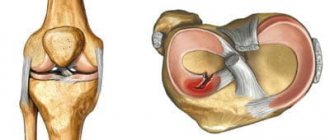
Structure of the meniscus of the knee joint
The meniscus is a cartilage-like formation inside the knee joint that performs a shock-absorbing and protective function. It has a crescent shape and is located between the articular surfaces. There are two of them in each knee, namely:
- Lateral (also known as external) – is less likely to be injured, but is more mobile.
- Medial (otherwise called internal) - most susceptible to injury, less mobile compared to the external.
The structure of the knee joint. Internal and external meniscus of the knee.
The strength and elasticity of this cartilage layer is provided by collagen fibers located radially. Given the crescent shape, each of them has two horns: anterior and posterior. The inner surface has a worse blood supply than the outer surface, facing the joint capsule. This affects the healing processes at different locations and treatment tactics, respectively.
Severity of rupture
When determining therapeutic tactics, the traumatologist must take into account the type of injury and its severity. Minor injury to the meniscus often does not require surgical intervention, but when it is fragmented or displaced fragments, surgery is necessary. There are 3 degrees of severity of rupture of the cartilage lining of the knee:
- degree of severity. Clinically, the injury is manifested by moderate pain, mild swelling in the knee area;
- degree of severity. The leading symptoms of damage are severe pain, the severity of which gradually decreases, swelling, hematoma;
- degree of severity. A rupture is characterized by acute pain, extensive swelling, hematoma, and inability to put weight on the foot.
A rupture of any severity requires seeking medical help. Due to improper fusion of cartilage tissue, the knee joint will not be able to fully function.
Types of meniscal tears
Types of meniscal tears of the knee joint.
The meniscus is damaged both in isolation and in combination with other anatomical formations. When exposed to an external force, the rupture is called traumatic. It is usually found in athletes. If changes occur due to arthrosis, this is a degenerative damage that is more common in people of the older age group. Moreover, both of these options are often multiple, affecting articular cartilage. They are, one way or another, interconnected and one does not exclude the other or is its consequence.
A distinction is made between complete and partial rupture. In the first case, free fragments become mobile and can cause blocking (“jamming”), namely the occurrence of impingement syndrome. A sharp immobilization occurs, which can only be eliminated by specialists and mainly by surgical means. If the part where there is active blood circulation is damaged, hemarthrosis is most likely - the accumulation of blood inside the joint. It manifests itself externally by a rapid increase in swelling.
Possible causes of pathology
The cause of a meniscus tear can be careless movement, prolonged stay in an uncomfortable position, or other high load on the cartilage pad.
At a young age, a meniscus tear is usually provoked by professional and amateur sports - team sports (volleyball, basketball), badminton, running, gymnastics, wrestling - because the cartilage plate of the knee is not designed for such loads. Professional athletes can withstand them only by strengthening the muscular-ligamentous apparatus. But when the load is decompensated (for example, an unsuccessful eversion), it injures the meniscus of both a trained and an ordinary person with equal effect.
The following factors contribute to a tear of the knee meniscus:
- chronic or repeated traumatization of the meniscus or other parts of the joint architecture - for example, when performing heavy household and professional duties (loaders, masons, dancers, farmers);
- sports and sports injuries;
- habit of squatting for a long time;
- age-related changes in joints;
- chronic diseases - systemic and joints (rheumatism, arthritis, gout, intoxication of the body, autoimmune diseases);
- excess weight.
Traumatic meniscus tears usually occur during so-called “twist” movements—rotational movements of the legs with a load on the knee. It can be caused by a sharp movement of the knee inward or outward (twisting the leg), a deep squat (especially with a barbell or other load), a blow to the knee, or displacement when lifting weights. In old age, it is enough to just get up from a chair or squat and rotate your leg in the joint.
The victim of such unfortunate accidents is usually the medial (inner) meniscus of the joint.
Among the traumatic causes of meniscal tears, the leading ones are:
- jumping from heights;
- an unsuccessful fall to your knees;
- spinning on one leg;
- joint hypermobility;
- failure to comply with safety precautions when exercising in the gym or performing eversion exercises;
- running on rough terrain (or on a path with natural uneven ground);
- dislocations and subluxations of the knee joint.
Sports injuries are the most common cause of knee meniscus tears.
First aid for meniscus injury
When a meniscus ruptures, a sharp pain occurs in the first minutes, which intensifies when the leg is extended.
If pain occurs as a result of an injury, care must be taken to ensure that the victim gets to a medical facility as soon as possible. The injured leg must be immobilized. To avoid bending during transportation, it is better to apply a splint or splint. It is strictly not recommended to eliminate the blockade, if it occurs, on your own. In order to alleviate the condition and avoid the increase in swelling, cold is applied to the knee, for example, an ice pack. Aerosol coolers, used more often among athletes, are optimal. As a last resort, you can offer the victim a non-steroidal anti-inflammatory drug. The sooner the patient gets to the clinic in compliance with all transportation rules, the less complications can be expected.
