Infectious arthritis
Infectious arthritis caused by nonspecific microflora (staphylococci, streptococci, Pseudomonas aeruginosa, etc.) have an acute onset with pronounced local and general manifestations. Local signs of purulent arthritis include sharp pain at rest, with palpation, active and passive movements; increasing swelling, changes in the contours of the joint; local redness and increased skin temperature. The consequence of a purulent-inflammatory reaction is a dysfunction of the limb, which takes a forced position. In most cases, with acute infectious arthritis, general symptoms develop - fever, chills, myalgia, sweating, weakness; in children - nausea and vomiting.
Septic arthritis usually occurs in the form of monoarthritis of the knee, hip or ankle joint. Polyarthritis usually develops in individuals receiving immunosuppressive therapy or suffering from articular pathology. In drug-dependent patients, damage to the joints of the axial skeleton is often observed, mainly sacroiliitis. Infectious arthritis caused by Staphylococcus aureus can lead to the destruction of articular cartilage in just 1-2 days. In severe cases of purulent arthritis, the development of osteoarthritis, septic shock and death are possible.
Infectious arthritis of gonococcal etiology is characterized by a skin-articular syndrome (periarthritis-dermatitis), characterized by multiple rashes on the skin and mucous membranes (petechiae, papules, pustules, hemorrhagic vesicles, etc.), migratory arthralgia, and tenosynovitis. In this case, the symptoms of a primary urogenital infection (urethritis, cervicitis) may be erased or completely absent. With gonorrheal arthritis, the joints of the hands, elbow, ankle, and knee joints are most often affected. Typical complications include flat feet and deforming osteoarthritis. Syphilitic arthritis occurs with the development of synovitis of the knee joints, syphilitic osteochondritis and dactylitis (arthritis of the fingers).
Tuberculous arthritis has a chronic destructive course with damage to large (hip, knee, ankle, wrist) joints. Changes in joint tissues develop over several months. The course of the disease is associated with local synovitis and general tuberculosis intoxication. Mobility of the affected joint is limited by pain and muscle contractures. When periarticular tissues are involved in the inflammatory process, “cold” abscesses may occur.
Arthritis associated with brucellosis occurs against the background of symptoms of a general infectious disease: undulating fever, chills, heavy sweats, lymphadenitis, hepato- and splenomegaly. Short-term myalgia and arthralgia, the development of spondylitis and sacroiliitis are characteristic.
Viral arthritis is usually characterized by a short-term course and complete reversibility of the changes occurring, without residual effects. Migrating arthralgia, swelling of the joints, and painful movements are noted. The duration of viral arthritis can range from 2-3 weeks to several months. Fungal arthritis is often combined with mycotic bone lesions. The disease is characterized by a long course and the formation of fistulas. As a result of infectious arthritis of fungal etiology, deforming osteoarthritis or bone ankylosis of the joint may develop.
Bacterial (septic) arthritis
About the article
5806
0
Regular issues of "RMZh" No. 20 dated October 25, 2004 p. 1137
Category: Rheumatology
Author: Belov B.S.
For quotation:
Belov B.S. Bacterial (septic) arthritis. RMJ. 2004;20:1137.
