Dystrophic changes
Degenerative changes are anatomical damage to an organ resulting from injury, atypical joint structure or disease. Degeneration of the meniscus is most often the result of injury, sometimes not even obvious: one unsuccessful rotation of the tibia can cause damage to the cartilage disc, which is accompanied by severe pain.
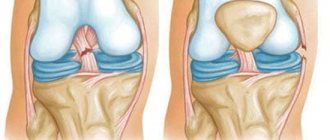
Most often, due to the anatomical structure, the medial meniscus undergoes degeneration. If the outer cartilage, which cushions the movement of the knee joint, does not have rigid fixation and moves to any side if necessary, then the medial one is rigidly fixed in the joint, and its horns are in close proximity to the condyles. One sharp turn of the shin - and the meniscus does not have time to escape from the displaced process of the bone, the result is its damage or rupture.
- separation from the attachment point;
- rupture of the horns and body of the meniscus;
- excessive mobility as a result of rupture of the intermeniscal ligaments;
- cyst - the formation of cavities filled with fluid inside the cartilage;
- meniscopathies are dystrophic changes that develop under the influence of minor injuries, as well as as a complication of gout, osteoarthritis, rheumatism, tuberculosis and a number of other diseases.
Dystrophic changes in the anterior cruciate ligament of the knee joint in most cases are the result of chronic microtraumas of the corresponding structures, which progress against the background of a number of unfavorable circumstances, in the form of professional sports, impact physical activity on the lower extremities, and so on.
At the same time, for a long period of time, the symptoms of this type of pathology may not appear at all or have vague signs.
Signs may be in the form of slight pain in the knee, intensifying after loading it, slight swelling at the joint, deterioration of its extension or flexion function, etc.
There are several types of dystrophic changes in the cruciate ligaments of the knee. In particular, these include mucoid degeneration, tendinitis, ligamentitis and intraligamentous damage.
By the term mucoid degeneration of the anterior cruciate ligament, modern doctors mean the initial phase of pathological changes in the connective tissues of the ligamentous apparatus, which is characterized by the accumulation and improper redistribution of mucopolysaccharides and plasma proteins in the structure.
Mucoid degeneration develops gradually, the ligaments are thickened, but not fibered.
Complications in the form of damage to the medial meniscus, osteoarthritis with impaired fiber function, and gonarthrosis may also occur. The problems described above affect the flexion and extension ability of the joint, and also create the preconditions for rupture of ligament fibers in the future due to a decrease in their elasticity.
By the term intraligamentous injury of the anterior cruciate ligament, specialized specialists mean the process of irreversible replacement of tissues of ligamentous structures with cartilaginous components, which provokes the deposition of calcium salts and ossification of the structure as a whole.
Concomitant impairment of the motor function of the knee joint has a pathological effect on the entire musculoskeletal system.
Typical reasons for the development of this condition include regular microtraumas of the anterior ligaments, age-related slowdown of metabolic processes with deterioration of blood circulation in them, inflammatory pathologies in the knee, as well as the presence of background deforming osteoarthritis.
Most often, ligamentosis manifests itself in the form of swelling and severe redness of the knee, the presence of dull pain at the site of damage to the ligaments.
During instrumental diagnostic procedures, structural changes in the elastic component are assessed, the zone of ossification and deposition of calcium salts is determined, and a side or secondary disease of the knee joint is identified, which provokes further development of the problem.
As part of complex therapy, most often not only conservative treatment and classical physiotherapy with massage and exercise therapy are required, but also surgical intervention to remove the affected ligaments and replace them with appropriate synthetic or donor prostheses.
Ligamentite
Ligamentitis of the anterior cruciate ligament of the knee joint in the modern medical interpretation is an inflammatory process in the ligamentous apparatus that develops against the background of various infectious diseases or injuries. The main symptoms of this pathological process include pain in the joint area, its high sensitivity, regular occurrence of contractures, decreased joint mobility, and the appearance of swelling.
The development of ligamentitis can be caused by chronic infectious processes in soft tissues, injuries, regular long-term shock loads on the lower limb, and the presence of a number of systemic diseases, in particular diabetes, gout and rheumatoid arthritis.
Depending on the severity of the pathology and its form, conservative and surgical treatment methods can be used. In the vast majority of cases, surgery is not required
Tendinitis
The term tendonitis in relation to the anterior cruciate ligament of the knee joint has a secondary meaning and usually indicates acute or chronic inflammatory processes in the nearby tendons. Despite some functional similarities, these two types of joint components are different structures.
If ligaments consist of connective tissue and fix the joint capsule, preventing excessive mobility of the knee, then tendons mainly perform the function of fastening, being, in fact, extensions of the muscles with which the latter are fixed to the bone.
Tendinitis develops gradually and is a chronic pathology, manifested in the form of pain during movement, local swelling, a characteristic crunch during activation of the joint, and hyperthermia of the skin.
The treatment procedure for anterior cruciate tendinitis of the knee joint is fully consistent with the treatment of tendons for this condition. A conservative approach is predominantly used using immobilization, cold, non-steroidal anti-inflammatory drugs, physiotherapy, massage and other manipulations, if necessary, as prescribed by a surgeon, traumatologist, or orthopedist.
