Mechanism of operation
To get rid of back pain and restore joint mobility, tablets and ointments alone are not enough. The complex treatment includes robotic therapy devices for the upper and lower extremities and spine. The technique is most in demand in traumatology and orthopedics due to a number of effects:
- Stimulating effect. While working on active-passive mechanotherapy simulators, metabolic processes in tissues are accelerated and the vital potential of cells increases. Blood circulation is activated and the functioning of the respiratory system is improved. For diseases of the spine and joints, the result of therapy depends on the quality of the exercises and the amount of work done.
- Trophic impact. Thanks to the saturation of tissues with oxygen and nutrients, the process of healing and restoration is accelerated. The basis of the trophic effect is biochemical and physiological changes, due to which the energy potential of muscle fibers is restored. For example, in case of paralysis and paresis, mechanical massage prevents the development of muscle atrophy.
- Compensatory effect. Helps restore lost function of limb joints or adapt to new conditions in cases of severe biomechanical disorders.
- Normalizing mechanism. Expands the functional indicators of the affected areas of the body. This occurs due to regularly performed physical activity on the muscles. Mechanotherapy helps restore not only the function of the joints and spine, but also other systems in the body.
- General impact. It is known that mechanotherapy of joints improves blood circulation and lymph flow of the limb, metabolism in articular cartilage and muscles. Exercises on simulators increase stroke and minute blood volume, activate coronary blood supply, and increase physical endurance.
The entire set of exercises is carried out in a certain sequence, under the supervision of a doctor or exercise therapy instructor. The initial stage includes simple traditional loads: dynamic and cyclic exercises for 15-20 minutes. The training is completed with specific exercises lasting up to 30-60 minutes.
Advantages
Doctors choose mechanotherapy for their patients for the following advantages:
- Versatility
Mechanotherapy is allowed for spinal decompression and other complex conditions when it is necessary to restore the mobility of joints and muscles.
- Safety
When performed correctly, the exercises relieve axial load from the joints and prevent them from rubbing against each other, which eliminates any injuries. This is especially important after injuries, as well as in cases of damage resulting from arthrosis or ankylosis.
- Individual loads
The degree of load is selected individually, in accordance with the anthropometric data of the patient.
Passive therapy
With passive mechanotherapy, movements in the joints occur due to the smooth and gradual operation of the device’s levers. The therapy is aimed at developing movements and restoring joint function through dosed stretching of the ligaments and joint capsule. At the same time, the muscles relax. The effectiveness of passive exposure lies in the fact that the joint moves with an individually selected amplitude and speed. There is no active contraction of the periarticular muscles. The technique is recommended to be carried out during early rehabilitation.
How exactly does mechanotherapy help restore the body?
The therapeutic effect of mechanotherapy is:
- tonic effect;
- improving tissue trophism, blood and lymph circulation;
- formation of functional compensations;
- improving pulmonary ventilation and coronary blood supply;
- increasing proprioceptive sensitivity;
- normalization of the functions and integrity of the body.
Restoring the body with the help of mechanotherapy is one of the auxiliary means of rehabilitation and should be used in combination with other methods, such as the use of hygienic and therapeutic exercises, walking, and dieting.
Types of simulators
Modern mechanotherapeutic simulators, depending on their design, are designed to perform a number of tasks:
- Block. In block simulators, a cable is passed through the blocks, at the end of which a load is attached. To regulate the force, a change in the mass of the load is provided. Training can be carried out in a standing, sitting, or lying position. Mechanotherapy using block devices is carried out in order to improve mobility, strength and endurance, and strengthen weakened muscles.
- Pendulum. The exercises are performed thanks to the force of inertia that occurs when the pendulum mechanism oscillates during loads performed by the patient himself. Muscles are strengthened and joint mobility increases. The load is adjusted by changing the angle, weight of the load or the location of its attachment.
- Isokinetic. They are represented by electromechanical devices with the ability to regulate the speed of load execution and resistance force. The greater the force, the greater the resistance and load on the limb. Isokinetic exercise machines are used exclusively to increase strength.