Diagnostics
By the time of consultation with a specialist, as a rule, extensive swelling has already formed in the injured area, and the pain syndrome is reduced due to the use of painkillers. Anamnesis data, as well as special functional tests, allow the doctor to conduct a differential diagnosis. They are simple, relatively painful, but help clarify the picture of the disease. Tests help determine the presence and location of pathology. The doctor decides which ones to use.
The most common of them include:
- Baykov's method. The knee is bent at a right angle, after which the joint space is palpated, while simultaneously extending the leg. The occurrence of sharp pain symptoms confirms the presence of damage.
- Shteiman's sign. The knee joint is bent 90 degrees, then the shin is rotated. If the pain increases with inward rotation, it means the medial meniscus is damaged, and with outward rotation, the lateral meniscus is damaged.
- Chaklin test. There are two types of such testing. Firstly, the presence of a rupture is indicated by a crunching sound when flexing and extending, and as if “rolling” the lower leg over an obstacle. In the second test, the patient raises his straight leg, and the doctor in this position palpates it for muscle atrophy in the thigh area.
- Polyakov's symptom. He lifts the healthy leg up, while trying to raise the pelvis and lean his elbow on the heel of the injured one. There is pain at the rupture site.
- Landau test. It consists of sitting in a “Turkish” position. Such an attempt in the presence of deformity will result in pain in the area of the rupture.
- Mac Murray's method. The patient, lying on his back, bends his leg and then rotates his knee. Painful sensations will appear, and a click will also be heard.
- Perelman's symptom. It has two varieties - climbing stairs or putting on shoes without hands. In both cases, pain appears, localized in the area of injury.
In addition, X-ray diagnostics (x-ray or computed tomography) and MRI (magnetic resonance imaging) are performed. They give a clear picture of the location and degree of deformation. Arthroscopy is also used for diagnosis. It also allows you to immediately perform the necessary surgical treatment.
Radiation research methods.
In all patients with clear clinical symptoms, radiographic examination should be performed in two projections - anteroposterior and lateral.
Old injuries (2-3 months) are accompanied by changes in the edge of the ipsilateral tibial plateau with the deposition of periosteal deposits or the formation of osteophytes (Rauber's sign), which can grow up or down from the edge of the eminence. It is also possible for the cortex to thicken without the formation of osteophytes. Radiographic signs of meniscal cysts in the anteroposterior projection are depressions of the medial and lateral plateau of the tibia with pointed and sclerotic edges.
Magnetic resonance imaging is a highly informative method for assessing meniscus damage.
knee joint. According to MRI, there are four degrees of changes in the meniscus (classification according to Stoller).
- ✅ Grade 0 is a normal meniscus.
- ✅ Degree I is the appearance of a focal signal of increased intensity in the thickness of the meniscus (not reaching the surface of the meniscus).
- ✅ Degree II - the appearance of a linear signal of increased intensity in the thickness of the meniscus (not reaching the surface of the meniscus).
- ✅ Degree III - a signal of increased intensity that reaches the surface of the meniscus. Only grade III changes are considered a true meniscus tear. It is possible to distinguish grade III a, when the tear extends to one edge of the articular surface of the meniscus, and grade III b, when the tear extends to both edges of the meniscus.
The accuracy of MRI in diagnosing a meniscus tear is approximately 90-95%, especially if a signal of increased intensity is recorded twice in a row (i.e., on two adjacent sections), covering the surface of the meniscus. To diagnose a tear, you can also focus on the shape of the meniscus. Typically, on sagittal plane images, the meniscus has a butterfly shape.
Any other shape could be a sign of a rupture. A sign of rupture is also the symptom of “double posterior cruciate ligament” (or “third cruciate ligament”), when, as a result of displacement, the meniscus ends up in the intercondylar fossa of the femur and is adjacent to the posterior cruciate ligament.
A meniscus tear can be detected by MRI even in the absence of complaints from the patient, and the frequency of such cases increases with age. This shows how important it is to take into account all clinical and radiological data during the examination.
Conservative therapy
Shock wave therapy is an effective method of conservative treatment for minor disorders.
Conservative treatment is aimed at reducing inflammation and accelerating healing when the rupture is incomplete and surgery can be avoided. If there is pathological fluid in the joint - blood due to vascular damage or effusion due to inflammation - it is removed using a puncture. The limb is partially immobilized with an orthosis in order to avoid excessive stress when moving. A course of non-steroidal anti-inflammatory drugs is prescribed. Sometimes intra-articular corticosteroids are required. Injections of hyaluronate, platelet-rich plasma, help cartilage quickly recover. For this purpose, oral chondroprotectors are prescribed. You need to start developing the joint under the supervision of a rehabilitation specialist. Rehabilitation is aimed at restoring all functions and strengthening the thigh muscles. In addition to kinesiotherapy, mechanotherapy and massage are used. Physiotherapeutic methods (UHF, electrophoresis, electromyostimulation) accelerate the healing process.
Meniscus arthroscopy
At the SportClinic, meniscal arthroscopy is performed by the best traumatologist-surgeons in Russia.