MRI in the diagnosis of acute anterior cruciate ligament (ACL) injury
ANTERIOR CRUCIATE LIGAMENT RUPTURE ON MRI
Studies show that the sensitivity of MRI for diagnosing anterior cruciate ligament (ACL) rupture ranges from 78% to 100%, and the specificity ranges from 68 to 100%. According to recent studies, the accuracy of the method reaches 95%, taking into account all errors in the interpretation of images when diagnosing a proximal, partial or old rupture. Sensitivity is also significantly reduced in the presence of damage to other large ligaments of the knee joint.
There is less data on the role of MRI in the diagnosis of ACL injuries in children compared to those in adult patients. It has been shown that the accuracy of the method is low in early adolescence; however, according to the results of a study conducted on patients 5-16 years old, the sensitivity of the method reached 95% and the specificity - 88%.
High-resolution 3 Tesla MRI did not significantly improve the accuracy of visualization of ligament injuries, despite improved imaging of the anteromedial or posterolateral fascicles.
Most tears (about 70%) occur in the middle portion of the ligament; 7-20% - at the site of its proximal attachment. Only 3-10% of tears occur distally at the attachment of the ligament to the tibia.
Get an MRI of the knee joint in St. Petersburg
PRIMARY (DIRECT) SIGNS OF ACL RUPTURE
Direct signs of a fresh ACL rupture (i.e., MRI phenomena that are absent in the case of an intact ligament) allow the injury to be diagnosed with great accuracy even in the absence of secondary signs:
- Lack of visualization of the ligament
- Focal heterogeneity of structure
- Curvature, curvature of the course
- Pathological position of the ligament axis
Most often, a fresh rupture is depicted on MRI images as a lack of visualization of the ligament with its replacement by local edema and hemorrhage caused by the injury. A partial tear, presented on images as an extended ACL with a signal of increased intensity, but with visualized intact fibers, is usually called an interstitial tear (or dissecting). This MR picture should be distinguished from mucoid dystrophy (degeneration) of the intact ligament (to be discussed in more detail below).
Lack of visualization as the primary sign of ACL rupture. Complete (or almost complete) absence of visualization of the ligament on sagittal images with inflammatory edema and hemorrhage at the site of its usual localization is one of the most common pictures in cases of fresh injury. Note: The normal ligament is sometimes poorly visible on sagittal images with short echo times (T1-weighted or gradient-echo images). This problem does not occur when analyzing T2-weighted images; In addition, images in different planes must be carefully compared.
Lack of visualization of the anterior cruciate ligament as a primary sign of injury. Sagittal T2-weighted fast spin-echo fat-suppressed image shows replacement of the ACL in the intercondylar fossa by hyperintense signal from edematous fluid.
Focal signal heterogeneity as a primary sign of ACL injury. T2-weighted image shows focal hyperintense edema and/or fluid collection at the proximal ACL.
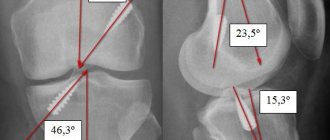
The position of the ACL axis is considered pathological if the axis is noticeably displaced in the horizontal direction compared to a line drawn along the arch of the intercondylar fossa (Blumensaat's line) on sagittal images. The position of the ACL axis can also be quantified, but the authors do not indicate the need for such an analysis.
Curvature/non-linearity as the primary sign of anterior cruciate ligament rupture. The T1-weighted sagittal MR image shows a sharply curved mid-ACL (arrow). A normal ligament usually has a gently curved, convex-down shape, while a wavy or sharply curved shape indicates pathological changes.
Primary signs of ACL injury. The sagittal image (top left) shows a high signal intensity disruption of the ligament with a fragmented appearance. Coronal T2-weighted images (top right) and T1-weighted images (bottom) show lack of fiber visualization and abnormal edema and fluid collection in the lateral aspect of the intercondylar fossa.
Flattened axis of the distal part of the ACL as a primary sign of injury. This sign has very high specificity. Visualization of the proximal part of the ligament is difficult, which also confirms the diagnosis.
Slightly flattened ACL axis as a primary sign of damage. The sagittal T2-weighted image shows a slightly more horizontal axis (indicated by the arrow) compared to the axis of the vault of the intercondylar fossa, or Blumensaat's line (indicated by the arrow) in a patient with an arthroscopically confirmed rupture of the anterior cruciate ligament.
The stump of a partially or completely torn ACL may prolapse anteriorly into the anterior aspect of the intercondylar fossa, resulting in an “angular” appearance of the ligament; may form nodules. This sign is called the bell-hammer sign, “bell-hammer sign” or “preoperative cyclops syndrome” (similar to the classic cyclops syndrome: focal fibrous growths anterior to the graft).
Along with evaluation of sagittal and coronal images, axial scans should be carefully examined for primary signs. The signal from the proximal ACL in the form of an oval-shaped hypointense shadow may be weakened, fragmented, completely or partially replaced by hemorrhage, or displaced away from the lateral wall of the intercondylar fossa.