- Combined or general strengthening mechanotherapeutic devices - roller, rowing machine, treadmill, exercise bike, etc. Exercises on them involve several muscle groups at the same time. Such devices are indispensable for compensating for insufficient physical activity.
Commented by orthopedic doctor Ph.D. Litvinenko Andrey Sergeevich:
In the rehabilitation of diseases of the joints and spine, active-passive mechanotherapy devices from Ormed have proven themselves to be excellent. The equipment is universal, computer controlled, allows you to individually configure all parameters, suitable for both adults and children. Thanks to the introduction of mechanotherapeutic simulators into complex treatment programs, we were able to double the rate of restoration of function of the knee and hip joints in degenerative diseases.
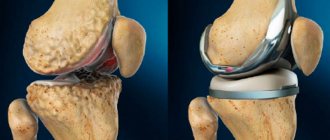
Total joint replacement
Hip endoprosthesis
Total arthroplasty, like many other types of joint replacement, must be accompanied by restoration of the work and functioning of soft tissues. Choosing the right and appropriate rehabilitation scheme helps solve many problems.
During the operation, the surgeon passes through the skin, musculoskeletal and capsular structures to reach the hip. Traumatic effects on soft tissue as a result of surgery can lead to complications. "By-products" of surgery include pain, stiffness, swelling, and possible thrombosis, affecting a variety of soft tissues in addition to bone.
In the postoperative period, many difficulties arise related to rehabilitation, the health of the patient and the cost of recovery for him. If these issues are not addressed, the effects of injury, inflammation, and immobility can inhibit the recovery of function in the injured limb.
Rehabilitation after joint replacement: what the patient may encounter
- Pain , the body's natural response to injury, can limit a person's functionality, especially if it is protective muscle pain. Active exercises begun immediately after surgery can be extremely painful, while slow, controlled passive movements help relieve pain through the pain gate control mechanism.
- Stiffness as a result of interconnected crossing of connective tissue fibers and adhesions can occur quite quickly in the postoperative period. This may result in functional limitations in range of motion when walking or other types of movement. It has been demonstrated that early rehabilitation after joint replacement, ACL reconstruction, fracture, etc. promotes the restoration of connective tissue due to the parallel alignment of collagen and elastin fibers.
- Edema , which is a product of inflammation and repair, poses a certain challenge for doctors and patients. When coupled with immobilization of the patient, edema tends to spread into the tissues and also limits muscle contraction and reduces blood flow.
- Finally, deep vein thrombosis is a serious danger for many patients after joint surgery, arthroplasty, ACL reconstruction, etc. Older patients are especially at risk. Due to vascular congestion, which is a consequence of immobility of the limb, deep vein thrombosis is a common manifestation following joint replacement. Its incidence ranges from 34% to 75% depending on the complexity of the operation.
Rehabilitation after endoprosthetics with the help of mechanotherapy helps pump blood and maintains blood circulation. By positively influencing the speed of blood flow, mechanotherapy also helps reduce the negative impact of limb immobility, which is the root cause of deep vein thrombosis.
Mechanotherapy or manual joint development?
In the modern world of highly effective medicine and patient care, the question of cost inevitably arises when deciding on postoperative rehabilitation techniques. Clinics reduce the length of a patient’s stay in the hospital after surgery, and return home is faster. At the same time, rehabilitation after joint replacement is an essential component of a good result of the operation as a whole. It must be ongoing and appropriate to the objectives of the various stages of recovery to avoid possible complications after surgery. Rehabilitation after joint replacement includes active development, passive development with the help of a rehabilitation therapist, mechanotherapy and physiotherapy.
