“Walking barefoot is beneficial,” we often tell our children, without even thinking about what exactly this benefit consists of. Orthopedic doctors actually recommend regularly walking barefoot on sand, mown grass, loose soil, and on a high-pile rug. This is a good exercise for the feet, as it strengthens the muscles and improves blood circulation. It is a pity that adults themselves often do not follow the advice they give to children. On the contrary, for the sake of fashion, they wear narrow, uncomfortable shoes, high-heeled shoes... And as a result, they risk getting a whole range of diseases. Arthrosis of the 1st metatarsophalangeal joint of the foot is one of them.
Like any other type of arthrosis, this is a degenerative disease in which the cartilage that provides joint mobility is gradually destroyed. The surfaces of the foot bones it connects are deformed, and osteochondral exostoses—bone spines—are formed in the joint area. They limit movement in the joint and cause periodic exacerbations - pain, swelling, inflammation.
A common cause of arthrosis is trauma. And this is not only about heavy objects falling on your feet or frequent bruising of a finger. Wearing tight shoes or high heels causes a strong traumatic effect.
Congenital predisposition plays a major role in the development of arthrosis. For example, anatomical features such as pronation of the foot, hollow foot deformity, high standing or excess length of the metatarsal bone.
The likelihood of developing arthrosis increases with age. Risk factors include diabetes, gout, and rheumatoid arthritis. And also – an advanced form of hallux valgus deformity of the 1st toe. Or – medical errors during foot surgery (when treating valgus, for example).
Who's at risk
Arthrosis of the hands, or interphalangeal joints of the fingers, develops in old age. Women are ten times more susceptible to it than men. You should be especially careful:
- those whose relatives have a history of arthrosis, regardless of the affected joint (the disease is often hereditary);
- whose type of activity involves stress on the hands, for example, representatives of agriculture, computer typing operators, seamstresses;
- who has congenital defects in the structure of the ligamentous apparatus of the hands or interphalangeal joints;
- who suffered injuries;
- who is obese;
- who have already been diagnosed with rheumatoid arthritis, psoriasis or diabetes.
In women during menopause, estrogen synthesis decreases, which leads to a number of diseases, including osteoporosis and arthrosis, including the joints of the hands.
Do you do manual labor? Pay attention to the slightest problems with your fingers
Why is it developing?
Just imagine: the ankle joint can withstand a load that is 6-7 times the human body weight. The reason for this is the complex anatomical structure, as well as the characteristic plexus of ligaments, muscles and fascia. It is not surprising that microtraumas occur in this area of the musculoskeletal system more often than others.
People at risk for developing ankle arthrosis:
- overweight;
- with metabolic disorders;
- after injury or inflammation of cartilage tissue.
Excess weight is an additional load on the ankle: the risk of developing arthrosis increases
What is deforming arthrosis of the ankle and what are the reasons for its development? What traditional and folk methods of treatment are used today?
Arthrosis of the interphalangeal joints goes through the following stages of development:
As is the case with diseases of other joints, deformities in the interphalangeal joints progress very slowly, so a person may not notice the problem for a long time. But even the slightest discomfort in the fingers should alert you.
- At the first stage, arthrosis of the hands can be recognized by a characteristic crunching sound in the fingers during extension and flexion. The pain is minor, aching, dull or bursting, and occurs periodically, for example, after heavy exertion. Sometimes swelling appears at the interphalangeal joints.
Already at the first stage of arthrosis, the fingers may periodically swell
- In the second stage, the pain becomes more intense and lasts longer, especially at night. Pulsation and burning appear in the joints. In place of the swelling, usually symmetrically on both hands, growths of bone tissue are noticeable - Heberden's nodes. It becomes uncomfortable for a person to move already slightly deformed fingers.
Heberden's nodes are a characteristic symptom of the second stage of arthrosis of the hands
- The third stage indicates the complete destruction of the cartilage tissue of the interphalangeal joints. Bone growths increase in size and merge, which leads to curvature of the fingers and complete limitation of their mobility. The person experiences constant aching pain. Ankyloses often appear - areas of fused bone surfaces.
Symptoms of hallux limitus/hallux rigidus
Pain
. At the early stage of the disease (hallux limitus), pain in the joint occurs only periodically - under heavy loads. But the longer you ignore the problem, the more frequent and severe the attacks become. Soon pain becomes an indispensable companion when walking. And in the later stages it does not disappear, even when the patient’s legs are at rest.
