Joint damage has increased significantly in recent years, as has the number of young people experiencing joint damage problems.
The most injured joint is traditionally the knee joint. A torn meniscus and torn anterior cruciate ligament are the most common injuries.
The main stabilizers of the knee joint are the anterior, posterior cruciate ligaments, external and internal collateral ligaments. The anterior cruciate ligament keeps the tibia from moving too far forward. A torn anterior cruciate ligament is a less common injury than a torn meniscus, but is not uncommon among people involved in sports.
Knee-joint
Knee joint
The knee joint is a complex part of the musculoskeletal system. The anterior and posterior cruciate ligaments are strong bands of connective tissue. They are necessary to strengthen the joint and stabilize it.
Their damage occurs due to rotation (rotation) of the thigh with the lower leg fixed in one position, as well as due to direct mechanical impact in the form of an impact. This often occurs in people actively involved in sports (people involved in basketball, gymnastics). ACL rupture is also possible in everyday life, in particular when twisting your leg or falling on your knee.
S80—S89 Knee and lower leg injuries
S80 Superficial injury of the leg
- S80.0
Contusion of the knee joint - S80.1
Contusion of other specified and unspecified part of the leg - S80.7
Multiple superficial injuries of the leg - S80.8
Other superficial injuries of the leg - S80.9
Superficial injury of the leg, unspecified
S81 Open wound of the leg
- S81.0
Open wound of the knee joint - S81.7
Multiple open wounds of the leg - S81.8
Open wound of other parts of the leg - S81.9
Open wound of the leg, unspecified location
S82 Fracture of lower leg bones, including ankle joint
- S82.00
Patella fracture, closed - S82.01
Open patella fracture - S82.10
Fracture of the proximal tibia, closed - S82.11
Open fracture of the proximal tibia - S82.20
Fracture of the body [diaphysis] of the tibia, closed - S82.21
Open fracture of the body [diaphysis] of the tibia - S82.30
Fracture of the distal tibia, closed - S82.31
Open fracture of the distal tibia - S82.40
Closed fracture of the fibula - S82.41
Open fracture of the fibula - S82.50
Fracture of the medial malleolus, closed - S82.51
Open medial ankle fracture - S82.60
Fracture of the external [lateral] malleolus, closed - S82.61
Open fracture of the lateral malleolus - S82.70
Multiple closed fractures of the tibia - S82.71
Multiple open fractures of the tibia - S82.80
Fractures of other parts of the leg, closed - S82.81
Fractures of other parts of the leg, open - S82.90
Fracture of unspecified part of the tibia, closed - S82.91
Fracture of unspecified part of the tibia, open
S83 Dislocation, sprain and overstrain of the capsular-ligamentous apparatus of the knee joint
- S83.0
Patella dislocation - S83.1
Dislocation of the knee joint - S83.2
Fresh meniscus tear - S83.3
Fresh rupture of articular cartilage of the knee joint - S83.4
Sprain, rupture and strain of the external internal collateral ligament - S83.5
Sprain, rupture and strain of the anterior posterior cruciate ligament of the knee joint - S83.6
Sprain, rupture and overstrain of other and unspecified elements of the knee joint - S83.7
Injury to multiple structures of the knee joint
S84 Nerve injury at calf level
- S84.0
Injury to the tibial nerve at the level of the leg - S84.1
Injury of the peroneal nerve at the level of the leg - S84.2
Injury of cutaneous sensory nerve at the level of the leg - S84.7
Injury of several nerves at the level of the leg - S84.8
Injury to other nerves at the level of the leg - S84.9
Injury of unspecified nerve at the level of the leg
S85 Injury to blood vessels at the level of the leg
- S85.0
Popliteal artery injury - S85.1
Injury of tibial anterior posterior artery - S85.2
Injury of the peroneal artery - S85.3
Injury of the great saphenous vein at the level of the leg - S85.4
Injury of the small saphenous vein at the level of the leg - S85.5
Popliteal vein injury - S85.7
Injury of several blood vessels at the level of the leg - S85.8
Injury to other blood vessels at the level of the leg - S85.9
Injury of unspecified blood vessel at the level of the leg
S86 Injury to muscle and tendon at shin level
- S86.0
Injury of the calcaneal [Achilles] tendon - S86.1
Injury to another muscle and tendon of the posterior muscle group at the level of the lower leg - S86.2