Hip displacement is a serious complication that accompanies total joint arthroplasty and manifests itself in weakening of prosthetic components, weakening of supporting soft tissues, and/or hypertrophied hip movements in the directions of flexion, adduction, and internal rotation. If the caregiver/assistant is insufficiently competent or the manual range of motion techniques used after joint replacement are inconsistent (in active and/or passive modes), then the risk of displacement of joint components increases dramatically. When using a mechanical therapy device, early movements are consistently and carefully controlled. Since most mechanical therapy devices maintain the limb in a neutral position relative to the flexion-extension axis and limit the range of motion through which the joints can move, this technique, when used correctly, helps prevent complications. Rehabilitation after joint replacement can begin almost immediately after surgery.
What effects does the technique produce?
The maximum effect is observed when classes begin in the early rehabilitation period. Long-term use of the method is possible. Exercises on a device for robotic mechanotherapy of the upper limb, legs and spine can be performed for a long time for both therapeutic and preventive purposes.
Effects of the technique:
- strengthening muscle fibers;
- improving blood flow and lymph outflow;
- pain relief;
- improvement of synovial fluid synthesis;
- acceleration of regeneration of damaged tissues;
- increasing performance and endurance;
- stabilization of the condition of periarticular structures;
- restoration and improvement of joint mobility;
- acceleration of rehabilitation and recovery.
Therapeutic exercise and mechanical massage affect the entire body. Muscular activity improves the functioning of the central nervous system (eliminates neurological symptoms of diseases), normalizes the functioning of internal organs, and improves immunity.
Mechanotherapy devices for the hip joint
The Arthromot mechanotherapy device is used in the early stages of rehabilitation after joint replacement to increase the amplitude of leg flexion
As a rule, mechanotherapy devices can be used in the early stages after joint replacement surgery. The Arthromot or Kinetek mechanotherapy device moves the patient’s leg, while controlling all movements and keeping the patient’s leg aligned along the axis, without moving around the circumference or to the side. This avoids the risk of excessive movement and displacement of the joint. In addition, the design of the device avoids discomfort and possible irritation at the incision sites on the thigh.
See further rehabilitation program after knee replacement
Contraindications
- Joint contractures;
- Arthritis and arthrosis of the joints;
- Scoliosis of the spine;
- Posture defects (kyphosis, lordosis);
- Ankylosing spondylitis;
- Myalgia and myositis;
- Scar changes in soft tissues;
- Paresis and paralysis;
- Injuries of the spine and joints;
- Postoperative period;
- Prolonged bed rest;
- Restricted mobility in elderly patients;
- Long-term immobilization (after plaster casts, Ilizarov apparatus).
- Ankylosis (complete closure) of the joint;
- Severe joint deformities;
- Complete muscle atrophy;
- Thrombosis and varicose veins in advanced form;
- Increased body temperature, chills;
- Presence of tumors in the affected area;
- Some forms of cerebral palsy;
- Severe heart disease;
- Mental disorders;
- Alcohol intoxication;
- Pregnancy.
Mechanotherapy for curvature of the spine and poor posture helps stop the progression of the deformity and strengthen the muscle corset.
Patients with unhealed fractures are recommended to refrain from sessions on mechanotherapeutic devices. After the procedures, mild muscle pain is possible, since the muscles have not been stressed for a long time. Intense pain indicates incorrect dosage of exercises or non-compliance with implementation tactics.
Patient preparation
The effectiveness of the technique depends on the quality of preparation. It is aimed at the effectiveness of therapy and safety. Before mechanotherapy, it is recommended to carry out simple preparatory measures:
- exclusion of contraindications;
- refusal of heavy meals 1.5-2 hours before training;
- clarification with a doctor about the technique of performing exercises.
During sessions, medical professionals monitor how correctly the patient performs the exercises.
How is the procedure done?
After the preparatory measures, the patient is ready for the session. Stages of mechanotherapy.
- Examination of the patient.
- Determination of indications for therapy and volume of load.
- Placing the patient on a mechanotherapeutic device.
- Mode programming.
- Start the procedure.
- Doing exercises.