About limited mobility
in the joint in the early stages of arthrosis (hallux limitus) is minimal. But with severe arthrosis (hallux rigidus), it becomes more and more difficult to move the finger - first of all, to lift it. Ultimately, arthrosis leads to the almost complete inability to move a finger.
Lameness
appears inevitably due to pain. With severe arthrosis of the 1st metatarsophalangeal joint, patients involuntarily begin to shift weight to the outer edge of the foot when walking. This, in turn, leads to the formation of painful calluses in the area of the 4th and 5th metatarsals and under the main phalanx of the first toe.
Joint deformity
. Due to the presence of bone spines (exostoses), thickening of the metatarsal head is observed. The deformation becomes more noticeable over time.
Inflammation
.
When arthrosis worsens, swelling is periodically observed, the skin turns red, and the temperature rises. Diagnosis of the disease in the clinic does not take much time. The podiatrist examines the foot and takes x-rays. With arthrosis, x-rays clearly show narrowing of the joint space and bone exostoses.
The main principles of treatment of arthrosis of the hands
The choice of treatment methods in traditional medicine depends on the stage of the disease. Until the cartilage is destroyed, it makes sense to try different approaches:
- taking chondroprotectors to improve nutrition and restore metabolic processes in cartilage tissue (courses are quite long and do not give results immediately);
- taking non-steroidal anti-inflammatory drugs;
- if synovitis or arthritis of an inflammatory nature has developed against the background of arthrosis, corticosteroid hormones are often prescribed.
Drug treatment of arthrosis and osteoarthritis of the hands is aimed at relieving a person of pain and reducing symptoms. However, it is quite difficult to completely cure the disease with their help or achieve stable remission for a period of a year or two.
Drug treatment for arthrosis of the hands is aimed at combating the symptoms, not the cause.
The hands consist of the most fragile joints that are susceptible to damage. Simple exercises help improve blood circulation and maintain good physical condition:
Before treating deforming osteoarthritis of the foot joints
Before treating osteoarthritis of the foot, it is necessary to conduct a series of examinations. An x-ray will allow you to accurately determine the degree of destruction of the articular surfaces. If the image shows bone deformations and thinning of the cartilaginous synovial tissue, a decrease in joint spaces, then we can safely say that the patient has a 2-3 degree deformity. And at the initial stage, an X-ray image at stages 1-2 of osteoarthritis will show only a decrease in the height of the cartilage pad. There are no deformations of the bone structure yet. And it is at this stage that complete recovery is possible without surgery.
Therefore, if you have signs of trouble in the small joints of your feet, do not delay visiting the doctor. The doctor will conduct an examination and prescribe the necessary examinations to clarify the diagnosis. Then it will be possible to effectively treat deforming osteoarthritis of the joints of the feet using all available modern means and techniques.
What other methods are used?
- Manual influence on the interphalangeal joints - percussion massage, finger stretching, kneading.
- Therapeutic exercise – squeezing and unclenching fingers.
- Physiotherapy – paraffin and ozokerite applications, laser and magnetic therapy.
The procedures in question are auxiliary in the complex treatment of arthrosis; they require a lot of effort and time, while providing an insignificant alleviating effect.
Gymnastics for arthrosis of the hands improves blood circulation
How to eat properly with arthrosis of the hands
Taking chondroprotectors and other medications makes no sense if you do not provide the cartilage tissue with proper nutrition. Nutritionists and doctors recommend eating red salmon fish, vegetable oils and nuts for this diagnosis. These products are an optimal source of polyunsaturated fatty acids.
It is very important to diversify your diet with B vitamins and folic acid, which are found in wholemeal bread, sprouted cereals, beans, cabbage, lentils, bananas and fermented milk products. Alcohol and high-calorie foods are taboo.
How does the liquid endoprosthesis "Noltrex" work?
- The drug is injected into the joint in a medical office, covering the articular surfaces and synovial membrane with an even layer. Noltrex has the consistency of a hydrogel, so it performs a shock-absorbing function - it softens the mechanical stress on the joint and stops its destruction.
- The viscosity characteristics of the Noltrex hydrogel are close to natural, therefore, after its administration, the physical properties of the joint environment are quickly restored.
- After the appearance of artificial synovial fluid, the joint space in the interphalangeal joints expands - the surfaces stop rubbing, and the pain disappears.