Surgical treatment of meniscal tears of the knee joint is carried out using arthroscopy. This is a minimally invasive and effective method for diagnosing and treating such pathologies today. It is low-traumatic in relation to surrounding tissues. The high resolution of the arthroscope camera provides a detailed image, which is displayed in an enlarged format on the screen, which ensures the accuracy of the examination during arthroscopy. Immediately after diagnosis, all surgical procedures are performed. In case of a rupture, this means resection or removal of the meniscus, and in case of minor damage, it can be sutured.
Arthroscopic suturing of the meniscus
By connecting the torn edges, mainly from a fresh injury, it is possible to achieve their fusion and restore the integrity of the damaged structure. This occurs most successfully after a rupture in the part that faces the joint capsule and is better supplied with blood. During arthroscopy, special clamps are introduced into the joint, which the doctor places on the torn edges, having previously connected them. This method is especially relevant for athletes and people who regularly expose their knee to fairly heavy loads. The effectiveness of the technique is high, success is achieved in 90%. Arthroscopy is a low-traumatic and easily tolerated operation. If you follow the recommendations of specialists during the rehabilitation period, it is possible to restore your previous shape in the shortest possible time.
Meniscus resection
If reconstruction is not possible after a rupture, then resection is performed through arthroscopy - damaged and torn elements are removed. The remaining healthy tissue is preserved and the surface and edges are sanded for best function. After which, the leg returns to active movements without significant consequences. As a rule, if most of the meniscus was preserved, then the functions of the knee do not suffer in any way in the future; after several weeks of a rehabilitation course, the patient is allowed to participate in sports training.
Complete arthroscopic removal
Complete removal or meniscectomy is a common operation and is also performed using an arthroscopic technique. The meniscus, previously affected by arthrosis, literally falls into pieces under traumatic influence. Sometimes a complex mechanism of injury leads to its loss. The decision to remove is usually made during arthroscopy. The limb after such operations functions stably, provided proper recovery and moderate loads. Further, it is recommended to be constantly monitored by a doctor to prevent the development of arthrosis.
Treatment process
Traditionally, treatment methods are selected by a traumatologist, taking into account all the data obtained during the diagnosis. In most cases, patients require a plaster cast after puncture of the joint. In the first days after surgery, it is very important to ensure maximum rest for the injured leg, after which painkillers will be administered to help relieve pain.
Removing the cast does not guarantee complete recovery. Patients are prescribed chondroprotectors, a complex of physical therapy, as well as all kinds of anti-inflammatory drugs for both internal and external use.
In particularly difficult situations, surgical intervention is resorted to. In this case, the meniscus is sutured or its torn parts are removed. In the latter case, complete removal of the meniscus is carried out in the presence of degeneration in the cartilage tissue, as well as in case of serious injury, which is accompanied by a large tear.
Rehabilitation after arthroscopy
After arthroscopy, the rehabilitation period proceeds quite easily and quickly, in contrast to open access surgery, and no large scars are left on the patient’s body. A rehabilitation plan is developed individually by a rehabilitologist, taking into account the characteristics of the pathology, the treatment performed, age characteristics, concomitant pathologies, and his lifestyle. Following all recommendations is the key to a successful and quick recovery.
The main methods include:
- Kinesiotherapy. Otherwise, this method of rehabilitation can be called physical therapy. This is a set of exercises aimed at strengthening the muscles in the desired area and developing the motor activity of the joint.
- Manual therapy. Relieves spasms, stimulates atrophied muscles to activity, and promotes better innervation.
- Mechanotherapy. Exercises on machines that strengthen the muscle frame in the required area.
In addition, kinesiotaping (application of special patches that regulate the load on certain muscles), physiotherapy, including: ultrasound, myostimulation, shock wave therapy, magnetic therapy and others, are used. As a rule, recovery takes about one and a half months, after which patients return to their normal lives, and athletes can begin training.
Advantages of arthroscopic surgery
Minimally invasive endoscopic technology is considered the gold standard for the treatment of injuries to the knee and other joints. It has multifaceted capabilities, allowing for diagnosis and surgical intervention of almost any complexity. Main advantages:
- low blood loss;
- low tissue trauma;
- no rough postoperative scars remain;
- minimal risk of complications;
- quick recovery period with little pain.
During endoscopic surgery, it is possible to perform partial or complete removal of cartilage plates, apply sutures, and fix the meniscus.
The duration of the operation is on average 1-1.5 hours, which depends on the complexity of the damage and the scope of treatment. After processing the surgical field, the surgeon makes two punctures into which an arthroscope with a fixed camera is inserted. From it, an image of the joint cavity is displayed on the monitor screen. Through another puncture, manipulators are inserted - instruments for all actions during the operation. To improve visualization, a small amount of saline is placed into the cavity.
Upon reaching the meniscus, the doctor assesses the condition of the tissues and, taking into account the damage, decides on further actions - suturing, tissue resection, removal of the meniscus. After all manipulations, the joint cavity is washed with antiseptic solutions, the instruments are removed, sutures are applied to the wound and covered with a sterile bandage.