Depending on the type of simulators and diagnosis, the session duration ranges from 10 to 45 minutes. The time and number of repetitions are gradually increased. The number of sessions is at least 5, breaks between classes are 1-3 days. These indicators are individual for each patient.
Principles when practicing mechanotherapy.
- Individual training and strict dosing of loads.
- Regularity of classes.
- Maintaining the sequence of exercises.
- Alternating physical activity with short rest.
- Gradually increase the duration of the workout. Taking into account contraindications and the patient’s age group.
Mechanotherapy can get back on their feet even those patients who have experienced severe limitation of activity. Targeted and gradually increasing loads are an effective way of rehabilitation. The technique goes well with massage and physiotherapeutic procedures. Treatment must be carried out under the strict supervision of a doctor!
Author of the article:
Litvinenko Andrey Sergeevich
Orthopedist
Make an appointment
Recent publications by the author:
- Laser therapy
- Magnetotherapy
- Myostimulation
- Transcutaneous electrical nerve stimulation (TENS)
Modern methods of rehabilitation of children with cerebral palsy
The relevance of the issue of treatment and rehabilitation of children with cerebral palsy is beyond doubt. It is especially important at the present stage, when therapy evaluation should be carried out using evidence-based methods. Cerebral palsy (CP) is a group of stable disorders of motor development and postural maintenance leading to motor defects caused by non-progressive damage and/or an abnormality of the developing brain in the fetus or newborn child. Cerebral palsy develops, according to various sources, in 2–3.6 cases per 1000 live births and is the leading cause of childhood neurological disability in the world. Among premature babies, the incidence of cerebral palsy is 1%. In newborns weighing less than 1500 g, the prevalence of the disease increases to 5–15%, and with extremely low body weight – up to 25–30%. Multiple pregnancies increase the risk of developing cerebral palsy: the frequency for singleton pregnancies is 0.2%, for twins - 1.5%, for triplets - 8.0%, for quadruple pregnancies - 43%. In the Russian Federation, the prevalence of registered cases of cerebral palsy is 2.2–3.3 cases per 1000 newborns [1].
Optimal care for a patient involves a multidisciplinary approach from a team of medical, pedagogical and social specialists who pay attention to the needs of not only the patient himself, but also his family members involved in the daily rehabilitation and social adaptation of the patient. Being a dysfunctional condition, the disease requires continuous daily rehabilitation from the first days of the patient’s life, taking into account the following medical and social aspects of the task:
- movement, maintaining posture and motor activity of the child;
- communication;
- treatment of concomitant diseases;
- daily activity;
- baby care;
- quality of life of the patient and family members;
- motivational and emotional support.
In a child under 4 months (according to the classification of K. A. Semenova), the diagnosis is not always obvious. The presence of a burdened perinatal history and delayed psychomotor development of the child are indications for targeted observation of the child by a pediatrician, rehabilitation specialist, occupational therapist, psychologist, defectologist, mechanotherapist, hydro-rehabilitation specialist and neurologist. At the first stage of rehabilitation, the provision of assistance to newborns at risk of developing cerebral palsy begins in the maternity hospital and continues at the second stage - in specialized departments at children's hospitals and subsequently moves to the third stage - on an outpatient basis at children's clinics under the supervision of a pediatrician, neurologist and medical specialists ( orthopedist, ophthalmologist, etc.). The initial examination of the patient and further treatment can be carried out in a hospital setting, a day hospital or on an outpatient basis in a children's clinic, which is determined by the severity of the patient's general condition. An additional stage of rehabilitation treatment is the referral of patients to sanatorium institutions, as well as social rehabilitation centers. The length of continuous stay of such a child in a medical institution depends on the severity of motor disorders and concomitant pathology. It is important not only to conduct courses of comprehensive rehabilitation treatment in a medical institution, but also to follow recommendations regarding the level and nature of physical activity, and the use of technical means of rehabilitation at home. The key principles of providing assistance for this disease are its early onset, continuity and continuity of all stages of rehabilitation or a multidisciplinary approach.
