
Diet:
Diet for arthrosis is also very important.
You can read more about the anti-arthrosis diet here*
***
Using a cane:
Leaning on a stick when walking, patients with arthrosis of the knee joints seriously help their treatment, since the stick takes on 30 - 40% of the load intended for the joint.
It is important to choose a stick according to your height. To do this, stand up straight, lower your arms and measure the distance from your wrist (not your fingertips!) to the floor. This is exactly the length the cane should be. When buying a stick, pay attention to its end - it should be equipped with a rubber nozzle. Such a stick cushions and does not slip when people lean on it.
Remember that if your left leg hurts, then you should hold the stick in your right hand, and vice versa. When taking a step with your affected leg, transfer part of your body weight to the stick.
***
Physiotherapy:
The most important method of treating arthrosis of the knee joints is special therapeutic exercises. Almost no person suffering from gonarthrosis will be able to achieve real improvement in their condition without therapeutic exercises.
After all, in no other way is it possible to strengthen muscles, “pump” blood vessels and activate blood flow as much as this can be achieved with the help of special exercises.
At the same time, Dr. Evdokimenko’s gymnastics is almost the only treatment method that does not require financial costs for the purchase of equipment or medications. All the patient needs is two square meters of free space in the room and a rug or blanket thrown on the floor.
Nothing more is needed except consultation with a gymnastics specialist and the desire of the patient himself to do this gymnastics. True, most sufferers do not have this desire. Almost every patient in whom I detect arthrosis during examination has to be literally persuaded to engage in physical therapy. And it is most often possible to convince a person only when it comes to the inevitability of surgical intervention.
The second “gymnastic” problem is that even those patients who are committed to physical therapy often cannot find the necessary sets of exercises. Of course, there are brochures for sale for patients with arthrosis, but the competence of a number of authors is questionable - after all, some of them do not have a medical education.
This means that such “teachers” themselves do not always understand the meaning of individual exercises and the mechanism of their action on sore joints. Often, gymnastic complexes are simply thoughtlessly copied from one brochure to another. At the same time, they contain such recommendations that you can just grab your head!
For example, many brochures instruct a patient with knee arthrosis to “do at least 100 squats a day and walk as much as possible.”
Often patients follow such advice without first consulting a doctor, and then sincerely wonder why they feel worse. Well, I’ll try to explain why the condition of sore joints from such exercises, as a rule, only worsens.
Let's think of a joint as a bearing. Damaged by arthrosis, the diseased joint has already lost its ideal shape. The surface of the “bearing” (or cartilage) is no longer smooth. Moreover, cracks, potholes and “burrs” appeared on it. Plus, the lubricant inside the sphere had thickened and dried out, and it was clearly not enough.
Try to put such a structure into operation and, in addition, give it a load beyond the norm. Do you think that due to excessive rotation, such a deformed “bearing” can become smoother and more even, and the lubricant more liquid and “sliding”? Or, on the contrary, will the entire structure quickly wear out, become loose and collapse? In my opinion, the answer is obvious: such a “bearing” will collapse prematurely due to excessive load. In the same way, any bearings are destroyed and worn out during movement if, for example, sand gets into the lubricant and excessive friction occurs.
It is not difficult to understand that already damaged, cracked and “dried out” joints are destroyed by stress in the same way. This means that from exercises that create excessive stress on sore joints, these same joints will only get worse.
So maybe if you have arthrosis you can’t do gymnastics at all? Nothing like that is possible and even necessary. As already mentioned, gymnastics is an important method of treating arthrosis. However, of all the exercises, it is necessary to choose only those that strengthen the muscles of the affected limb and the ligaments of the diseased joint, but do not force it to bend and unbend excessively.
Probably, after such a recommendation, many of the readers will be surprised: how can you load the muscles and ligaments of a limb without forcing its joints to bend and straighten?
