- What types of arthritis are massaged for?
- Traumatic arthritis
- Periarthritis
- Massage for arthrosis of the shoulder joint
- How is massage done?
- The effectiveness of shoulder massage
For shoulder arthrosis and some types of arthritis, massage is used. It helps reduce the symptoms of the disease, improve tissue trophism and prevent muscle atrophy. The procedure has both immediate and long-term effects. Immediately after the massage, a person’s pain, swelling decreases, and muscles relax. Regular procedures allow you to develop the joint, improve its function, reduce the amount of effusion, and strengthen the muscles by improving their blood supply.
massage
massage
- microcrystalline arthritis
- autoimmune (rheumatic);
- infectious (septic).
For most types of arthritis, massage can be used. The exception is septic arthritis. In the acute phase, antibacterial treatment is required. Only after its completion can physiotherapeutic procedures and massage be carried out. It is used as a method of recovery after illness. Other inflammatory processes are most often chronic. Massage helps relieve the patient's condition, relieve pain and reduce the need for medications.
Traumatic arthritis
Arthritis of traumatic origin is usually associated with professional activities. A person performs the same movements for many months or years in a row. They do not cause acute injury, but provoke constant microtrauma of tissue. As a result, a chronic inflammatory process develops, which is accompanied by:
- pain;
- stiffness;
- pain in those movements that actually led to microtraumatic arthritis;
- crunching sound when moving;
- pain at rest along the nerve.
The purpose of massage is to eliminate pain or reduce it. It is also necessary to reduce the amount of effusion, prevent the occurrence of contractures and atrophic changes in muscles. They are possible as a result of prolonged restriction of movements in the limb. A person experiences pain, so he spares the sore arm, does not perform any movements in it and does not put any strain on it. This impairs blood circulation and leads to atrophic changes.
Massage for arthritis of the shoulder joint of microtraumatic origin is carried out carefully, without chopping techniques, tapping or squeezing. Especially if there are already signs of muscle atrophy. Vigorous rubbing is also avoided. First of all, this should not be done during the period of exacerbation of the symptoms of inflammation in the joint. Because rubbing may increase the amount of effusion. Massage the muscles above and below the shoulder. The duration of each session is from 10 to 15 minutes. A course requires up to 20 procedures.
At the same time, other measures are required to eliminate chronic inflammation in the shoulder joint. It is important to avoid repetitive microtrauma. A person will have to change his profession, since continuing to engage in this activity will inevitably lead to a recurrence of shoulder inflammation. For a long time, the limb requires functional rest. Over time, arthritis usually regresses.
Finger joint pain, arthritis and massage
Many people believe that arthritis and joint pain are inevitable as we age, but this is not true. Joint pain indicates tissue damage that causes inflammation. If pain occurs in a joint when moving, the brain sends a signal to the synovium of the joint, and it begins to synthesize more synovial fluid. Because of this, joint mobility decreases. Of course, in old age our joints will not be as flexible and mobile, but they should not hurt - this is a sign of pathology.
Arthritis is inflammation of a joint (Latin: arthrītis, “ache in the joints”). At its core, it is a collective name for many types of inflammatory joint diseases. These include:
• Traumatic arthritis
• Osteoarthritis
• Rheumatoid arthritis
• Psoriatic arthritis
Most often in practice we encounter traumatic arthritis, and it is quite simple to treat. I have worked with dozens of clients who have complained of pain in their finger joints over the years - even in such cases, the correct treatment gave very quick results, sometimes the pain went away within a week.
Traumatic arthritis of the finger joints
When a finger joint becomes inflamed, pain occurs and sometimes visible swelling and redness occur. In most cases, swelling is very difficult to notice because the finger joints are relatively small. Typically, the synovial membrane of a finger joint produces no more than one drop of synovial fluid, so increasing its volume to two or three drops already significantly affects the functionality of the joint. Inflammation of these joints is indicated by pain during passive flexion and extension of the finger (in this article you will find the most effective tests for diagnosing lesions of the joints of the fingers).
