Injections into the elbow joint and medications used
As part of complex therapy, the following drugs are administered intra-articularly:
- Hormonal agents have powerful anti-inflammatory and analgesic effects and are necessary for urgent relief of pain and inflammation. For example, injections for elbow bursitis help stop the accumulation of inflammatory fluid.
- Chondroprotectors - nourish and improve metabolism in the cartilage of the elbow joint.
- Hyaluronic acid is a synovial fluid prosthesis that helps lubricate articular cartilage and reduces friction.
Diprospan is often administered for therapeutic purposes. An injection into the elbow joint of this medicine, a glucocorticosteroid, is famous for its long-lasting and rapid action. Side effects are minimal. This medication is also used for therapeutic blockades in the treatment of the spine in case of severe pain. The pain goes away almost immediately. For Diprospan injection into the elbow joint, the price at the Stoparthrosis clinic is indicated on the website. All injections have different costs.
Pharmacological properties of the drug Diprospan
Pharmacodynamics. The drug Diprospan is a combination of soluble and poorly soluble betamethasone esters for intramuscular, intra-articular, periarticular, intrasynovial and intradermal administration, as well as for administration directly into the lesion. Diprospan has high GCS activity and insignificant mineralocorticoid activity. The small size of betamethasone dipropionate crystals allows the use of small diameter needles (up to 0.9 mm) for intradermal injections and injection directly into the lesion. Pharmacokinetics. Betamethasone sodium phosphate is a highly soluble component that is rapidly absorbed from the injection site, which ensures a rapid onset of therapeutic action. Betamethasone dipropionate is a poorly soluble component that is slowly absorbed from the depot created at the injection site and provides a long-lasting effect of the drug.
Indications and contraindications
Indications for injections include inflammatory processes in the articular and periarticular area, synovial bursa, and degenerative processes. Also, local administration of drugs is prescribed for fluid accumulation. An injection for bursitis of the elbow joint is not recommended during periods of acute infection, during pregnancy, with skin problems in the elbow area and cancer. Before therapy, consultation with a doctor is important.
Do you need to get an injection in the elbow joint with Diprospan or another? Contact the Stoparthrosis clinic. It has modern equipment and experienced specialists. Here, all treatment and diagnostic procedures are carried out by qualified doctors. Get diagnosed and treated, return to a full life!
Author of the article:
Litvinenko Andrey Sergeevich
Orthopedist
Make an appointment
Recent publications by the author:
- Medicine chondroprotector
- Hyaluronic acid injections: reviews
- Fermatron injections into the hip joint
- Finger injections
Indications for use of the drug Diprospan
- Rheumatoid arthritis, osteoarthritis, bursitis, tenosynovitis, tendonitis, peritendinitis, ankylosing spondylitis, epicondylitis, sciatica, coccydynia, sciatica, lumbago, torticollis, ganglion cyst, exostosis, fasciitis, foot disease, bursitis due to hard callus, spurs, stiffness of the big toe .
- Asthma, status asthmaticus, hay fever, allergic bronchitis, allergic rhinitis, drug allergies, serum sickness, reactions to insect bites.
- Atopic dermatitis (coin-shaped eczema), neurodermatitis, contact dermatitis, severe solar dermatitis, urticaria, lichen planus, insulin lipodystrophy, alopecia areata, discoid erythematous lupus, psoriasis, keloid scars, pemphigus vulgaris, herpetic dermatitis, cystic acne.
- Systemic erythematous lupus, scleroderma, dermatomyositis, periarteritis nodosa.
- Palliative therapy of leukemia and lymphomas in adults; acute leukemia in children.
- Adrenogenital syndrome, ulcerative colitis, regional ileitis, sprue; pathological changes in the blood requiring corticosteroid therapy, nephritis, nephrotic syndrome.
- Primary and secondary insufficiency of the adrenal cortex (with mandatory simultaneous administration of mineralocorticoids).
Our doctors
- LITVINENKO Andrey Sergeevich
Traumatologist orthopedist Sports medicine doctor Experience: 19 yearsSign up
- SKRYPOVA Irina Viktorovna
Physiotherapist rehabilitator Experience: 20 yearsSign up
- MOISEENKO Alexey Yurievich
Traumatologist orthopedist Sports medicine doctor Experience: 17 yearsSign up
- KHOLIKOV Timur Vyacheslavovich
Traumatologist orthopedist Sports medicine doctor Experience: 19 yearsSign up
Overdose of the drug Diprospan, symptoms and treatment
Symptoms An acute overdose of betamethasone is not life-threatening. Administration of GCS for several days in high doses does not lead to undesirable consequences (except for cases of use in very high doses or in case of use for diabetes mellitus, glaucoma, exacerbation of erosive and ulcerative lesions of the gastrointestinal tract, or in patients who are simultaneously receiving therapy with digitalis preparations, indirect anticoagulants or potassium-sparing diuretics). Treatment. Careful monitoring of the patient's condition is necessary. Optimal fluid intake and control of electrolyte levels in blood plasma and urine, primarily the balance of sodium and potassium, are shown. If an imbalance of these ions is detected, appropriate therapy must be carried out.
Why do they contact us?
- No queues
No need to wait, we work by appointment
- All in one day
Doctor's appointment, diagnosis and treatment on the day of treatment
- Let's relieve the pain
We will help you relieve pain in just 1-2 visits to us
- We guarantee
Professional approach, affordable prices and quality
- Doctor's appointment 0 RUB!
During course treatment all consultations are free
- Three treatment options
We will select several options and offer optimal treatment
Interactions of the drug Diprospan
The simultaneous administration of phenobarbital, rifampicin, phenytoin or ephedrine may increase the metabolism of the drug, thereby reducing its therapeutic effectiveness. With the combined use of GCS and estrogens, dose adjustment of the drug may be required (due to the possibility of overdose). The simultaneous use of Diprospan with diuretics, which promotes the excretion of potassium, increases the likelihood of developing hypokalemia. The combined use of GCS and cardiac glycosides increases the risk of arrhythmia or digitalis intoxication (due to hypokalemia). Diprospan may enhance potassium excretion caused by amphotericin-B. Concomitant use of Diprospan and indirect anticoagulants may lead to changes in blood clotting, which may require dose adjustment. With the combined use of GCS with NSAIDs or ethanol, it is possible to increase the incidence or severity of erosive and ulcerative lesions of the gastrointestinal tract. With simultaneous use, GCS can reduce the concentration of salicylates in the blood plasma. The combined administration of GCS and somatropin may slow down the absorption of the latter.
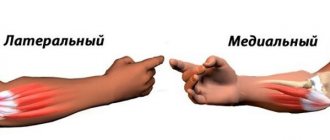
Surgical treatment of medial epicondylitis
Sometimes conservative treatment of ulnar epicondylitis is not able to rid a person of the disease, or at least reduce the pain. In these cases, surgery is performed.
During the operation, the surgeon accesses the tendon part of the forearm flexor muscles in the projection of their attachment to the medial epicondyle. The operation is performed under local or general anesthesia and a pneumatic tourniquet on the humerus in order to prevent even the slightest bleeding. Otherwise, it will be impossible to distinguish healthy tendon tissue from scar tissue. It is this scar tissue that the surgeon must carefully remove.
In some cases, removing scar tissue alone is not enough to achieve a cure. Therefore, they resort to the “tendon release” operation.
The tendon is cut from its insertion on the medial epicondyle. Scar tissue is separated from healthy tendon fibers, and areas of tendon calcification (calcium deposits) are removed. Next, the tendon is sutured to the fascia of a nearby muscle (fascia is the tissue covering muscles and organs throughout the body).
The operation is performed on an outpatient basis, which means that you do not have to stay in the hospital, but go home 30 minutes after the operation.
Instructions for use DIPROSPAN® (DIPROSPAN)
Diprospan® is administered intramuscularly (if systemic entry of GCS into the body is necessary) and directly into the affected soft tissues, for intra-articular, periarticular, intrasynovial, intradermal and intralesional administration.
The dosage regimen and route of administration are set individually, depending on the indications, severity of the disease and the patient’s response to treatment. The drug should be used in the minimum dose and for the shortest possible period.
The dose should be adjusted to obtain a satisfactory clinical effect. If a satisfactory clinical effect does not appear after a certain period of time, treatment with Diprospan® should be discontinued and other therapy should be started.
IM injection
For systemic therapy, the initial dose of Diprospan® in most cases is 1-2 ml. The administration is repeated if necessary, depending on the patient’s condition. The drug is injected deep intramuscularly into the gluteal region.
In severe conditions (systemic lupus erythematosus and status asthmaticus),
requiring emergency treatment, the initial dose of the drug may be 2 ml.
For dermatological diseases
the dose is usually 1 ml.
For diseases of the respiratory system
The effect of the drug begins within a few hours after the intramuscular injection of Diprospan®.
For bronchial asthma, hay fever, allergic bronchitis and allergic rhinitis
a significant improvement in the condition is achieved after administration in a dose of 1-2 ml.
For acute and chronic bursitis
the initial dose for intramuscular administration is 1-2 ml. If necessary, carry out several repeated injections.
Local administration
When administered locally, simultaneous use of a local anesthetic drug is necessary only in isolated cases. If simultaneous administration of a local anesthetic drug is desired, then use a 1% or 2% solution of procaine hydrochloride or lidocaine using dosage forms that do not contain parabens. The use of anesthetics that contain methylparaben, propylparaben, phenol and other similar substances is not permitted.
When using an anesthetic in combination with the drug Diprospan®, first draw the required dose of the drug into a syringe from the bottle, then draw the required amount of local anesthetic from the ampoule into the same syringe and shake for a short period of time.
For acute bursitis
(subdeltoid, subscapularis, ulnar and prepatellar) the introduction of 1-2 ml of Diprospan® into the synovial bursa can relieve pain and completely restore mobility within several hours.
For the treatment of chronic bursitis
the drug is used in smaller doses after stopping an acute attack of the disease.
For acute tendosynovitis, tendonitis and peritendinitis
one injection of the drug Diprospan® alleviates the patient’s condition; for
chronic conditions
the injection of the drug should be repeated depending on the reaction. It is necessary to avoid injecting the drug directly into the tendon.
For rheumatoid arthritis and osteoarthritis
intra-articular administration of the drug in a dose of 0.5-2 ml reduces pain, tenderness and stiffness of the joints within 2-4 hours after administration. The duration of the therapeutic effect of the drug varies significantly and can be 4 weeks or more.
Recommended doses of the drug when administered to large joints
make up 1-2 ml;
medium -
0.5-1 ml;
in small ones
- 0.25-0.5 ml.
For some skin diseases
the drug is administered intradermally directly into the lesion at a dose of 0.2 ml/cm2. The lesion site is evenly pricked using a tuberculin syringe and a needle, which has a diameter of approximately 0.9 mm. The total dose of the drug administered to all injection sites within 1 week should not exceed 1 ml.
Recommended single doses of Diprospan® (with intervals between injections of 1 week) for hard calluses are 0.25-0.5 ml (usually 2 injections are effective); with a spur - 0.5 ml; for stiffness of the big toe - 0.5 ml; for a synovial cyst - from 0.25 to 0.5 ml; for tenosynovitis - 0.5 ml; for acute gouty arthritis - from 0.5 to 1 ml. For administration, it is recommended to use a tuberculin syringe with a needle that has a diameter of approximately 1 mm.
After achieving a therapeutic effect, the maintenance dose is selected by gradually reducing the initial dose by reducing the concentration of betamethasone in the solution, which is administered at appropriate time intervals. The dose reduction is continued until the minimum effective dose is reached.
If a stressful situation occurs or is threatened (which is not related to the disease), an increase in the dose of the drug may be required.
Discontinuation of the drug after long-term therapy should be carried out by gradually reducing the dose. The patient's condition is monitored for at least a year after completion of long-term therapy or after using the drug in high doses.