In fact, everything is very simple. Instead of the fast dynamic exercises we are accustomed to, that is, active flexion and extension of the legs, we need to do static exercises. For example, if, while lying on your back, you slightly lift your straightened leg up and keep it suspended, then after a minute or two you will feel fatigue in the muscles of your leg and abdomen, although the joints in this case did not work (did not move). This is an example of a static exercise.
Another variant. You can very slowly raise your straightened leg to a height of 15 - from the floor and slowly lower it. After 8 to 10 such slow exercises, you will also feel tired. This is an example of a gentle dynamic exercise.
It’s a completely different matter if the exercise is performed quickly and energetically, with maximum amplitude. By swinging your legs or actively squatting, you put increased stress on your joints, and their destruction accelerates. But the muscles, oddly enough, are strengthened much worse with such movements. We conclude: to strengthen muscles and ligaments with arthrosis, exercises should be done either statically, fixing the position for a certain time, or slowly dynamically.
By the way, it is slow dynamic and static exercises that most of my patients do not like to do, since they are especially difficult to perform. But this is how it should be: correctly selected, these exercises strengthen those muscles and ligaments that have atrophied in a person due to illness. Therefore, at first, be patient.
When doing gymnastics, do not rush. If you want to recover, you will somehow have to train yourself to do the exercises slowly and smoothly, without jerking. A jerking effort can only “tear” the muscles and will bring absolutely no benefit. And remember: if some exercise causes sharp pain, it means that it is contraindicated for you or you are doing it incorrectly. In this case, be sure to consult with your doctor about the correct execution of this exercise.
A video with gymnastics for the treatment of arthrosis of the knee joints can be viewed here *
At the end of the section on the treatment of arthrosis of the knee joint, I would like to address one question that patients often ask me: is it necessary to exercise the leg by walking for a long time and is walking useful for gonarthrosis?
I answer: of course, for a healthy person, long walking is useful in every sense - for the heart, for the respiratory system, for blood vessels, for the legs, etc. But with arthrosis, especially advanced, the knee joints cannot cope with even the minimum daily load, and here We invite you to download even more of them! Such actions will most likely only lead to aggravation and further destruction of the joints.
Before loading, or rather overloading, your knees, you must first relieve the aggravation, strengthen the leg muscles and properly treat the sore joints. Only then can you move on to active everyday activities, gradually increasing the load and in no case allowing pain.
***
Article by Dr. Evdokimenko© for the book “Pain in the Legs”, published in 2004. Edited in 2011. All rights reserved.
READ MORE:
- Arthrosis of the knee joint (gonarthrosis). Symptoms, stages.
- What is arthrosis of the knee joint (gonarthrosis) often confused with?
- Examination for arthrosis of the knee joint (gonarthrosis)
- Causes of arthrosis of the knee joint (gonarthrosis)
- Changes in the knee joint with gonarthrosis
- The best exercises for the treatment of gonarthrosis
Chapters from other books by Dr. Evdokimenko
Chondroprotectors
Such drugs are taken for degenerative-dystrophic diseases of the joints and spine to protect hyaline cartilage. The process of destruction of cartilage tissue during arthrosis and arthritis is progressive and irreversible. It can be slowed down with the help of chondroprotectors, which are especially effective when they “directly hit” the joint cavity. They improve local metabolism and nutrition of intra-articular tissues, and most importantly, stimulate the synthesis of their own collagen.
Collagen is the main component of cartilage, which performs a protective function. Thanks to the cartilage coating, the articular surfaces of the bones slide rather than rub, and movement does not cause pain. Most often, doctors prescribe Alflutop; the frequency and duration of the course is determined individually. The minimum number of injections is 5.
Causes of arthrosis and its features
This disease has several reasons why it occurs. These include:
- hormonal and metabolic disorders;
- poor blood supply to the joints;
- heredity;
- advanced age;
- joint injuries;
- excess weight.