Injury to the muscle and tendon of the anterior muscle group at the level of the lower leg - S86.3
Injury to the muscle and tendon of the peroneal muscle group at the level of the lower leg - S86.7
Injury of several muscles and tendons at the level of the leg - S86.8
Injury to other muscles and tendons at the level of the leg - S86.9
Injury to unspecified muscles and tendons at the level of the leg
S87 Crushed leg
- S87.0
Knee crush injury - S87.8
Crushing of another and unspecified part of the leg
S88 Traumatic amputation of the lower leg
- S88.0
Traumatic amputation at the level of the knee joint - S88.1
Traumatic amputation between the knee and ankle joints - S88.9
Traumatic amputation of lower leg at unspecified level
S89 Other and unspecified injuries of the leg
- S89.7
Multiple leg injuries - S89.8
Other specified injuries of the leg - S89.9
Unspecified lower leg injury
Classification
Depending on the degree of damage, there are several degrees of injury severity:
- Incomplete (partial) rupture, in which partial damage to the connective tissue fibers of the ligament occurs without disturbing the overall anatomical structure.
- Moderate injury, in which the number of damaged fibers is greater. This results in a slight increase in the length of the cruciate ligament with partial loss of knee stability.
- A complete break with a violation of integrity. At the same time, the functions of the knee deteriorate significantly, in particular the stability of the joint decreases.
Determining the severity of the rupture during an objective diagnosis of such an injury as a rupture of the cruciate ligament of the knee, treatment allows you to select the most effective one.
Trauma with ACL damage
Trauma with ACL damage
- Pain sensations developing inside the joint and in the area of its anterior surface. They are usually high intensity and appear immediately after injury.
- Increased severity of pain during loading of the knee.
- Impaired functioning of the knee joint, which is manifested by a limitation in the range of passive and active movements in it.
- The appearance of pathological mobility of the knee joint with a complete rupture.
The severity of the symptoms depends on the severity of the damage, as well as the individual characteristics of the human body.
Causes
The main causes of knee ligament damage are:
- simultaneous flexion of the knee joint, rotation of the shin outward and abduction to the side (for an injury to occur, the movement must be quite sharp);
- flexion, abduction and internal rotation of the lower leg;
- excessive extension of the knee joint;
- blow to the knee joint.
Symptoms of knee ligament damage:
- pain in the knee; when trying to move the knee, the pain intensifies;
- impaired joint mobility;
- constant tension in the muscles of the thigh and lower leg;
- swelling in the area of the knee joint, its increase in size;
- After an injury, hemorrhage forms under the skin.
An injury during which the ligaments of the knee joint are damaged is usually accompanied by hemarthrosis, an accumulation of blood in the joint cavity.
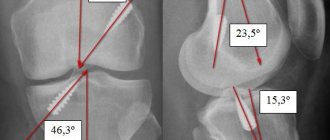
Diagnostics
Determining the location and severity of anterior cruciate ligament injury in modern medical clinics is carried out using various diagnostic techniques. These include:
- Radiography and fluoroscopy.
- Arthroscopy.
- Ultrasound.
- CT or MRI.
In clinics where there are technical capabilities for this, arthroscopy is used. It is a diagnostic method. Its principle is to introduce an optical device equipped with a camera and a light source into the joint cavity. Using a manipulator, a medical specialist can perform plastic surgery of joint structures.
Causes of anterior cruciate ligament rupture
A rupture of the anterior cruciate ligament can occur at the moment of a sudden stop with rotation of the whole body when the leg is fixed. This puts a huge load on the knee joint. A strong blow to the leg can also cause a rupture. After injury, patients complain of instability of the knee joint. In such cases, there is a feeling that the thigh is moving relative to the lower leg. Many people tend to mistake this for a knee dislocation, however, a dislocation is a much more serious injury that is not common. In order for the tibia to dislocate relative to the femur, all ligaments must be torn. This type of injury can occur in an accident or being hit by a very heavy object.