Sometimes during diagnosis it turns out that the client has several joints of his fingers affected by arthritis, but he knows only about the most painful ones. With mild inflammation and normal general physical condition, a person can help himself by gently stretching his finger joints. In addition, daily stretching goes well with hand massage, providing a synergistic effect.
Once you have managed the pain, teach the client to strengthen and stretch the fingers daily. Ask him what his job is. If he actively uses his fingers during the day (for example, working at the computer, sewing, etc.), advise him to do simple finger exercises during breaks.
During the recovery period, you should take time away from work more often. People with arthritis need to drink plenty of water and eat a healthy diet.
Never miss the opportunity to learn more about the client’s hobbies, the sports he is passionate about, and so on - very often the cause of pain in the finger joints lies precisely in these factors.
When the pain significantly decreases or goes away completely, move on to active stretching of each joint with auxiliary movements (for example, when stretching, the client can gently help himself with the other hand, the massage therapist can do the same). Stretching should be done in sessions for a couple of months, and then you can teach the client to do it on their own. Good luck!
Ben Benjamin
Periarthritis
Periarthritis
Not only the joints themselves can become inflamed, but also the tissue nearby. This phenomenon is called periarthritis. Mainly, the inflammatory process involves the sites of tendon attachment to the bone. These are the areas where collagen fibers and the periosteum connect. The disease is accompanied by degenerative-dystrophic changes. As a consequence, secondary reactive periarthritis develops.
The most common type of this disease is glenohumeral periarthritis. In addition, this is the most common pathology that affects the shoulder joint. In the vast majority of cases, the lesion is unilateral and localized on the right. The main role in the development of pathology is played by repeated microtrauma to the tendon. Usually the disease occurs against the background of physical activity.
Massage is used to reduce pain and inflammation in the tissues of the shoulder area. The procedure ensures a resolving and trophic effect. Massage improves joint function and helps reduce swelling by normalizing the outflow of lymph and venous blood.
First, the back, cervical and thoracic spine areas are massaged. They use stroking movements, various types of rubbing, and kneading. The joint capsule of the shoulder is massaged in front and behind. Particular attention is paid to the place of tendon fixation.
CAUSES AND ALARM SIGNS THAT MAY INDICATE FAILURE
Arthritis of the scapula - damage to the joint with the joint capsule, erosion due to inflammatory processes and synovitis in the shoulder articulation apparatus - can be provoked by the same circumstances that cause any type of arthritis:
- trauma (in the case of the scapula, this must be a serious injury or a mechanical blow of enormous force);
- infection without treatment;
- arthrosis, ankylosis or osteoarthritis due to age-related wear of the articular cartilage (the smooth surface of the scapula is damaged).
Manifestations of scapula arthritis may be delayed. Therefore, if there are any alarming signals, you should not postpone a visit to a rheumatologist - there is a possibility that the scapula bone is already affected by erosion and needs urgent support.
Characteristics of arthritis are:
- decreased mobility (in the case of damage to the scapula, stiffness is felt when trying to move the arm back, the amplitude of its movement is reduced);
- muscle damage or atrophy;
- discomfort on palpation of the scapula is often indicated by arthritis of the adjacent joint.
The basic symptom of scapular arthritis (scapulohumeral) is pain. It decreases under the influence of analgesics, but invariably returns, increasing with movement.
Detection of pathology in the scapular area
Since we are talking about damage to the smooth surface of the bone, the part adjacent to the joint, or the hard processes of the articulation of the scapula, the only informative diagnostic tool for arthritis remains an x-ray.
Depending on your symptoms, you may need:
- arthrography (x-ray with the introduction of a contrast mixture to determine the articular background of arthritis of the scapula);
- serial photographs or electroradiography;
- To assess the reactions of muscle tissue to bone inflammation, tomography is prescribed.