ACL rupture on axial T2-weighted image with fat suppression. There is a lack of visualization of the ACL in the upper part of the intercondylar fossa. In addition, there is significant exudation into the joint cavity and a Baker's cyst.
SECONDARY (INDIRECT) SIGNS OF ACL RUPTURE
Other MRI phenomena are usually called secondary signs. The sensitivity of such diagnostic features is very limited; thus, their absence does not rule out ACL injury. Some of these signs, however, have a specificity of more than 80% in diagnosing ACL injuries (discussed below). As a result, they can help in establishing a diagnosis in cases where the presence of primary signs is doubtful.
Highly specific secondary signs include contusions and/or osteochondral fractures arising from a torsional mechanism of the joint, as well as a Segond fracture.
Damage to bones due to the twisting mechanism (pivot-shift)
When there is a rotational component to the ACL injury, there is external rotation of the lateral femoral condyle relative to the fixed tibia. This offset rotation causes the lateral femoral condyle to “cut” into the posterolateral region of the tibial articular surface, often causing characteristic bony lesions on both bones.
Injury to the lateral femoral condyle occurs most often near the anterior horn of the lateral meniscus, but may be displaced posteriorly if the injury occurs during knee flexion. Damage to the tibia involves its posterolateral aspect.
In severe injuries, bone damage may be accompanied by osteochondral fractures. On MRI in such cases, subchondral fracture lines or flattening of the surface of the cortical layer are visible. Sagittal scans (and lateral x-rays) may show the “deep lateral notch sign,” which is an enlarged (more than 1.5 mm deep) groove between the lateral femoral condyle and the patella. Such fractures are clearly visible on MRI, but often go undetected on X-rays. Such fractures appear as a slight cortical indentation or as an avulsion of a small bone fragment in the posterior part of the joint capsule.
Osteochondral fracture of the lateral femoral condyle with a pivot-shift mechanism on a sagittal gradient echo image in a 17-year-old patient with arthroscopically confirmed ACL rupture. The fracture is represented by a local depression of the cortical layer along the articular surface of the condyle (indicated by an arrow) near the anterior horn of the lateral meniscus.
Symptom of deep lateral notch of the femur as a secondary sign of damage to the anterior cruciate ligament. On a lateral radiograph, the lateral notch between the condyle and the patella is unusually prominent. Such findings should suggest a possible pivot-shift injury.
Typical torsional injuries, in particular osteochondral fractures of the tibia or femur, indicate ACL injury with a probability of greater than 90%. However, occasionally such injuries occur without an associated ACL rupture, more often in children or adolescents.
Contusions or impression fractures of the medial part of the tibia, occurring as a counter-impact type, are also characteristic of the described mechanism of injury. Most often, such injuries involve the posteromedial aspect of the tibial articular surface or the site near the insertion of the semimembranosus tendon.
Medial tibial injury combined with ACL injury. There is a high-intensity signal from a bone lesion in the posteromedial part of the articular surface of the tibia. This pattern is often found due to a sharp turn with displacement. Such bone damage is a sign of a rotational mechanism of injury. In such cases, tears of the medial meniscus are also common (even if the meniscus tear is not visible, there are often hidden tears in the area where the meniscus connects to the joint capsule).
Severe impact-type injury in the posteromedial zone of the tibia with an impression fracture in a 26-year-old patient with arthroscopically confirmed ACL rupture.
Previously, it was believed that MRI signs of such bone lesions persisted for up to 6 weeks. It is now clear that such lesions continue to be visible on MRI for 12-14 weeks after injury.
Presumably, such bone lesions visible on MRI may be diagnostic in determining the higher likelihood of corresponding cartilage damage, which may lead to subsequent degenerative changes in the joint.
Anterior displacement of the tibia
Anterior displacement of the tibia is the MRI equivalent of the anterior drawer sign seen on physical examination and thus indicates impaired anterior cruciate ligament function. The radiologist should look for this sign on sagittal sections taken through the center of the lateral femoral condyle. If the tibia is displaced anteriorly so that the distance between the vertical tangent lines drawn through the posterior edge of the femur and tibia exceeds 5 mm, then a fresh or old ACL rupture should be suspected. A shift of a smaller degree turns out to be unreliable.
Pathological malalignment of the tibia can also be suspected if the vertical tangent to the posterior surface of the cortical layer of the articular surface of the tibia passes through the posterior horn of the meniscus.
Anterior displacement of the tibia as an indirect sign of ACL rupture. A sagittal T2-weighted image of a patient with an arthroscopically confirmed ACL tear shows moderate anterior displacement of the tibia. As a result, a tangent line drawn along the posterior edge of the femur passes through the posterior horn of the lateral meniscus (the “uncovered meniscus” sign). In a healthy knee joint, this line runs behind the meniscus. This sign should be looked for on the image in a plane drawn through the middle part of the lateral femoral condyle. It is characteristic of both fresh and old ligament rupture.