Arthrosis of the 1st metatarsophalangeal joint (Hallux rigidus)
Surgical treatment is indicated for patients for whom conservative treatment has proven ineffective.
Patients should be aware that the choice of surgical treatment must be carefully considered.
Any surgical treatment option must be approached carefully, giving preference primarily to less invasive and traumatic interventions.
There are several options for surgical treatment, each of which is selected based on the individual characteristics of the patient and the stage of the disease:
- Stage 0-1 - redressal under general anesthesia and local injection therapy.
- 1-2 degree:
- cheilectomy - removal of excess bone growths (osteophytes) and damaged joint tissues;
- microfracture is a surgical technology for the restoration of articular cartilage, which consists in the formation of microfractures of the underlying subchondral bone plate in the area of the cartilage defect. This leads to the formation of blood clotting in the defect area, the release of growth factors and promotes the formation of new cartilage;
- various types of osteotomies that reduce the load on the joint or Moberg wedge osteotomy.
- arthrodesis of the 1st MCP joint;
Generally speaking, patients who note pain in the area of a large osteophyte on the dorsal surface of the 1st MCP joint and a limitation in the range of motion of the 1st finger in the absence of pain in the middle (between dorsiflexion and plantar flexion) position of the finger are considered candidates for joint-saving surgery - cheilectomy - or osteotomy decompressing the first metatarsophalangeal joint.
For patients who note constant pain, including in the middle position of the finger, arthrodesis of the 1st MCP joint or hemiarthroplasty is indicated.
Cheilectomy
Cheilectomy can be called “putting things in order” in the joint. This operation includes the following steps:
- removal of a large dorsal osteophyte of the head of the 1st metatarsal bone;
- resection of the dorsal 1/3 of the articular surface of the head of the 1st metatarsal bone;
- synovectomy (removal of the inflamed inner lining of the joint);
- removal of loose articular bodies;
- removal of excess bone growths on the dorsal surface of the proximal phalanx of the 1st finger.
The effectiveness of this operation is about 85%. Efficiency means relief of pain and restoration of an acceptable range of motion of the 1st finger. In 15% of patients, symptoms persist or return again due to the progression of degenerative joint damage and the persistence of areas of damaged cartilage in the central part of the joint.
The operation can be performed minimally invasively or using a mini-open approach. Whenever possible, we always try to perform such operations in a minimally invasive manner.
Cheilectomy has the following advantages:
- joint preservation;
- maintaining movements in the joint;
- maintaining joint stability;
- this operation does not complicate any other subsequent interventions on the joint, if any are needed.
The operation is performed under general anesthesia and is, in fact, an “outpatient” operation.
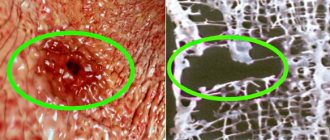
X-ray of the foot: A - a large dorsal osteophyte is noted; B - schematically shows the areas of bone resected during cheilectomy
This operation is more effective in patients who have cartilage damage only in the peripheral parts of the joint; these areas can be removed during surgery. With central cartilage defects, the effect is not so pronounced and the disease continues to progress, involving new parts of the joint in the process.
Microfracturing
This technique is performed simultaneously with a cheilectomy. In a number of patients whose central cartilage defects are quite small, closure (arthrodesis) of the joint is undesirable, since most articular surfaces still have a healthy cartilaginous cover, and the range of motion in the joint is quite significant.
Microfracture is used for interventions on the hip, knee and first toe joint. It involves removing damaged (loose, loose and exfoliated) cartilage and forming micro-holes in the underlying bone plate. Through these holes, the defect area is filled with bone marrow cells, a blood clot rich in growth factors is formed, which stimulates the formation of new cartilage tissue. The newly formed cartilage is called fibrocartilage and is similar in structure to a scar on the skin. It, of course, differs in its properties from normal articular cartilage, but it is still better than nothing at all. Its basic characteristics are the same as those of normal hyaline cartilage, but it is not as strong and durable.
In the short and medium term, good to excellent results are observed in 75% of patients. Long-term treatment results are difficult to predict. This operation is a good option for patients for whom it is too early to talk about arthrodesis or endoprosthetics.