With arthrosis, collagen and proteoglycans (complex proteins) that make up cartilage are destroyed. Gradually it becomes less elastic, then begins to crack, exposing the bone. The cartilage ceases to perform its function - shock absorption and uniform distribution of load during movement. The exposed bone is injured, and bone growths appear in the cartilage tissue. In the final stages, treatment of arthrosis with chondroprotectors, that is, medications, may no longer be effective and surgical intervention will be required.
Statistics show that arthrosis affects 6 to 12% of the population. With every decade, this disease makes more and more people disabled. At the same time, women suffer from it twice as often, although by the age of 65 there is practically no difference. By this age, more than half of people already suffer from arthrosis.
Not only the elderly, but also professional athletes and dancers are at risk. Arthrosis affects those who have the problem of a curved spine, excess weight, as well as lovers of high heels.
Treatment of the disease is long and difficult, so it is better to prevent it. Excessive physical activity with heavy weights, injuries and sudden movements should be avoided. Pay attention to preventive exercises, maintain weight within normal limits. And if the disease has already made itself felt, it is important not to miss these first “bells” and start treatment on time. If it is diagnosed in a timely manner, it can be completely cured with the help of drugs that are aimed at restoring cartilage tissue. They are called chondroprotectors.
Hyaluronic acid
It is also called a “synovial fluid prosthesis”, since hyaluronic acid acts as a lubricant that protects the joint from injury. It normalizes the composition of the synovium, which becomes denser and more viscous. Hyaluronic acid perfectly relieves pain and inflammation, activates the processes of self-regeneration of cartilage. Its most common use is in patients with arthrosis. With this remedy, injections are often made into the hip joint and knees. The standard course of treatment consists of 3-5 procedures with a week interval between them. The effect lasts for a long time, up to 1 year. The most frequently prescribed drugs with “natural lubrication” are Gialgan, Hi-Flex, Gialsin.
Classification of chondroprotectors for arthrosis
These drugs can be classified according to how long ago arthrosis has been treated with chondroprotectors in medical practice:
- first generation, which are becoming less and less effective;
- second generation - chondroprotectors for joint arthrosis with complex effects, which include glucosamine and chondroitin;
- third generation - drugs that are distinguished by the highest degree of purification and the most effective combination of components.
The latest generation of drugs, which are considered one of the best chondroprotectors for arthrosis, includes Artradol.
Carbon dioxide (carboxytherapy)
The effect of carboxytherapy is based on the property of carbon dioxide to cause oxygen starvation in tissues. Gas injections are given through a special device, and after the injection the body strives to enrich the joint with oxygen, increasing its blood supply. Metabolism accelerates sharply, and much more nutrients are supplied to damaged structures. In a matter of minutes, carbon dioxide leaves the joint cavity, and the effect remains for a long time.
Attention! The advantage of this unique technique is the absence of side effects, since CO2 is a natural element, a product of metabolic processes.
Carbon dioxide treatment was developed by Czech specialists from the city of Karlovy Vary, where the famous sanatorium is located. It has been successfully treating diseases of the musculoskeletal system for more than a century.
PRP therapy
PRP stands for platelet-rich plasma. Platrlet rich plasma. Platelets are responsible for the formation of blood clots - blood clots that can clog damaged blood vessels. Platelets also actively participate in the processes of cleansing wounds of unnecessary proteins and stimulate the activity of fibroblasts. The latter are responsible for the production of collagen and elastin, which are the basis of connective tissue.
PRP therapy is injections for joint pain that have a number of advantages:
- do not cause allergies or side effects;
- rarely lead to the development of complications; (hormones);
- vitamins;
- do not transmit infection..
These advantages are due to the use of the patient’s own blood, which is completely compatible with body tissues. To improve the effect, plasma administration can be combined with hyaluronic acid preparations.
Evaluation of results
Starting from the 1st month of treatment, patients of all three groups began to notice a decrease in pain and other clinical signs of the disease, but significantly more significant changes in indicators were observed in group I.