Segond fracture: relationship with ACL injury
The Segond fracture is a characteristic tibial fracture that is associated with an ACL tear in 75-100% of cases. The Segond fracture is an ellipsoidal, vertically oriented bone fragment located parallel to the lateral cortical edge of the tibia approximately 4 mm distal to the articular surface. Segond fractures are traditionally associated with tractional avulsion of the middle third of the meniscotibial ligament from the joint capsule; Recently, the possible role of the iliotibial tract and the ligamentous complex of the lateral collateral ligament in the formation of a fracture has been increasingly emphasized.
What is a Segond fracture? The T1-weighted image shows a characteristic elongated bone fragment located along the proximal and lateral edge of the tibia (indicated by the arrow). This fracture is associated with a rupture of the ACL (a ligament stump is identified in the intercondylar fossa).
A Segond fracture on an anteroposterior radiograph shows a linear bone fragment located parallel to the proximal lateral surface of the tibia (indicated by an arrow). Patients with a Segond fracture are at very high risk of ACL rupture.
Segond fractures are not easily seen on MRI and are therefore often missed. Often the attention of the doctor evaluating the image is distracted by a focus of increased signal resembling edema in the medulla of the adjacent lateral part of the articular surface of the tibia. The bone fragment from a Segond fracture in the acute period appears on a T2-weighted image as a high-intensity focus of edema in the medulla; Over time, the signal becomes isointense with respect to the bone marrow (or low-intensity, which corresponds to sclerosis of the bone tissue) and can spread down the bone.
On photographs in direct projection, a Segond fracture should be distinguished from a fracture of the Gerdi tubercle, i.e. its traumatic separation in the anterolateral direction due to traction of the iliotibial tract; this fracture is better visible on an x-ray in the position of external rotation. In contrast, a Segond fracture is better visualized on a classic anteroposterior x-ray.
Avulsion fracture of the intercondylar eminence of the tibia
In fact, the anterior cruciate ligament is not attached directly to the intercondylar eminence of the tibia, but somewhat laterally and anteriorly. Thus, fractures of the tibial intercondylar eminence may occur in patients with an intact ACL. However, the possibility of ACL injury should be kept in mind when evaluating patients with such fractures. An avulsion fracture of the intercondylar eminence of the tibia, accompanied by damage or functional insufficiency of the ACL, indicates, in most cases, an extensor mechanism of injury. Among adults, only 5% of traumatic ligament injuries are accompanied by an avulsion fracture of the tibia. Such fractures are more likely to occur in isolation in children, while in adults they represent a serious injury associated with many other injuries.
Secondary functional insufficiency of the anterior cruciate ligament due to a distal avulsion fracture of the tibia. An avulsion fracture (arrowed) is seen at the typical distal ACL insertion site near the intercondylar eminence. This finding should suggest a possible involvement of the ACL because the ACL inserts just lateral to the intercondylar eminence. In children, most often this represents an isolated injury (with or without ACL involvement). In adults, however, such fractures occur when significant force is applied; fractures are often longer than expected and are often accompanied by numerous other injuries.
Avulsion fracture of the tibia at the ACL insertion site. The sagittal gradient echo image shows a displaced bone fragment at the distal ACL insertion. The doctor should be aware of the possibility of such a fracture as they are often missed. In unclear cases, a CT scan or a second opinion may be helpful.
Several classifications of tibial intercondylar eminence fractures have been proposed. The choice of treatment method is controversial; For larger bone fragments, surgery is often performed to reduce them.
Get a CT scan of the knee joint in St. Petersburg
PARTIAL RUPTURE OF THE ANTERIOR CRUCIATE LIGAMENT OF THE KNEE JOINT
Partial damage to the anterior cruciate ligament accounts for about 10-43% of all tears. This type of rupture is more common in children. Features of management and treatment of patients with such injuries are still being discussed. A low-grade tear involving less than 25% of the ligament as determined by arthroscopy has a favorable prognosis; a 50-75% rupture is highly likely to develop into a complete ACL rupture. Overall, less than 50% of patients with an unrepaired partial tear are able to return to their preinjury level of activity.
MRI allows one to accurately distinguish a normal ACL from a pathologically altered one, but is a much less reliable method in diagnosing partial tears.
Van Dyck et al listed the main features of the MRI picture of partial ACL ruptures. First, partial tears can look like a full tear. Overestimating the severity of the tear in such cases, fortunately, has little effect on the outcome, since most high-grade partial tears progress to a complete tear as soon as the patient returns to his usual level of physical activity. It is worth emphasizing once again that secondary signs of an ACL rupture (for example, bone damage of the pivot-shift type) are characteristic of both complete and partial high-grade ruptures, and therefore do not allow one to reliably distinguish a complete rupture from a partial one.
Subtotal rupture of the anterior cruciate ligament of the knee joint. On the left, the T2-weighted image shows some attrition of the ACL; probably slight flattening of the ligament axis. In the center is the same patient in the axial plane: a poorly visible, fragmented ligament is visible. On the right, typical bone injuries of the pivot-shift type are visualized in the area of the lateral condyle of the femur and the posterolateral surface of the tibia. The Lachman test is negative. From these images it is clear, firstly, that secondary signs of rupture (for example, bone damage of the pivot-shift type) can be observed in partial ruptures, and secondly, that high-grade partial ruptures are difficult to differentiate from complete ruptures.