After consulting a patient entering for rehabilitation, a multidisciplinary medical team makes a rehabilitation diagnosis (in the categories of the International Classification of Functioning or ICF), determines short-term and long-term rehabilitation goals, and draws up an individual rehabilitation plan. There is a constant increase in the number and improvement of existing traditional and alternative methods of treating patients with cerebral palsy, but the fundamental goal remains the same - timely compensation of functional disorders that have developed as a result of damage to the child’s brain, and minimization of secondary biomechanical deformations and social consequences of the disease. If it is impossible to have a pathogenetic effect on the cause of cerebral palsy, the task is to optimally adapt the child to the existing defect, based on the principles of plasticity of the nervous system.
At the present stage, surgical correction is one of the most effective methods of rehabilitation of children with cerebral palsy. The complexity of the problem lies in the fact that decision making requires an understanding of a number of factors influencing the prognosis and prospects of the patient. Surgical treatment methods are indicated only in cases of severe spasticity and apply only to resistant conditions of cerebral palsy, especially after all conservative methods have failed. Surgical treatment should always be carried out in a complex manner using a multidisciplinary approach, based on a thorough clinical and neurophysiological assessment. The purpose of this assessment is to determine the role of spasticity in the formation of pathological posture and movement patterns and the influence of this spasticity on the degree of impairment of vital activity criteria. It must be remembered that in some cases the patient can carry out his physical activity only if there is a certain level of spasticity and its cancellation can actually lead to a worsening of the condition. Therefore, at the stage of choosing treatment tactics, it is very important to distinguish between the so-called “functional” spasticity, which helps maintain a certain level of daily activity of the patient, and “pathological”, which is actually disabling. It is also important to separate muscle and joint contractures. When choosing a “suitable candidate”, it is necessary to very clearly define the goals for a particular patient that must be achieved during the upcoming operation. The goals of the upcoming surgical intervention may be to improve the quality of life and independence, improve limb function, and reduce the severity of orthopedic disorders.
Approaches to surgical treatment of spasticity in cerebral palsy can be divided into several groups depending on the level of impact, the specific task and the method of solving it [2]:
1. Neurosurgical treatment:
1.1. Destructive neurosurgical techniques:
a) stereotactic encephalotomy; b) longitudinal (longitudinal) myelotomy; c) posterior cervical rhizotomy; d) selective dorsal rhizotomy; e) neurotomy.
1.2. Functional neurosurgery:
a) stimulation of the cerebellum; b) spinal cord stimulation (cervical, lumbar).
2. Orthopedic surgical treatment:
2.1. By location of impact:
a) operations on bones and joints. b) operations on tendons. c) muscle surgery.
2.2. By method of influence:
a) compression-distraction techniques; b) bone intra-articular operations; c) osteoplastic surgery.
Overcoming spasticity and decreased muscle tone still remain the central goals of most rehabilitation techniques for cerebral palsy. At the same time, it should be understood that high muscle tone can play a certain supporting role when moving a patient with cerebral palsy; its decrease does not always lead to an improvement in motor function [3].
Therapeutic exercise (PT) is an extremely effective method that must be included in the rehabilitation of children with cerebral palsy [4]. The objectives of treatment from exercise therapy are:
- normalization of muscle tone;
- normalization of motor skills;
- increased joint mobility;
- increasing strength and power endurance of major muscle groups;
- optimization and prevention of muscle spasms.
Massage is a manual intervention on the skin and underlying formations of patients with cerebral palsy. The massage procedure is traditional and most prescribed in the structure of complex therapy. Massage solves the same therapeutic problems as exercise therapy; spasticity is at the head of these problems. Massage techniques have an impact either on the areas of the main lesion - the so-called trigger points, or on the body as a whole - a general relaxing massage, or on reflex-segmental areas - reflex, paravertebral massage. The dosage of massage for cerebral palsy deserves special attention. They are an order of magnitude higher than in other neurological diseases and amount to 5–7 massage units.