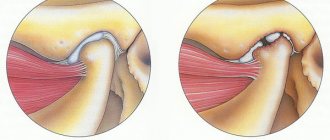
Bacterial (septic) arthritis (BA) is a rapidly progressive pathology caused by direct invasion of the joint by pyogenic microorganisms 1 . The disease occurs everywhere. Mostly children and people over 60 years of age are affected. The annual incidence of asthma is 2–10 cases per 100,000 population, and among patients with rheumatoid arthritis (RA) and recipients of valve prostheses, these values reach 30–70 per 100,000. Despite the extensive arsenal of antimicrobial agents developed and introduced into clinical practice and intensive development surgical technology, irreversible loss of joint function develops in 25–50% of patients. The incidence of deaths from asthma has not changed significantly over the past 25 years and is 5–15% [1]. Etiology Theoretically, all known bacteria can cause AD (Table 1). The most common etiological agent of asthma is S. aureus, which accounts for up to 80% of cases of joint infections in patients with RA and diabetes mellitus. This pathogen is also the main one in infectious coxitis and polyarticular variants of asthma. In second place in the frequency of isolation in patients with asthma are streptococci (primarily β-hemolytic streptococcus of group A), which, as a rule, are associated with underlying autoimmune diseases, chronic skin infection and previous trauma. The occurrence of S. pneumoniae as a causative agent of asthma has decreased significantly in recent years. Streptococci of other groups (B, G, C and F - in descending order) are isolated from asthma in patients with immune deficiency, malignant neoplasms, as well as infectious pathologies of the digestive and urogenital tract. Gram-negative bacilli are the cause of asthma in elderly patients, drug addicts who inject drugs intravenously, as well as in patients with immunodeficiency. Anaerobes as causative agents of asthma are more often found in recipients of joint prostheses, people with deep infections of soft tissues and patients with diabetes mellitus. The most significant etiological agents of asthma among children are S. aureus and Str. pyogenes. The role of H. influenzae, previously quite common in asthma in children, has significantly decreased in recent years due to the widespread introduction of a specific vaccine. At the same time, a number of researchers have noted an increase in the incidence of the gram-negative bacillus K. kingae in asthma, which is a normal inhabitant of the oral cavity in children under 2 years of age [6]. Table 2 summarizes data on the most common pathogens of asthma depending on the categories of patients. Pathogenesis Normally, articular tissues are sterile, which is ensured by the successful functioning of phagocytes of the synovial membrane and synovial fluid (SF). For the development of asthma, the presence of a number of “risk factors” is necessary, depending both on the state of the macroorganism (primarily anti-infective immunity and joint status) and the pathogenic microbe (virulence, exposure, inoculum volume, etc.). The main factors predisposing to the development of asthma are presented in Table 3. One of the most significant aspects of the occurrence of asthma is the weakening of the natural defenses of the macroorganism, due to concomitant diseases, immunosuppression, and the age of the patients. Of no small importance is the background articular pathology, the therapy performed, as well as possible complications of the latter. In particular, in RA, the likelihood of asthma increases due to the prescription of glucocorticosteroids (including intra-articular), cytotoxic immunosuppressants, as well as monoclonal antibodies to tumor necrosis factor - ? (infliximab). Penetration of the pathogen into the joint can occur in several ways. 1. Hematogenous dissemination with transient or persistent bacteremia, as a consequence of distant primary foci of infection (pneumonia, pyelonephritis, pyoderma, etc.). 2. Lymphogenic spread from foci of infection close to the joint. 3. Iatrogenic route during arthrocentesis or arthroscopy. 4. Penetrating injuries caused by plant thorns and other contaminated objects. Invasion of the bacterium into the joint is accompanied by an active inflammatory cellular response and the release of cells involved in inflammation into the joint cavity. Subsequently, under the influence of bacterial waste products, the immune response is stimulated and various inflammatory mediators are released. The accumulation of pro-inflammatory cytokines and phagocyte autolysis products – proteases – entails inhibition of cartilage synthesis and its degradation, followed by destruction of cartilage and bone tissue and the formation of bone ankylosis. Clinical picture As a rule, asthma is characterized by an acute onset with intense pain, swelling, skin hyperemia and hyperthermia of the affected joint. In most cases (60–80%) there is fever. However, body temperature can be low-grade and even normal, which is more common with damage to the hip and sacroiliac joints, against the background of active anti-inflammatory therapy for the underlying disease, as well as in elderly patients. In 80–90% of cases, a single joint is affected (usually the knee or hip) (Fig. 1). The development of an infectious process in the joints of the hands is mainly of traumatic origin (penetrating puncture wounds or bites). The oligo- or polyarticular type of lesion is more often observed with the development of asthma in patients with RA, systemic lesions of connective tissue, as well as in drug addicts who inject drugs intravenously. In addition, in “intravenous” drug addicts, asthma is characterized by a slower onset, a long course and frequent damage to the syndesmosis of the body (sacroiliac and sternoclavicular joints, pubic fusion). In young children, the only manifestation of bacterial coxitis may be sharp pain when moving with fixation of the hip joint in a position of flexion and external rotation. Unlike gonococcal arthritis, BA is not characterized by damage to periarticular soft tissues. Diagnostics When analyzing peripheral blood in patients with asthma, leukocytosis is detected with a shift in the leukocyte formula to the left and a significant increase in ESR. The basis for diagnosing BA is a detailed analysis of the fluid obtained by puncture aspiration from the affected joint (in this case, it is necessary to remove the effusion to the maximum extent possible). A definite diagnosis of AD requires identification of bacteria in the SF. It is inoculated on media for aerobic and anaerobic microbes and should be performed immediately after collection (at the patient’s bedside). In order to obtain preliminary information about the pathogen and prescribe empirical antibacterial therapy, Gram staining of smears is necessary, and the effectiveness of the study is increased by preliminary centrifugation of the fluid. The diagnostic efficiency of this technique is 75% and 50% for infection with gram-positive cocci and gram-negative bacilli, respectively. Visually, SF in BA is purulent in nature, grayish-yellow or bloody in color, intensely turbid, thick, with a large amorphous sediment. When counting leukocytes, the level of cytosis often exceeds that in other inflammatory diseases (RA, gouty arthritis, reactive arthritis) and is >50,000/mm 3 , often more than 100,000/mm 3 with a predominance of neutrophils (>85%). SF also has low glucose levels, less than half of serum concentrations, and high levels of lactic acid. Blood cultures for blood culture give positive results in 50% of cases. X-ray of the joint is one of the first-priority diagnostic measures, since it allows one to exclude concomitant osteomyelitis and determine further tactics for examining and treating the patient. However, it should be noted that distinct changes on radiographs in BA (osteoporosis, narrowing of the joint space, marginal erosions) appear approximately 2 weeks from the onset of the disease. The use of radioisotope scanning techniques with technetium, gallium or indium is especially important in cases where the joint under study is located deep in the tissue or is difficult to reach for palpation (hip, sacroiliac). These methods also help to identify changes inherent in AD at early stages of the process, i.e. during the first two days, when there are still no radiological changes. On computed tomograms, destructive changes in bone tissue are detected much earlier than on plain radiographs. This method is most informative for lesions of the sacroiliac and sternoclavicular joints. Magnetic resonance imaging can detect soft tissue swelling and effusion into the joint cavity, as well as osteomyelitis, in the early stages of the disease. Differential diagnosis Differential diagnosis of BA should be carried out with the following diseases manifested by acute monoarthritis: – acute gouty arthritis; – pseudogout; - rheumatoid arthritis; – viral arthritis; – seronegative spondyloarthritis; – Lyme borreliosis. It should be noted that joint infection is one of the few emergency situations in rheumatology that requires rapid diagnosis and intensive treatment, which avoids irreversible structural changes. Therefore, there is a rule - to regard every acute monoarthritis as infectious until proven otherwise. Prosthetic joint infections The incidence of infection of prosthetic joints is 0.5–2%. Among the pathogens, staphylococci (primarily coagulase-negative), streptococci, gram-negative aerobes and anaerobes predominate (Table 4). Early forms of joint prosthesis infections (up to 3 months after implantation) are caused mainly by epidermal staphylococci and develop due to postoperative contamination or due to contact spread from infected skin, subcutaneous tissues, muscles or postoperative hematoma. Late forms occur during infection with other microbes presented in Table 4 and are caused by hematogenous dissemination. The main risk factors for damage to prosthetic joints include: immunodeficiency states, RA, repeated operations on the joint, long-term surgical intervention, prosthetics of superficial joints (elbow, shoulder, ankle). The onset of the disease can be acute or subacute depending on the virulence of the pathogen. Pain appears (95%), fever (43%), swelling of the joint (38%), outflow of purulent discharge through the drainage (32%). This symptomatology, combined with radiographic signs of destruction of bone tissue near the prosthesis, always indicates infection. Distinguishing a surgical skin infection from a purulent lesion of a joint prosthesis often causes great difficulties. The final diagnosis is made by blood tests, examination of aspirate from the cavity of the artificial joint and/or bone biopsy taken near the area where the cement joins the prosthesis. Treatment Treatment of asthma is complex, including antimicrobial and symptomatic therapy, drainage of infected fluid and physical therapy. Antimicrobial therapy is carried out empirically during the first 1–2 days, taking into account the patient’s age, the clinical picture of the disease and the results of a Gram smear study of the liver, and subsequently, taking into account the isolated pathogen and its sensitivity to antibiotics (Tables 5, 6). Antibiotics should be administered predominantly parenterally; their intra-articular use is inappropriate. The lack of positive dynamics after 2 days dictates the need to change the antibiotic. Continued accelerated ESR is an indication for prolongation of treatment, which averages 3–4 weeks. (sometimes up to 6 weeks), but not less than 2 weeks. after the elimination of all signs of the disease. In addition to antimicrobial therapy, analgesics and non-steroidal anti-inflammatory drugs (diclofenac, ketoprofen, etc.) are prescribed. Drainage of the infected joint is carried out (sometimes several times a day) by closed aspiration through a needle. In order to assess the effectiveness of treatment, leukocyte counts, Gram staining and SG cultures are performed each time. Open surgical drainage of the infected joint is carried out in the presence of the following indications [7]: – infection of the hip and, possibly, shoulder joint; – vertebral osteomyelitis, accompanied by compression of the spinal cord; – anatomical features that make drainage of the joint difficult (for example, the sternoclavicular joint); – impossibility of removing pus with closed drainage through a needle due to increased viscosity of the contents or adhesions in the joint cavity; – ineffectiveness of closed aspiration (persistence of the pathogen or lack of reduction in leukocytosis in the synovial fluid); – prosthetic joints; – concomitant osteomyelitis requiring surgical drainage; – arthritis that develops as a result of a foreign body entering the joint cavity; – late start of therapy (more than 7 days). During the first two days, the joint is immobilized. Starting from the 3rd day of illness, passive movements in the joint are performed. Loads and/or active movements in the joint are started after the arthralgia disappears. Treatment of an infected prosthetic joint is carried out as follows: 1. Simultaneous arthroplasty with excision of infected tissue, installation of a new prosthesis and a subsequent 6-week course of antibiotic therapy (vancomycin + amikacin; vancomycin + cefepime/ceftazidime; oxacillin + rifampicin). 2. Excision of prosthetic components, contaminated areas of skin and soft tissue, followed by parenteral antimicrobial therapy for 6 weeks. After this, the joint is reimplanted with continued antibiotic therapy for 5 days. Prevention The likelihood of infection of a prosthetic joint increases significantly during bacteremia that occurs during dental and urological procedures. In this regard, experts from the American Academy of Orthopedic Surgery, the American Dental Association and the American Urological Association have developed antibiotic prophylaxis regimens for individuals at high risk of developing joint prosthetic infection [11,12]. All recipients of joint prostheses are subject to prophylaxis during the first two years after surgery, patients with immunosuppression due to the underlying disease (RA, systemic lupus erythematosus) or drug/radiation therapy, as well as patients with aggravating concomitant pathology (previous infection of the joint prosthesis, hemophilia, HIV -infection, insulin-dependent diabetes type I, malignant neoplasms) when they undergo a number of dental interventions, including tooth extraction, periodontal manipulation, installation of implants, etc. The above categories of patients should also receive prophylaxis for various manipulations associated with a possible violation of the integrity of the mucous membrane of the urinary tract (lithotripsy, endoscopy, transrectal prostate biopsy, etc.) Antimicrobial prophylaxis regimens are presented in Table 7.
References 1. Goldenberg DL. Septic arthritis. Lancet. 1998;351(9097):197–202. 2. Weston VC, Jones AC, Bradbury N, Fawthrop F, Doherty M. Clinical features and outcome of septic arthritis in a single UK Health District 1982–1991. Ann Rheum Dis. 1999; 58(4):214–219. 3. Dubost JJ, Soubrier M, De Champs C, Ristori JM, Bussiere JL, Sauvezie B. No changes in the distribution of organisms responsible for septic arthritis over a 20 year period. Ann Rheum Dis. 2002; 61(3):267–269. 4. Kaandorp CJ, Dinant HJ, van de Laar MA, Moens HJ, Prins AP, Dijkmans BA. Incidence and sources of native and prosthetic joint infection: a community based prospective survey. Ann Rheum Dis. 1997; 56(8): 470–475. 5. Shirtliff ME, Mader JT. Acute septic arthritis. Clin Microbiol Rev. 2002; 15(4): 527–544. 6. Lahmann JD, Lahmann SJ Etiology of septic arthritis in children: an update for the 1990s. Pediatr. Emerg. Care. 1999; 15:40–42. 7. Gilliard WR Bacterial (septic) arthritis. In the book. West S.D. Secrets of rheumatology. /Trans. from English M., St. Petersburg – “Binom Publishing House” – “Nevsky Dialect”, 1999. 331–341. 8. Urban JA, Garvin KL Prosthetic joint infections. Curr. Treat. Opt. Infect. Dis. 2003; 5:309–321. 9. Rao N. Septic arthritis. Curr. Treat. Opt. Infect. Dis. 2002; 4: 279–287. 10. Trampuz A., Steckelberg JM Septic arthritis. Curr. Treat. Opt. Infect. Dis. 2003; 5:337–344. 11. Antibiotic prophylaxis for dental patients with total joint replacements. JADA. 2003; 134:895–898. 12. Antibiotic prophylaxis for urological patients with total joint replacements. J Urology 2003; 169(5):1796–1797.
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Arthritis: acute or chronic
The acute form can occur very suddenly (acutely) or flare up again and again, that is, be chronic.
Arthritis basically has five clearly defined symptoms:
- stiffness of movements;
- severe pain;
- local redness;
- increased temperature (local);
- swelling in the joint area.
Only a doctor can determine the form of the disease. Based on the results obtained during diagnosis, effective treatment is prescribed. The main thing is to consult a doctor in time, because in the early stages of progression the disease is more treatable. In the acute course of the disease, medications can relieve symptoms and prevent chronicity of the pathology.
The most common form of chronic arthritis is rheumatoid arthritis. Mostly, several joints are affected, which is why doctors also talk about “polyarthritis” (i.e. multiple). If the inflammation is limited to only one joint, it is “monoarthritis.” Often, instead of the somewhat cumbersome term “rheumatoid arthritis,” they simply say “rheumatism.”
Establishing diagnosis
To begin with, the doctor collects an anamnesis of the disease and studies the medical history. The specialist takes into account the following symptoms:
- morning joint stiffness that lasts more than an hour after waking up;
- damage to three joints or more;
- arthritis in the joints of the hands, toes and fingers;
- symmetrical inflammation of the joints (on both sides of the body);
- subcutaneous nodes (rheumatic);
- detection of rheumatoid factor (autoantibodies) in blood serum;
- typical changes that appear on an x-ray.
The diagnosis is confirmed if at least four of these seven criteria are present, with the first four criteria having been present for more than 6 weeks.
To determine the degree of arthritis, the doctor will order a complete blood test to determine rheumatic factors and markers of inflammation. Antibodies to certain proteins are also searched for.
Interesting fact! It is not always possible to detect rheumatic factor at the onset of the disease. It is at an early stage that it is detected in the blood of only 50% of patients. However, if it is present, the disease can take a rather severe course.
In addition to blood tests, X-rays also provide information about the nature of damage to joints and bones. Visualization of joint structures is also carried out using ultrasound (ultrasound).
Magnetic resonance imaging may be prescribed. But this procedure is mainly used when it is necessary to examine certain areas of the body, for example, the cervical spine.
Rheumatoid arthritis (rheumatism)
Rheumatism is a chronic condition that occurs in outbreaks and gradually gets worse. In most cases, more than three joints are affected (polyarthritis). If left untreated, the joints can be destroyed, which can lead to significant limitations in mobility.
Attention! Women suffer from rheumatoid arthritis 3 times more often than men. They also get the disease earlier (between ages 55 and 64) than men (often between ages 65 and 75). Children are most often affected (juvenile idiopathic arthritis). Risk factors include, in particular, genetic factors, as well as smoking and being overweight.
Typical symptoms of rheumatoid arthritis
With rheumatoid arthritis, in addition to five symptoms, a specific picture of the disease appears. At first, it is mainly the small joints on the fingers and toes that hurt. They become “stiff”, morning stiffness appears, and every movement is accompanied by pain. During the day, these symptoms subside somewhat, but without treatment they do not disappear completely.
The longer the disease is left untreated, the more joints become inflamed. Tendon sheaths may also be involved in this process. A special characteristic are rheumatic nodes, which often form on the fingers or in the elbow area.
Inflammation also makes itself felt in the deterioration of general well-being:
- weakness and fatigue appear;
- body temperature rises;
- there are night sweats;
- performance is limited and reduced.
Often the inflammatory process spreads to the tendon sheaths, sometimes internal organs and blood vessels. Although all joints of the body can be affected, the most common areas are the hands, hips, knees and toes.
Diagnosis and treatment of infectious arthritis at the Yauza Clinical Hospital
If the development of infectious arthritis is suspected, the patient is referred for an X-ray or ultrasound of the joints. It is also necessary to do a blood test, an immunogram, examine the intra-articular fluid, and swabs from the genital tract are taken for analysis. If the tuberculous nature of arthritis is suspected, a study is carried out to identify foci of tuberculosis.
Acute infectious arthritis is treated in a hospital. The affected limb is immobilized, then the range of movements is gradually increased. If the inflammation is purulent, then sanitation of the joint (washing) can be performed.
Depending on the pathogen, a drug is selected: antibiotics, antifungals, non-steroidal anti-inflammatory drugs.
You can see prices for services
The mechanism of development and causes of rheumatoid arthritis
The onset of the disease is often associated with a viral infection, injury, stress on a particular joint, hormonal imbalance, and renal failure. The joints most susceptible to damage are the knees, feet, wrists and fingers. When exposed to certain factors, the human immune system triggers an erroneous reaction: it mistakes a normal part of the body for a foreign object. As a result, substances begin to be produced that destroy the synovial membrane of the joints.
Currently, the reasons for the overactivity of the immune system leading to RA are unknown. The main suspected causes:
- Genetic factor
. A number of studies have revealed a high percentage probability of RA manifestation in close relatives in several generations. - Infectious agents
. There is reason to believe that the cause of the disease may be its infectious nature. This is most likely the Epstein-Barr virus, which causes rheumatoid manifestations. Other infectious causes may be: rubella virus, cytomegalovirus, mycoplasma, retroviruses, parovirus B19. Viral RA is acute and rarely becomes chronic. - Emotional stress
. There is a version that the development of the disease begins after a serious psychological shock. This explains the fact that women get sick 4 times more often than men.