Secondly, a partial rupture may resemble mucoid dystrophy (degeneration) of the ACL. The ligament is thickened, the fibers appear straight and unchanged, but are sometimes interspersed with areas of medium to high signal intensity. This corresponds to a dissecting type of tear, which is less severe than a transverse tear, due to which physical examination does not reveal functional impairment of the joint.
Partial ACL injury: should be differentiated from mucoid ACL degeneration. The patient was admitted with complaints of pain, without a history of previous trauma. The ACL is enlarged due to hyperintense areas that do not correspond to edema, which intersperse intact ACL fibers. Differential diagnosis includes mucoid degeneration (quite common) and dissecting partial tear. To establish a diagnosis, it is necessary to clarify the anamnesis and conduct the Lachman test.
Third, an MRI image showing partial ligament injury may be normal. This should be kept in mind and a partial rupture should be considered in cases where there is an appropriate mechanism of injury, physical instability of the joint, or if there are indirect signs of damage to the anterior cruciate ligament on MRI (for example, bone lesions or anterior displacement of the tibia).
As previously discussed, a complete or partial rupture of the ACL can form a stump that protrudes anteriorly into the anterior region of the intercondylar fossa of the femur (the so-called hammer sign or preoperative cyclops syndrome). Lefevre et al. indicate that despite the fact that this sign is not typical, it may be useful in the diagnostic search. This sign is either (1) a protruding ACL stump or (2) a heterogeneous nodule with inhomogeneous signal that projects anterior to the ACL. Histological examination of such nodes reveals disorganized ACL fibers, fibrosis, inflammation and hemorrhage, which resembles the histological characteristics of tissue changes in post-transplantation cyclops syndrome; as in patients with post-transplantation arthrofibrotic changes, in such cases there is limited mobility in the joint.
From the above, it is clear that MRI can be of significant assistance in the diagnosis and management of partial tears, and that the findings on the images should not be ignored, even if the Lachman test is negative. Additional coronal oblique, isotropic voxel, or flexion scans may also be helpful.
Get an MRI of the knee joint in St. Petersburg
DAMAGE TO THE ANTERIOR CRUCIATE LIGAMENT OF THE KNEE: TREATMENT
The choice of treatment for a torn ACL depends on the extent of the injury and your specific goals and needs. Some people with this type of injury may continue to lead their normal lives but subsequently suffer long-term effects from the injury. For athletes, surgery and physical therapy may be the best choice to get you back into physical activity as quickly as possible.
What to do if you have an anterior cruciate ligament injury?
- Avoid physical activity until you see your doctor
- Create measures to immobilize the limb (splint, tight bandage)
- Keep your leg above your heart
- Put ice on your knee
- Use crutches to relieve pressure on your knee
SURGERY FOR ACL RUPTURE
Sometimes complete surgical repair of the ligament using hamstring, donor material, or artificial material is required. After surgery, you may need up to six months of physical therapy to regain full range of motion and strength in your legs. As a rule, reconstructive operations have good results. With the right choice of treatment method, complete recovery is possible. An accurate assessment of MRI results is a prerequisite for successful treatment. If there are doubts or inaccuracies in the interpretation of the images, an additional second opinion from a specialized radiologist can be obtained.
TREATMENT OF PARTIAL RUPTURE
Treatment recommendations for patients with partial ACL tears are still under active debate. Factors that favor the choice of conservative treatment include older age, a negative or near-negative Lachman test result, moderate daily physical activity, and arthroscopically detected damage to less than 50% of the ACL fibers. Reconstructive surgical treatment is more suitable for young and physically active patients, patients with a positive Lachman test, involvement of more than 50% of the ACL fibers, or involvement of the posterolateral fascicle on arthroscopy.
Materials used in preparing the text:
https://emedicine.medscape.com/article/400547-overview#showall
Pavel Popov
Candidate of Medical Sciences, Member of the European Society of Radiologists
Causes of pathology
Knee meniscus injury
Functionally, the ACL of the knee joints helps keep the lower leg from moving inward or forward. Taking this into account, the mechanism of injury that causes sprain or rupture of the ligament becomes more clear. The reasons for its damage are formulated as follows:
- direct injury due to a blow to the thigh or lower leg;
- indirect injury (torsion on one book combined with sudden braking).
The most common mechanism of ACL rupture is simultaneous outward deviation of the tibia and torsion of the femur in the opposite direction. Often this type of damage is diagnosed in basketball, volleyball and football players. During the game, athletes have to turn sharply while running, or after making a jump, they are forced to sharply turn their body in the direction opposite to that in which the supporting leg is turned.
Provided that the described movement has a large amplitude, there will be a violation of the integrity of three structures simultaneously:
- anterior cruciate ligament;
- internal meniscus;
- internal collateral ligament.
This type of injury is informally called a “blowout knee joint.” The condition was first described in 1950.
The mechanism of injury opposite to that described above, involving deviation of the tibia and torsion of the thigh in different directions relative to each other, can lead to a tear of the outer meniscus.