Methods of physical rehabilitation are traditionally represented by mechanotherapy, and in a number of medical centers and clinics - robotic hardware therapy using specialized simulators, including those based on the principle of biofeedback (BFB). The most effective devices today are the Locomat series devices - a robotic orthopedic simulator for restoring walking skills. The proposed device is used in different configurations, taking into account the characteristics of rehabilitated patients. The Armeo simulator is a robotic complex for functional therapy of the upper and lower extremities with biofeedback. One of the most effective mechanisms for diagnosing, monitoring and treating patients with cerebral palsy is a stabiloplatform, produced in different versions, which makes it possible not only to provide a therapeutic effect, but also to determine the patient’s condition in a given period of time, that is, to determine the quality and dynamics of the rehabilitation process. In the system of comprehensive rehabilitation treatment for children, verticalizers of various modifications are an important component. These simulators make it possible to create and impart the correct gradual vertical position of the patient in space. A breakthrough technique in the treatment of patients with cerebral palsy was the emergence of exoskeletons of various types. These simulators enable the patient to create and develop a complete sense of walking pattern with extremely low physiological capabilities. Separately, we consider the Motion Maker training system, which has shown high proven effectiveness. A domestic development that has found wide application in the complex rehabilitation of such patients is the use of the method of dynamic proprioceptive correction, carried out using specialized suits (Adele, Gravistat, Atlant), systems consisting of supporting elastic adjustable elements, with the help of which targeted posture correction and dosed load on the musculoskeletal system of patients are created in order to normalize proprioceptive afferentation.
Traditionally, in Russia, during the rehabilitation of patients with cerebral palsy, physiotherapeutic methods are widely used, including those based on natural factors: applications of mud, paraffin, fangoparaffin, ozokerite for antispastic purposes. Electrophysiological methods are also actively used - various types of electrical stimulation, electrophoresis with medicinal substances. The photochromotherapy technique, proposed for various significant reflexogenic zones, showed good results. Methods of influencing the brain (Tomatis and bioacoustic correction) are actively used with good therapeutic effect. Physiotherapeutic methods for treating children with cerebral palsy also include the method of hyperbaric oxygenation, which has proven itself in ataxic forms of the disease. To optimize mood, improve emotional state and prevent vitamin D deficiency conditions, children with cerebral palsy are prescribed heliotherapy using the “Artificial Sun” apparatus.
In cases where the speech and mental abilities of a patient with cerebral palsy are impaired to one degree or another, a specialist speech therapist-defectologist is involved in the complex of rehabilitation measures. Depending on the direction of the lesion (speech, mental, cognitive impairment), certain techniques are prescribed. Speech therapy correction involves pronouncing certain sounds, their combinations, syllables and words in a certain sequence. Various author’s gymnastics are also used, which make it possible to improve the condition of the maxillofacial apparatus. As additional assistance, the specialist is offered speech therapy massage of the face, tongue and lower jaw, which is carried out manually or using special probes. A defectologist conducts educational programs that improve the mental and logical state of a child with cerebral palsy.
To normalize the psycho-emotional status of families in which children with cerebral palsy live, in a comprehensive rehabilitation program, a specialist - clinical psychologist - solves the following tasks:
- assessment of the psychological status of the child with cerebral palsy and the family;
- in-depth assessment of the child’s cognitive functions (memory, attention);
- assessment of emotional state, diagnosis of anxiety, depression;
- Provides counseling and psychological assistance and correction to families and children.
The assessment is carried out using special questionnaires and scales, which make it possible to objectively assess these conditions and make appropriate corrections.
Methods with high evidence include alternative communication technologies and various options for play therapy (fairy tale therapy and other methods).