Surgeries for decompression of the 1st metatarsophalangeal joint
Decompression of the joint of the 1st toe refers to a surgical intervention aimed at reducing the pressure on each other of the articular surfaces of the first metatarsal bone and the phalanx of the big toe. Decompression is achieved by slightly shortening the metatarsal bone. In practice, a shortening SCARF osteotomy is usually used. As a result of a decrease in the length of the metatarsal bone, the joint space becomes wedged and widens, and the range of motion in the big toe joint increases. Decompression surgeries are usually performed in combination with a cheilectomy. According to scientists, patients note a significant decrease in pain and an increase in the range of motion in the first finger after such an operation. The results usually last for 5–7 years.
Moberg operation – closing dorsal wedge osteotomy
Moberg's operation is indicated for a number of patients for whom dorsiflexion of the 1st finger is critical, for example, runners and dancers. It can also be performed in addition to or after cheilectomy.
This operation consists of resection of a wedge-shaped bone fragment at the base of the 1st finger, which increases the dorsiflexion of the 1st finger, but this is achieved at the cost of reducing the amount of plantar flexion of the 1st finger.
The operation is performed under general anesthesia and is, in fact, an “outpatient” operation.
During the Moberg operation, a bone wedge (yellow triangle) is removed from the dorsal surface of the proximal phalanx of the 1st finger, which leads to increased dorsiflexion of the finger
Arthrodesis of the 1st MCP joint
Arthrodesis of the 1st MCP joint provides excellent results in terms of pain relief and return to normal daily activities.
The operation consists of removing all damaged parts of the joint (cartilage) and creating conditions for fusion of the bones that form the joint, i.e. closure of the joint. No joint means no movement and therefore no pain. The purpose of the operation is to eliminate pain at the cost of joint mobility.
Most patients are anxious about the idea of joint closure when they first hear about such an operation. This is quite understandable - after all, the joint is created in order to move. And the closure of a joint is the exact opposite of its mobility, which seems unnatural. In fact, after arthrodesis, you most likely will not even limp and will become much more active than before it.
The operation is usually performed from a single access from the inside of the 1st MCP joint, under general anesthesia and in most cases on an outpatient basis.
The main complication is impaired bone fusion. According to numerous studies, the incidence of this complication is 5–10%. In such cases, the operation is repeated and supplemented with bone grafting to stimulate healing, with the result that most patients eventually achieve union.
Today, arthrodesis of the 1st MCP joint remains the method of choice in the treatment of end-stage osteoarthritis of the 1st MCP joint. In such cases, endoprosthetics of the 1st MCP joint is also possible, but the indications for it remain the subject of debate, and the results are quite contradictory.
For patients who do not want repeated interventions, it probably makes sense to opt for arthrodesis, since hemiarthroplasty and total endoprosthetics of the 1st MCP joint are accompanied by a higher incidence of complications requiring repeated operations.
After arthrodesis, patients can wear heels up to 5 cm high.
A – The radiograph shows a massive dorsal osteophyte, which is the source of pain for the patient and problems with wearing shoes; B — the patient underwent osteophyte resection and arthrodesis of the 1st MCP joint
Radiographs before (A) and after (B) arthrodesis of the 1st MCP joint (one of the fixing screws was removed because it caused skin irritation)
Fixation of bones during arthrodesis of the 1st MTPJ is performed using 1-2 screws or 1 screw and a plate.
Advantages of screw fixation:
- small access;
- faster fusion;
- fewer complications.
Disadvantages of screw fixation:
- the need to avoid stress for 6 weeks.
Advantages of using the record:
- possibility of dosed loading immediately after surgery.
Disadvantages of using a record:
- longer access;
- potentially higher complication rates.
Is it dangerous?
Many people diagnosed with arthrosis are afraid of intra-articular injections. In fact, the introduction of a synthetic endoprosthesis under medical supervision does not pose any danger:
- the molecules of the drug are inert and do not interact with body tissues, so the drug does not cause rejection or allergies;
- the medicine has no side effects, there may be a slight burning sensation in the joints, which can be relieved with analgesics or goes away on its own after 12-24 hours.
The synthetic components in Noltrex are not recognized by the body's immune cells, so the drug, unlike its natural analogues, remains in the joint for a long time. This explains its long-term effect - from 9 months to two years, depending on the degree of damage to the interphalangeal joint.
Compared to other methods of treating arthrosis, Noltrex intra-articular injections have a significant advantage: both doctors and patients note their effectiveness and safety, and most importantly, quick results!