Another rupture mechanism occurs in people who engage in alpine skiing. Injury occurs due to a fall. The result of pronation of the lower leg is an isolated injury - a rupture, complete or partial, of the anterior cruciate ligament.
Important: the damage is not accompanied by a violation of the integrity of the menisci or other structures of the knee joint.
After knee ligament suturing surgery
In orthopedics and traumatology, many provoking factors are identified that lead to the development of damage to the anterior cruciate ligament.
Treatment of ACL rupture.
As a rule, advantage is given to conservative treatment. Only in cases of persistent dysfunction and instability is surgical treatment indicated. It is also necessary, when transporting the patient to the clinic, to provide rest to the leg and cold to the injured area to reduce swelling and to avoid an increase in hemarthrosis. For fixation, orthoses are used as the most convenient option for limb immobilization.
Conservative technique
To relieve pain and reduce the inflammatory response, non-steroidal anti-inflammatory drugs are prescribed. If hemarthrosis is present, blood is removed from the joint using a syringe. Sometimes intra-articular glucocorticosteroids are prescribed. After reducing inflammation, a course of intra-articular injections of hyaluronic acid or platelet-rich plasma can be prescribed to speed up the regeneration of damaged structures. For a speedy recovery, exercise therapy, mechanotherapy, physiotherapy, etc. are prescribed.
Anterior cruciate ligament arthroscopy
Arthroscopy is the most modern and effective method of repair for ACL rupture.
Arthroscopy is performed in cases where there is instability of the joint or other tissues are damaged. The operation is a minimally invasive method of diagnosis and treatment, since the cavity is not opened, and surgical instruments are inserted into it through two small incisions in the skin. The arthroscope allows you to visualize all structures at multiple magnification, thanks to which the doctor can most accurately make a diagnosis and begin surgical treatment.
Characteristic symptoms
With any form of meniscal degeneration, the following characteristic symptoms are observed:
- pain in the affected area;
- swelling;
- sensation of a foreign body when bending;
- clicks and crunching sounds while moving;
- blockade of the joint with a bent knee.
Injury
There are some differences in manifestations between traumatic injury and meniscal degeneration. Immediately after a bruise or blow, there is a sharp pain and slight swelling of the soft tissues.
Damage to the red zone of cartilage leads to hemorrhage into the joint cavity. The intensity of the pain syndrome varies. Sometimes a person cannot even step on his foot, and in some cases, discomfort is felt only with certain movements.
If the integrity of the internal meniscus is compromised, the patient feels pain along the tibial ligament when bending the limb. And when palpating the muscles of the front of the thigh, a decrease in tone is noted.
When the outer meniscus is damaged, the pain increases significantly when trying to turn the lower leg inward, and radiates to the outer part of the joint. If a meniscus tear occurs, the separated part can greatly impede movement.
A large piece of cartilage can even lock a joint in a certain position. Symptoms of an injury also depend on which part of the meniscus is torn. Rejection of the posterior horn results in difficulty in flexion movements, and damage to the body and anterior horn is accompanied by impaired extension.
Since the meniscus is rarely damaged in isolation, a violation of its structure with degenerative changes in the anterior cruciate ligament often occurs. This pathology is accompanied by a sharply occurring pronounced edema.
Degeneration
Meniscal degeneration in its pure form is most often observed in people after 40-45 years of age. This is associated with the appearance of chronic joint diseases and age-related tissue changes. A significant disruption of the tissue structure leads to the fact that injury is not necessary for the development of pathology.
The problem occurs after the usual action of squatting, getting up from a chair or bed.
If you are haunted by aching pain in your knee, which either disappears or appears with renewed vigor, you can already assume that there are changes in the meniscus. About 90% of pathologies of the knee joint are caused by damage to the “shock absorber”.
Symptoms largely depend on the nature of the pathology. Ruptures are accompanied by severe pain, blockade of the leg in a bent state and swelling. With serious damage to the medial meniscus, hemorrhage into the joint cavity often occurs - hemarthrosis. Significant swelling and severe pain are also characterized by meniscal cystosis.
Tears and detachments from the attachment site are often chronic in nature and are manifested by periodic pain and a feeling of impediment in movement.
There is a diagnostic test: go up and down stairs or slopes. With pathology of the meniscus, the pain in the knee intensifies when moving down.
Secondary degenerative-dystrophic transformations in the medial meniscus, that is, those arising due to other pathologies of the body or diseases, are also characterized by a chronic course. Often in such cases there are clicks and rolling* of the joint during movement after a long period of rest, and sometimes there is pain in the knees.
The increase in symptoms occurs gradually as the cartilage layer thins and salts or uric acid crystals accumulate in it (the latter in case of gout). In the absence of adequate treatment, the final stage of meniscopathy becomes contracture - a stable violation (limitation) of joint mobility.
* Rolling – sensations of pathological mobility, instability and displacement of the articular surfaces of bones.
The following symptoms are common to all types of meniscal degeneration:
- soreness,
- swelling,
- blockage of the joint in a bent position or sensation of a foreign body in the knee,
- clicks and crunches,
- numbness of the knees after a long period of inactivity.
Symptoms of damage
The patient can often associate the onset of symptoms with exposure to a traumatic factor. When the ligament ruptures and the joint is dysfunctional, the vessels are damaged and hemorrhage occurs – hemarthrosis. Its increase leads to increased pain to the point that it is impossible to touch the sore spot. This can make diagnosis difficult. To avoid extensive hemarthrosis, it is necessary to apply cold and hold it until arriving at the clinic.
Symptoms appear quite acutely and increase over time. There are complaints about:
- Sensation of displacement, twisting of the lower leg, instability of the knee joint.
- Cracking in case of injury.
- Severe acute pain not only in the area of the bruise, but also in the area of the joint cavity.
- Swelling that appears on the first day.
- The pain intensifies with movement.
Clinical picture of the pathology
Knee swelling
ACL injury is most often preceded by a knee injury. The victim feels acute pain and notes the reactive development of edema. A ligament rupture is often accompanied by a popping sound. However, this sign is also observed when other knee ligaments are torn. A feeling of the lower leg being dislocated forward or to the side is a reason to immediately consult a doctor.
A rupture of the anterior cruciate ligament is accompanied by bleeding into the cavity of the knee joint - hemarthrosis. During the first few days after injury, this condition is so pronounced that it eliminates the possibility of palpation.
Classification
Because the anterior cruciate ligament has two bundles, only one or both of them can be damaged. There is a possibility of complete tearing off along with a section of the bone at the place of its attachment to the lower leg (Segond fracture).
There are three degrees of ACL rupture:
- The first is characterized by stretching, accompanied by moderate pain and swelling. As a rule, the ligament is restored after such cases.
- Second , there are also small tears. Recovery is longer and the regimen plays a decisive role. However, relapses are likely due to a decrease in its strength.
- The third degree is a complete break. The pain is sharp, intense, accompanied by limitation of movement and joint instability. Hemarthrosis (free blood due to vascular damage) is most likely. In this situation, the issue of surgical treatment is resolved.
Also, according to age, fresh ruptures are distinguished - up to 3-5 days, stale - up to 3 weeks and old - more than three weeks. The choice of treatment tactics depends on the determination of these parameters.
Causes of degeneration
The anatomical features of the location and structure of the menisci determine the high incidence of pathologies both among young people and among mature people. Most often, athletes, ballerinas, dancers suffer from ruptures, damage and cystosis - that is, people who are in constant motion and experience high loads.
- dysplasia – abnormal formation of the knee joint;
- gout, syphilis, tuberculosis, rheumatism and other diseases that can affect joints;
- sprains of ligaments, as well as their incorrect formation;
- flat feet (low shock absorption of the foot is compensated by increased load on the knee);
- high physical activity;
- excess weight.
Structure of the anterior cruciate ligament and knee joint
The knee joint is the most complex anatomical structure of the musculoskeletal system, in the formation of which three bones take part: the tibia, the femur, and the patella.
The normal functioning of a joint is impossible without ligaments that connect bone tissue into a single mechanism and ensure its stability:
- anterior cruciate ligament;
- posterior cruciate ligament (PCL);
- internal collateral ligament;
- own patellar ligament;
- external collateral ligament.
Thanks to the ligaments, knee movement is possible only in a strictly designated range, which protects it from injury. The slightest excess of this amplitude leads to ligament ruptures or sprains. There is a misconception that ligaments are very elastic, but this is a completely wrong statement.
The anterior cruciate ligament is the same obstacle that limits the mobility of the lower leg relative to the thigh anteriorly. It originates from the edge of the lateral condyle of the femur and ends at the central part of the tibia. On the back side of the ACL is the PCL (posterior cruciate ligament). To understand the reason for the name cruciate ligaments, you need to look at them from the front - they form a cross.
When considering the anatomical features of the anterior cruciate ligament, it is worth noting that its length is 25-30 mm, thickness - 7-12 mm.
Diagnosis of pathology
Lachman test
The victim's leg is bent at a right angle, the lower leg is pulled towards the person conducting the test. The degree of displacement is compared with a healthy limb. Additionally, the foot rotates inward and outward.
If a questionable or inaccurate result is obtained, an arthrometer is fixed to the lower leg - a special device that allows you to evaluate the degree of mobility automatically.
The obtained figures are also compared with indicators taken from a healthy limb.
Lachman test
The leg bends at the knee. The angle of 20-30° is strictly observed. The specialist evaluates how much the lower leg moves forward, as well as the sensations of the victim before and after the manipulation. There are three degrees of insufficiency of ACL functions. The first is that the displacement of the tibia increases by 1-5 mm. The second is an indicator within 6-10 mm. Third - the displacement is more than 10 mm.
The tests are preceded by palpation. However, due to hemarthrosis and pronounced pain and edema syndrome, this is difficult. To eliminate these phenomena, the victim is subjected to aspiration or removal of blood from the joint with a syringe.
Radiography
Allows you to exclude or confirm the diagnosis of fracture. Especially if a Segond fracture is suspected. Most often, this pathology is diagnosed in children and adolescents.
The accuracy of diagnosis with this method is 95%. Helps detect hematomas near the condyle of the femur, as well as the outer part of this bone formation.
Treatment methods
When grade 1 and 2 degenerative damage to the menisci of the knee joint develops, treatment consists of relieving pain, improving blood flow and nutrition in the joint, and restoring the functionality of the joint.
In the initial stages, conservative therapy is used using medications, physiotherapy, and exercise therapy. In severe conditions and the lack of effectiveness of conventional therapy, it is necessary to resort to surgery.
The patient should move with the help of a crutch or stick during the rehabilitation period after surgical treatment, or during an exacerbation and taking medications. observe semi-bed rest.
Wearing a bandage or bandage gives a good result for temporary joint sparing. If there is effusion or blood in the cavity of the joint capsule, puncture and evacuation of the contents are performed.
To relieve pain, the patient should take NSAIDs and analgesics (Analgin, Ibuprofen, Voltaren). In case of severe discomfort, the doctor may use local administration of novocaine or glucocorticoids (Prednisolone, Hydrocortisone).
In rare cases, short-course opioid medications (Promedol) are used. Long-term use of chondroprotectors helps restore cartilage tissue. If there is an identified cause of the disease, you should observe dietary restrictions and take immunocorrectors.
Physiotherapy
During the acute period, physiotherapeutic methods are not used. But they have a positive effect to speed up rehabilitation and prevent re-exacerbation. Typically used:
- UHF or microwave;
- ozokerite;
- shock wave therapy.
The techniques promote blood flow to the affected area, accelerate healing and restoration of cartilage tissue.
To strengthen the leg muscles, relieve excess tension from them, and also prevent venous stagnation in the sore limb, special exercises are used. The first time after reducing the severity of the pathological process, movement should be carried out smoothly and slowly.
The load increases gradually, day by day, due to the number of repetitions and approaches. If pain, tension, or extreme fatigue occurs during movement, you should stop exercising and rest your leg.
Operation
Surgery is used for complete meniscal tears or unsuccessful treatment with drugs when the disease progresses. The cartilage pad is removed through small incisions in the knee. Then it is replaced with an implant. The surgical method is used only if there are no signs of acute inflammation.
Therapy for degenerative changes in the menisci completely depends on the nature of the damage. Acute injuries serve as a direct indication for the use of conservative treatment methods:
- First of all, a puncture of the joint is performed, eliminating its swelling and restoring mobility. Sometimes several procedures are required, since active exudation (secretion of inflammatory fluid) in the joint lasts up to three to four days.
- Analgesics are prescribed, preference is given to narcotic drugs (Promedol and its derivatives), because other drugs in this case, as a rule, are not able to relieve the patient of pain.
- Chondroprotectors provide the body with the necessary substances to restore the damaged area of the meniscus.
- Anti-inflammatory drugs.
- At the rehabilitation stage, physiotherapeutic methods are used as an auxiliary means - ozokerite, UHF, iontophoresis, shock wave therapy.
- For 14 days, a splint is applied to the straightened leg to secure the joint in the required position.
In case of ruptures, surgical intervention is indicated: instruments are inserted into the knee joint through two miniature incisions and the damaged area is sutured. Serious injury may require the cartilage lining of the joint to be removed and replaced with an artificial one. All surgical procedures are performed only after signs of inflammation have subsided.
Chronic dystrophies, joint dysplasia and abnormal development of the ligamentous apparatus require exclusively surgical treatment.
If the cause of degeneration is chronic diseases, such as rheumatism and gout, along with surgical methods, the underlying disease is also treated (diet, immunocorrectors and other methods).
Degenerative transformations of the menisci are a fairly common pathology that requires immediate consultation with a specialist. The future functioning of the joint depends on the timeliness of treatment, and delays can cause the spread of degenerative processes to other elements of the joint. Therefore, do not delay your visit to the doctor, take care of yourself and be healthy!
Treatment of menisci and cruciate ligaments
The choice of treatment technique is determined by the severity of the injury. Only a doctor can answer the question of how to treat. And it’s better if it’s an experienced orthopedic surgeon from the Central Clinical Hospital of the Russian Academy of Sciences. In each individual case, a personal approach is required to determine the need for surgical, conservative therapeutic, physiotherapeutic treatment or a combination of methods.
Conservative treatment. Its task is to eliminate the blockade of the joint. To do this, a puncture is performed, the joint is freed from effusions and blood, novocaine is administered, after which the blockade is removed. This is a step-by-step manipulation. If the outcome is favorable, immobilization is performed. For treatment use:
- UHF therapy;
- physical therapy;
- massage;
- restorative drugs.
If conservative treatment does not produce results or the disease has become chronic, the patient is prescribed surgery . The technique in this case is selected depending on the complexity of the case, the age of the patient and the presence of complications:
- Partial or complete removal of the meniscus (meniscectomy);
- If the victim is young, physiotherapeutic rehabilitation can be carried out - this is the most gentle method;
- The safest and preferred method is arthroscopy, when the damaged segment is sutured;
- A relatively new method - intra-articular fastening of the meniscus - is characterized by low trauma and the use of special clamps;
- Meniscus transplantation is an expensive procedure and is used when other methods are powerless. There are contraindications for the operation.