Such cases in our practice occur no more than 2-5 times a year, or even less often. In addition to the anterior cruciate ligament, ruptures of the internal or external collateral ligaments are also possible. In order to determine which ligament is damaged, a series of clinical tests are done to identify damage to the ligamentous apparatus. If there are doubts, it is possible to conduct additional studies, for example, magnetic resonance imaging (MRI), which shows the condition of the soft tissue structures of the joint, ligaments, and articular cartilage. In any case, an X-ray examination of the knee joint is performed. Immediately after an injury, treatment consists of reducing swelling and relieving pain. For this purpose, physiotherapeutic treatment and anti-inflammatory therapy are used. Once swelling has subsided, treatment is aimed at restoring range of motion and returning to normal levels of activity.
treatment without surgery
treatment without surgery
If the cruciate ligament is slightly damaged, treatment without surgery is possible. It includes conservative measures, the duration of which depends on the severity of the injury.
Typically, medications (non-steroidal analgesics, vitamins) and physiotherapy (electrophoresis with medications, mud therapy) are used.
For the entire period of treatment, it is imperative to ensure functional rest for the knee joint.
Rehabilitation after cruciate ligament surgery
Proper rehabilitation after cruciate ligament surgery is important for the patient’s complete recovery. A prerequisite for achieving success is the use of a complex of restorative measures (physical therapy, massage, physiotherapy, use of orthopedic devices), early exercise (in the first days after reconstruction) and a gradual increase in the load on the injured limb.
For athletes, rehabilitation after cruciate ligament surgery is carried out in 5 stages:
- From 1 to 4 weeks, measures are taken to relieve swelling and reduce pain, and learn to move without support.
- From weeks 5 to 10, the joint balance is improved, the leg muscles are strengthened, and the full range of motion is restored.
- From 11 to 16 weeks they work on increasing endurance and preparing for a return to normal activity.
- From 17 to 24 weeks, coordination of movements is improved.
- From 25 to 28 weeks - they restore special motor skills, move on to sports training and the usual rhythm of life.
For people who prefer a moderate level of physical activity, the rehabilitation period can be reduced to 20-24 weeks, provided they are careful when walking.
Surgery
If there is a pronounced rupture of the cruciate ligament, treatment must be carried out using surgical methods. Based on the severity of the knee injury and the location of the damage, several techniques can be used:
- An open access operation involves a wide layer-by-layer dissection of all tissues surrounding the knee joint, and then plastic surgery of the damaged ligaments.
- Arthroscopy is a low-traumatic technique in which manipulators and an arthroscope are inserted into the joint cavity through small incisions.
The choice of surgical treatment method is determined by the severity of the injury, as well as the capabilities of the clinic. In modern medical institutions, arthroscopy is predominantly used.
Treatment of anterior cruciate ligament rupture
Surgical treatment of anterior cruciate ligament injuries is now carried out arthroscopically rather than openly. Arthroscopy allows intervention into the joint in a more gentle way, through several punctures. Special optics are introduced into the joint area, which transmits on the screen everything that happens in the joint during the operation. To perform ligament plastic surgery, a graft is required, which is done using small incisions. However, these are not significant incisions and they heal much faster. The graft can be part of the patellar ligament or the tendon of the semitendinosus and gracilis muscles of the thigh. The graft is used to reconstruct the ligament.
Rehabilitation includes several stages. At the first stage, swelling and pain are relieved, joint movement is restored, and physical exercises are performed in combination with other methods of conservative treatment. At the second stage, the patient continues to restore the mobility of the joint, increases the number of movements, and strives to restore the stability of the joint when walking by strengthening the 4-headed thigh muscles. At the third stage, the load increases, endurance is trained and the ability to move for a long time without muscle pain, and the opportunity to run appears. Finally, in the fourth stage, the preoperative level of activity is achieved.
After ligament plastic surgery, complete recovery for team sports occurs under favorable conditions within 6-8 months from the date of surgery. After this period, you can return to your usual activities, including professional sports. Household loads and return to work are possible within 3-5 weeks. After this period, the patient can walk normally without limping.