Occupational therapy is a new direction in rehabilitation. In modern medicine, an occupational therapist is always present at the level of a multidisciplinary team, especially when the motor abilities of patients in the structure of everyday skills are reduced or significantly impaired. These specialists help children find comfort in everyday activities. By education, an occupational therapist is a psychologist or specialist in adaptive physical education who has undergone appropriate training. Treatment goals for an occupational therapist include:
- assessment of stress on everyday activities;
- assessment of the patient’s activities at the everyday level;
- assessment of anxiety during activity limitation;
- restoration or development of activities that have been limited or impaired;
- assessment of opportunities for independent activity. Prevention of family overprotection;
- inclusion of the patient in self-care and mobility activities;
- examination of the living environment and its adaptation for the patient’s further activities;
- restoration of motor abilities in the domestic sphere;
- prevention of restrictions on everyday movements.
The main focus of classes with a social educator is teaching communication techniques and interaction with the environment. It is usually carried out individually over a long period of time. It is created on the basis of an individual social service program (IPSO). It is carried out in social rehabilitation centers for the disabled, city clinics or departments of medical rehabilitation centers and includes:
- working with specialists;
- creation of an educational environment in institutions of additional education;
- interaction with parents (educational work);
- diagnostics of professional orientation and preparation for training;
- working with the family of a sick child;
- research on family problems;
- social and pedagogical patronage of the family;
- social and pedagogical preparation for the rehabilitation process;
- working directly with the child;
- pedagogical and psychological diagnostics;
- development of individual rehabilitation programs;
- correctional and developmental work.
Orthopedic devices play a major role in the quality of life of children with cerebral palsy. These include specially manufactured insoles, orthopedic shoes and so-called lower leg orthoses. All of these devices help normalize the walking pattern or the ability to create an upright position, depending on the degree of disability of the child.
In addition to traditional methods of treating cerebral palsy, alternative rehabilitation programs are offered. Alternative methods of treatment and rehabilitation of patients include acupuncture and acupuncture, manual therapy, craniosacral techniques, canistherapy, hippotherapy and dolphin therapy, yoga, taijiquan, methods of Chinese traditional medicine, however, according to the criteria of evidence-based medicine, the effectiveness and safety of these methods has not currently been assessed. Also, with insufficient evidence base in the treatment of cerebral palsy, kinesio taping is proposed. A method that makes it possible to compensate for tone disorders and optimize motor skills.
An important and promising invention in modern hydrorehabilitation technologies for the treatment of concomitant cerebral palsy syndromes is the underwater traction method. The design of the water traction apparatus is a bath filled with water, with a special mechanism installed in it, into which the patient is immersed. In this case, the patient's lower limbs are fixed. Traction is applied to the shoulder girdle using a special device, which has electronic adjustment of traction. Traction is carried out using a specially developed technique, taking into account the disease and individual characteristics of the patients. The patient is brought to the device by a special platform, which creates immobility in a horizontal position. The underwater traction method has a therapeutic effect on chest deformities, postural disorders of varying degrees and pain syndromes caused by compression, which is often found in patients with cerebral palsy. The mechanism of action of water traction is aimed at reducing compression and traction of the spinal column, and with it the chest. Underwater traction has both a therapeutic and preventive effect on diseases of the spine and on the condition of the patient with cerebral palsy in general. The underwater traction method provides for the possibility of isolated traction of specified parts of the spinal column (any part of the spine can be affected). The procedure itself does not cause pain or negative sensations. Contraindications to underwater traction may be instability of various parts of the spine, mobility in the vertebrae, connective tissue dysplasia (“stretched” ligaments). Also, water traction is not prescribed if there are general contraindications for rehabilitation. The course of treatment using the underwater traction method averages 15–18 procedures every other day as part of complex therapy for children with cerebral palsy. It is recommended to conduct at least 3 courses throughout the year. Methodological features of the procedure include the strength and duration of traction in kilograms, determined individually. It is also necessary to individually determine the tempo (speed) of traction.