When analyzing the results of treatment in a group of patients with OA of the knee joints who received Flexinovo 1 tablet once a day for 3 months, there was a decrease in pain when moving according to VAS by the 3rd month of observation from 7.44 ± 1.51 to 3.3 ±0.96. In the same group, there was a significant decrease in pain at rest according to VAS from 3.44 ± 0.74 to 1.12 ± 0.31. The Lequesne functional index in this group of patients decreased from 6.6±1.19 to 4.35±0.49.
In group 2 of patients with polyosteoartosis, positive dynamics were also noted: a decrease in pain when moving according to VAS from 7.52±3.7 to 3.7±0.96 by the 3rd month of observation. At rest, pain in group 2 decreased from 3.37±0.81 to 1.41±0.54. The Lequesne functional index in this group of patients decreased from 6.5±1.36 to 4.5±0.51.
In group 3 of patients with OA of the hip joints, the pain index during movement decreased from 8.6±1.37 to 4.24±0.98, and the pain index at rest from 3.44±0.72 to 2.5±0. 81 by 3 month follow-up. At the same time, the Lequesne functional index also decreased from 6.8±1.23 to 5.3±0.81.
Thus, in all three groups, after 3 months of treatment, there was a significant decrease in the VAS pain index during movement (Fig. 2) and at rest (Fig. 3).
Rice. 2 VAS pain index when moving
Rice. 3 VAS pain index at rest
After three weeks of taking Flexinovo, the Lequesne index decreased in all three groups, but the most significant decrease in this indicator was noted in the knee OA group (Fig. 4).
Rice. 4. Lequesne functional index
Flexinovo made it possible to reduce or completely eliminate the use of traditional analgesics in patients of all three groups.
Three months after the start of therapy, 23% of patients were taking analgesics on demand, and 77% of patients were completely off pain medications (Fig. 5).
Rice. 5 Change in the proportion of patients taking NSAIDs while taking Flexinovo
The drug was well tolerated. Patients demonstrated high adherence to therapy. No side effects were identified when taking Flexinovo.
Advantages
- The drugs dissolve very slowly, up to 12 months.
- They have a local effect on all joint tissues.
- Almost do not enter the systemic circulation and do not affect the functioning of internal organs.
- Thanks to the previous point, they can be used in patients with severe concomitant pathologies, when treatment with other methods is unacceptable.
- Intra-articular injections help avoid surgery.
- After the procedure, no rehabilitation is required; the doctor can only apply a tight bandage and warn against excessive physical exertion.
Indications
- osteoarthritis;
- arthritis;
- bursitis;
- synovitis;
- tendinitis.
Joint diseases are very common, especially among older people. If you are one of them, or the time has come to repeat the course of treatment, call us. Our center employs high-level specialists with extensive experience, making patients feel comfortable and confident. If necessary, you will be prescribed one or more intra-articular injection procedures and a drug will be selected based on the indications.
Are chondroprotectors as effective as we are told?
According to manufacturers, chondroitin and glucosamine restore cartilage tissue in the joint and protect it from destruction. They contain components that replicate the structure of hyaline cartilage, which explains this effect. To get any results, you need to take the drugs for a long time, several months.
Many patients note that even after a long period of use, chondroprotectors did not give any result at all. This is also confirmed by x-rays, in which the size of the joint space remained the same, and sometimes decreased.
Drugs with a chondroprotective effect only help people with early stages of arthrosis. At stages 2 and 3 of coxarthrosis or gonarthrosis, there is no result from them: stronger drugs are needed. In such cases, it is advisable to undergo a course of intra-articular injections of Noltrex or decide on endoprosthetics if the joint is severely damaged and conservative treatment does not help.
Proponents of chondroprotectors often remain silent about what side effects are possible after long-term use of these drugs. Watch the video on this topic and draw your own conclusions: