Orthopedics
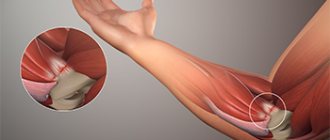
Epicondylitis is a disease characterized by pain in the elbow joint. Occurs as a result of overload of the arm muscles. Most often affected: professional athletes, tennis players, golfers and people whose profession involves performing frequently repetitive movements at the elbow.
The main complaint with epicondylitis is pain in the elbow area. Based on the location of the pain, lateral and medial epicondylitis are distinguished:
- TENNIS ELBOW. Lateral (external): pain occurs when extending the fingers and rotating the hand.
- GOLFER'S ELBOW. Medial (internal): pain occurs when bending the fingers.
As the disease progresses the pain becomes constant and its intensity increases. Other symptoms may appear: a feeling of “weak arm”, redness of the skin, swelling.
In advanced cases, a person may completely lose the functionality of his hand.
Treatment methods for epicondylitis
Treatment is selected individually . Depends on the patient’s profession, duration of the disease, and severity of pain. You will need to give up professional activities for the entire duration of treatment.
- Conservative treatment is aimed at relieving inflammation and eliminating pain.
- Orthotics Special orthoses are used, they limit movement and fix the joint in the correct position.
- Physiotherapeutic procedures, massage The following may be prescribed: pulsed magnetic therapy, electrophoresis, exposure to infrared laser radiation, cryotherapy, paraffin and ozokerite applications. The course consists of 10-12 procedures.
- Surgical treatment If there is no effect from conservative treatment (at the third relapse), surgery is indicated - release of the distal tendons of the shoulder muscles.
An integrated approach is possible. There are contraindications, consultation with an orthopedist is necessary.
Treatment methods for lateral epicondylitis.
“Whatever the stage, methods such as load modification, gradual therapeutic progression and adaptation should form the basis of treatment.”
Goals include reducing pain, maintaining motor function, increasing grip strength and endurance, and returning to function. During the acute phase, treatment focuses on reducing pain symptoms and inflammation. The use of corticosteroid injections is avoided until the full potential of conservative techniques has been exploited. The basis is training, therapeutic progression of the load and its modification. Individually selected exercises take into account the load, painful angles of movement, strength, endurance, preferences and characteristics of the patient. Eccentric exercises (EC) have the highest evidence of effectiveness. EC stimulate the restoration of the matrix of collagen structures and collagen synthesis, have an analgesic effect and improve the tendon’s tolerance to physical activity.
Correction of biomechanics, muscle imbalances and motor control training should be the basis of selected exercises to eliminate wrist extensor overactivity and compensation in upper extremity functionality. Self-massage and stretching of the tendon are usually limited, as they can increase compression and friction, which have a negative effect on it. The use of shock wave therapy and other procedures has moderate evidence and is used in the first 4-6 weeks as additional physical support. Whatever the stage of development of tendinopathy, modification of load and achievement of tissue tolerance should be the main principle of treatment of lateral epicondylitis.
- It is important to limit the functionality of the affected arm. Athletes should stop training. This way you can quickly relieve muscle spasms and inflammation, and avoid repeated microtraumas.
- The doctor prescribes anti-inflammatory drugs, which reduces pain and swelling. Sometimes it is necessary to use glucocorticosteroids in addition to NSAIDs. Additionally, muscle relaxants are prescribed if necessary.
- Anti-inflammatory drugs and platelet-rich plasma are injected into the epicondyle area.
- At the initial stage, it is recommended to periodically apply cold to reduce pain.
- Taping and orthoses are good helpers on the path to recovery - they limit the rotation of the arm, promote reduction and contribute to less trauma.
- Physiotherapeutic procedures (magnetic therapy, shock wave therapy, electrophoresis, electromyostimulation, acupuncture) are used in courses in combination with anti-inflammatory therapy.
- Physiotherapy exercises are prescribed after pain has been eliminated to restore the function of the upper limb.
After treatment, it is important to follow a therapeutic and protective regimen to avoid relapses of inflammation and repeated injuries.
Arthroscopy of the elbow joint
In advanced cases, when conservative treatment does not give the expected result, surgical intervention may be recommended. The most gentle method is arthroscopic surgery. It allows you to preserve the surrounding tissue as much as possible and remove the affected areas, and then restore muscle fixation. They perform sanitation in the area of damage, eliminate fibrous formations, adhesions, and release nerves from compression. Rehabilitation after arthroscopy is faster than after an open approach. With this operation, there is less risk of damage to nerves and blood vessels due to good visualization of all structures. Immediately after the operation, the arm is subject to immobilization, that is, wearing an orthosis. Rehabilitation measures begin after 1-2 weeks. They include physical therapy, wearing braces, taping, and kinesiotherapy. The results of complex treatment for this pathology are optimistic: patients regain functionality and painless movements.
Our specialists are always ready to help you! Call us by phone or.
Postoperative period
Recommendations will depend on the treatment method. If there was an operation:
For 1-2 weeks, the arm is immobilized with an orthosis. After 2 months, you need to do stretching exercises. After 4-6 months, you will be able to return to sports activities.
For prevention purposes:
- monitor the dosage of the load on the forearm, take pauses in work
- choose the optimal working position
- Always warm up before starting a workout
- athletes use bandages/elbow pads to fix their elbows, select high-quality sports equipment
Elbow epicondylitis (Golfer's Elbow, Tennis Elbow)
Security mode
Therapeutic tactics depend on the duration of the disease, the severity of clinical symptoms and the causes of tendon overload.
For fresh epicondylitis with mild pain, it is sometimes sufficient to prescribe a protective regimen that excludes certain movements of the limb. If epicondylitis occurs due to professional overload, the patient is issued a sick leave. If the cause of the disease is sports activities, it is recommended to temporarily stop training. After the pain disappears, the load is gradually increased. To prevent relapse, it is necessary to establish what caused the muscle overload. Patients are advised to pay attention to the technique of performing stereotypical movements, use other tools, take regular breaks during work, review their training regimen, etc. Sometimes the listed measures are sufficient to eliminate the symptoms of the disease and prevent relapses. If this method is ineffective, as well as with intense pain and prolonged epicondylitis, more active treatment is necessary.
Drug therapy
The arm is provided with complete rest by applying a splint and hanging the limb on a scarf. After the pain has reduced, the plaster is removed, and patients are advised to use topical NSAIDs. NSAIDs in tablets are usually not prescribed, since the risk of side effects (irritation of the stomach wall) outweighs the potential of anti-inflammatory therapy.
In case of persistent sharp pain, blockade of the affected area is carried out with solutions of glucocorticosteroids. The best option for epicondylitis is blockade with betamethasone, since this drug does not cause increased pain immediately after the blockade and does not provoke degenerative changes in tissue at the injection site. Betamethasone can be replaced with methylprednisolone or hydrocortisone, but in this case the patient must be warned that the pain will intensify on the first day after the blockade, and only then will relief come.
The use of triamcinolone for epicondylitis is contraindicated, since this drug, when administered subcutaneously, can cause disruption of skin pigmentation and the formation of adhesions between the skin and the underlying tissues (in this case, the surface of the condyle of the humerus).
Symptoms and diagnosis
Patients with lateral epicondylitis typically have pain in the elbow, which intensifies when holding a weight in the arm during extension. Playing tennis or similar sports activities may actually cause epicondylitis, but it is often associated with other activities. On palpation in the area of tendon attachment, about 1 cm distal to the middle part of the epicondyle, compaction and pain are noted. In addition, there is a decrease in muscle strength with resistance to grip and with supination of the hand. There are also tests such as the chair rise (with the arm pronating) and the coffee cup test (in which the patient lifts a full cup of coffee). Typically, these tests cause pain in the elbow. The diagnosis of lateral epicondylitis is usually made based on the clinical picture. Epicondylitis can be of moderate or severe severity.
With medial epicondylitis, pain is localized in the medial part of the elbow. Symptoms (pain) in patients with medial epicondylitis develop gradually (with the exception of acute trauma). Muscle weakness when grasping is also noted. Patients may have a history of playing golf, basketball, or volleyball. On palpation in the area of the flexor-pronator tendons (5-10 mm and distal to the middle part of the medial epicondyle), induration and tenderness are noted. In addition, pain increases when the wrist resists forearm flexion and pronation to 90°. Flexion contractures can develop in professional athletes due to muscle hypertrophy. It is necessary to differentiate medial epicondylitis from tunnel syndrome and ulnar nerve neuritis. There is a simple "milking" test (simulated milking) that causes increased pain in medial epicondylitis.
However, sometimes there is a need for instrumental diagnostics (imaging) for differential diagnosis with other diseases. It has been noted that 5% of people with a primary diagnosis of lateral epicondylitis have radial tunnel syndrome. Radial tunnel syndrome is compression of the posterior interosseous nerve (deep branch of the radial nerve) in the radial tunnel. Many patients with this syndrome have a history of activities involving frequent pronation and supination of the forearm. The most common MRI finding in radial tunnel syndrome is swelling, denervation, or atrophy in the muscles innervated by the posterior interosseous nerve.
MRI diagnostics helps to make an accurate diagnosis. But normal visualization is only possible with high-field devices (magnetic field power 1 tesla or more).
Ultrasound is a fairly informative research method that allows you to visualize this pathology.
EMG study is necessary only for signs of conduction disturbances (for tunnel syndromes and neuritis).
Treatment of epicondylitis
Treatment of epicondylitis is mainly conservative: the use of orthoses during an exacerbation and at night, shock wave therapy, ultrasound therapy or galvanization, sometimes local administration of corticosteroids, drug treatment (NSAIDs). In addition, exercise therapy is necessary to restore function (gradually increasing the load on the forearm). Conservative treatment methods are effective in 90% of cases. If there is no effect from conservative treatment within 3-6 months, surgical treatment is recommended.