Arthritis of the scapula has similar symptoms to arthrosis, scapular periarthritis, and hypothermia of the spinal muscles. Pain under the scapula can be reflected in lesions of the sternum, osteophytes, kyphosis, lordosis. Given such a dubious background, it is important to conduct the most detailed examination to recognize lesions of the scapular part.
Massage for arthrosis of the shoulder joint
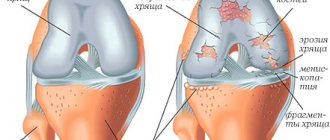
Osteoarthritis is a degenerative process in a joint. Cartilage gradually degrades. The surfaces of the bones are exposed and touch during movements, which provokes pain. Over time, fibrous tissue forms, the joint is completely destroyed, and its articular surfaces fuse together. This process takes many years. The disease develops gradually, but progresses steadily.
Primary arthrosis of the shoulder is rare. This disease is typical only for the joints of the lower extremities: hip and knee. Degenerative processes of the shoulder are usually secondary. That is, they develop against the background of another disease. Most often this is the result of injury.
osteonecrosis of the humeral head
osteonecrosis of the humeral head
Other causes:
- osteonecrosis of the humeral head;
- chondrocalcinosis;
- bone dysplasia;
- damage to the tendons of the rotator cuff muscles;
- previous infectious or autoimmune arthritis.
With arthrosis of the shoulder, its shape usually does not change. For character pathology, atrophy of the muscles of the shoulder girdle and upper limb.
In the treatment of arthrosis, the possibilities of massage are limited. Patients often require surgery. In the most severe situations, shoulder replacement is performed. Massage is used only as an auxiliary method. It is also used during the recovery phase after surgery.
Purposes of massage:
- pain reduction;
- elimination of swelling;
- prevention of atrophic changes in muscles;
- restoration of muscles already subject to atrophy by normalizing blood supply.
But massage does not lead to long-term clinical improvement. Arthrosis is characterized by a progressive course. The tissues inside the joint are damaged and degraded. Massage alone for shoulder arthrosis is not able to restore them. But the procedure helps reduce symptoms and improves the patient's quality of life.
Indications and contraindications for massage
When prescribing drug treatment, doctors take into account the patient’s age and lifestyle, general health, and external chronic processes. Joint diseases are also treated with additional methods: exercises, diet, physiotherapy and massage. Manual therapy and massage procedures are prescribed as a preventive measure against exacerbation of the disease.
Massage is indicated for gout, arthritis, arthrosis, ankylosing spondylitis. With it you can:
- reduce pain;
- relieve muscle tension;
- increase muscle tone and improve cell nutrition;
- relieve stiffness and limitation of mobility;
- restore normal limb movement;
- get rid of neurotic disorders.
Sessions are not carried out if:
- acute stage of inflammation;
- chronic osteomyelitis;
- skin diseases;
- active form of bone tuberculosis;
- neoplasms;
- dislocations;
- dystrophic processes;
- humeroscapular periarthrosis.
A temporary contraindication to massage is elevated body temperature and a feverish state. Self-prescribed sessions without consulting a doctor are impossible for these diseases: an incorrectly selected technique can provoke a sharp deterioration in well-being.
How to do a massage
How to do a massage
1. Start with stroking. Movements are performed in the proximal part of the arm. They go in the direction of the shoulder joint, upward. First, do a grasping stroke, then a circular stroke.
2. Next you should do cross rubbing with the edges of your palms. This procedure takes up to 20 seconds.
3. Proceed to rubbing with your fingertips. Spiral movements are performed. The exposure should not be excessively painful for the patient. Although in case of pain, it may cause slight discomfort.
4. Do rubbing and sliding. It is performed with the palms. Pressure should be applied to the shoulder from both front and back. You don't need to press so hard as to cause pain. But still, the impact should be sufficient for the skin to move. Circular movements are performed for up to 20 seconds.
5. Fading strokes. Performed with palms in the upward direction, from the middle of the shoulder to the shoulder joint.