In the complex rehabilitation of children with cerebral palsy who have motor impairments, a separate area of treatment is the use of water at a temperature of 36–38 °C in the pool along with special exercises. These water exercises, or hydrokinesitherapy, help to significantly increase joint mobility and muscle relaxation, which leads to the normalization of motor abilities in patients. Exercises are carried out in water by an instructor, often in passive mode along with special movements and slides on the surface of the water. The activity may involve diving and snorkeling. These movements are performed at different speeds in different planes and directions according to a strictly defined technique. At the beginning of a course of rehabilitation treatment, it is necessary to test a patient with cerebral palsy for tolerance to physical activity and, based on the test results, make the correct dosage of exercises.
An important point in the prognosis of patients with cerebral palsy is the possibility of maintaining motor skills throughout life and the actual duration of life itself. The mortality rate among patients with cerebral palsy is directly dependent on the degree of motor deficit and concomitant diseases. Another predictor of premature death is decreased intelligence and inability to self-care. Thus, it was shown that in European countries, patients with cerebral palsy and an IQ of less than 20 in half of the cases did not reach the age of 18 years, while with an IQ of more than 35, 92% of patients with cerebral palsy lived more than 20 years. As for the prognosis of motor abilities, it is not so optimistic. Unfortunately, it has been proven [5] that in adolescence and adulthood, motor function and walking deteriorate and only half (!) of children with level III motor functions on the GMFCS (Global Motor Function Classification System) scale continue to walk with aids when they become adults. .
Level V are bedridden patients and they reach their maximum motor development by 3 years of age. For children of levels IV–V, rehabilitation should be carried out according to “palliative” principles.
In general, the quality of life and prognosis of social adaptation of patients with cerebral palsy largely depend on the timely provision of medical, educational and social assistance to the child and his family. Social deprivation and lack of access to comprehensive care can have a negative impact on the development of a child with cerebral palsy, perhaps even more significant than the initial structural damage to the brain.
Literature
- Federal clinical guidelines for the provision of medical care to children with cerebral palsy. https://minzdrav.gov-murman.ru/documents/poryadki-okazaniya-meditsinskoy-pomoshchi/_kr_dcp.pdf.
- Shalkevich L.V., Zaretsky S.V. Surgical methods of treating spasticity in children with cerebral palsy: basic principles, indications, effectiveness // Medical panorama. 2005, No. 11.
- Rosenbaum PL, Dan B. The continuing evolution of “Cerebral Palsy” // Annals of Physical and Rehabilitation Medicine. 2021, 24. S1877–0657(19)30152–6.
- Nemkova S. A. Cerebral palsy: early diagnosis and rehabilitation treatment // Attending Physician. 2007, no. 5.
- Rosenbaum PL, Livingston MH, Palisano RJ, Galuppi BE, Russell DJ Quality of life and health-related quality of life of adolescents with cerebral palsy // Developmental Medicine & Child Neurology. 2007, Jul; 49(7):516–521.
L. B. Kuranova*, 1, Candidate of Medical Sciences B. I. Kherodinov**, Candidate of Medical Sciences
* Federal State Budgetary Educational Institution of Higher Education St. Petersburg State Pediatric Medical University of the Ministry of Health of Russia, St. Petersburg ** Federal State Budgetary Educational Institution of Higher Education Northwestern State Medical University named after. I. I. Mechnikov Ministry of Health of Russia, St. Petersburg
1 Contact information
DOI: 10.26295/OS.2019.11.39.007
Modern methods of rehabilitation of children with cerebral palsy / L. B. Kuranova, B. I. Kherodinov For citation: Attending physician No. 12/2019; Page numbers in the issue: 45-48 Tags: children, psychomotor development delay, motor activity
Our doctors
- LITVINENKO Andrey Sergeevich
Traumatologist orthopedist Sports medicine doctor Experience: 19 yearsSign up
- SKRYPOVA Irina Viktorovna
Physiotherapist rehabilitator Experience: 20 yearsSign up
- MOISEENKO Alexey Yurievich
Traumatologist orthopedist Sports medicine doctor Experience: 17 yearsSign up
- KHOLIKOV Timur Vyacheslavovich
Traumatologist orthopedist Sports medicine doctor Experience: 19 yearsSign up