Physical therapy (physical therapy) is one of the main methods of non-drug treatment of osteoarthritis of the hip joint (coxarthrosis). It helps relieve pain and optimize the functional activity of the affected joint. Exercise therapy is not capable of eliminating degenerative changes, but it can seriously improve the patient’s quality of life.
There are 3 degrees of severity of osteoarthritis of the hip joint (HJ). For each stage, you can use the same exercises, with the difference that in severe cases you need to reduce the intensity of the load and the amplitude of movement.
Therapeutic exercises for coxarthrosis are prescribed by a traumatologist or orthopedist, and an individual exercise program is developed by a physical therapy doctor. He also works with the patient in this direction.
Causes of coxarthritis
The development of hip arthritis can be triggered by a wide range of factors, which include:
- injury to the pelvis, lower extremities, or specifically the hip joint (for example, dislocation or subluxation, fracture of the femoral head);
- congenital or acquired anomalies of the structure of the musculoskeletal system (hip dysplasia, flat feet, rickets, Perthes disease);
- hereditary predisposition (in particular, for rheumatoid and psoriatic arthritis);
- overload of the hip joint (in runners, heavyweights and other professional athletes, as well as overweight people and representatives of “standing” professions);
- diseases of the spine (lordosis, kyphosis, scoliosis and others);
- problems with blood circulation in the hip joint;
- infectious diseases (specific - for example, osteoarticular tuberculosis, brucellosis, borreliosis, gonorrhea, syphilis, hepatitis and general - for example, chlamydia, other genitourinary and intestinal infections, phlegmon, ostiomyelitis, furunculosis, otitis media, tonsillitis, pneumonia);
- hormonal changes and disorders associated with malfunctions of the endocrine system, menopause;
- age-related changes in joints;
- poor nutrition and other factors that cause a deficiency of vitamins and minerals in the body;
- metabolic disorders (diabetes mellitus, gout, hemochromatosis);
- autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus and others);
- alcohol and coffee abuse;
- unfavorable environmental or working conditions;
- frequent hypothermia (general or specifically in the pelvis and lower limbs);
- animal and insect bites;
- diseases of the nervous system, frequent or chronic stress.
Types of coxarthritis
Depending on the symptoms and causes, arthritis of the hip joint is usually classified as follows:
- Rheumatoid arthritis
. This is a systemic disease in which the patient's own immune cells attack his cartilage and bone tissue. In RA, lesions of the hip joint are usually symmetrical (affecting both joints) and are often accompanied by inflammation of other joints. The disease sharply worsens under stress, allergies, overheating or hypothermia, physical and emotional overload. This is a chronic disease that requires lifelong treatment and management. - Reactive arthritis
. Always occurs as a result of infection - acute or chronic (for example, tonsillitis, cystitis, and so on). Most often, reactive arthritis of the hip joint causes ascending urinary tract infections, less often - descending intestinal infections. The causative agents of the disease include: ureaplasma, salmonella, chlamydia, mycoplasma, dysentery bacillus. Reactive arthritis is especially common among boys and men with reduced immunity and a history of recent infections. The acute phase of the disease must be stopped quickly - otherwise it can irreparably destroy the joint or part of it, and also become chronic. - Post-traumatic arthritis
. Injuries can be open or closed, single or repeated. Sports, household, and professional injuries, as well as disorders of the joint and soft tissues caused by surgery, require immediate treatment. This type of disease is the most unpredictable - changes and pain in arthritis of the hip joint due to injury can grow for years, or can progress quickly within 2-3 weeks. - Gouty arthritis
. A chronic form of arthritis associated with the deposition of uric acid salts in the joints. These crystals injure the cartilage lining and soft tissues when moving, causing constant irritation and inflammation. The disease requires lifelong treatment with diet. - Psoriatic arthritis
. It occurs as a secondary inflammatory disease against the background of psoriasis (usually advanced). It affects not only the hip, but also other joints (polyarthritis). - Degenerative-dystrophic arthritis
, which is also called
arthrosis-arthritis
. Appears due to wear and tear of synovial cartilage. In the absence of healthy gliding and shock absorption in the joint, chronic inflammation of the joint capsule occurs, which is accompanied by joint deformation and the appearance of osteophytes (bone outgrowths) that impede movement in the joint. Doctors associate it with disruption of healthy metabolic processes in cartilage tissue, as well as with endocrine pathologies.
Arthritis of the ankle
Arthritis of the ankle
- acute inflammatory disease of the cartilage tissue of the joint, synovial membrane and periarticular bursa. The ankle joint is often affected by arthritis due to very high static or dynamic loads. Most often, arthritis attacks young people, which significantly reduces the quality of life and affects ability to work.
Symptoms appear suddenly and increase rapidly. Walking and bending the foot are accompanied by severe pain, the ankles swell, redness of the skin and a local increase in temperature occur. Due to swelling and pain, it is difficult for a person with arthritis to make any movements in the ankle, their amplitude is sharply limited. General malaise is also possible as a reaction to the inflammatory process: increased body temperature, weakness, aches.
Arthritis of the ankle joint can develop as a result of injury, when the periarticular ligaments and muscles are damaged, and the resulting inflammation spreads to the elements of the joint. In this case, secondary arthritis develops. An equally common cause is a previous infectious disease and an associated decrease in immunity. It also happens that arthritis affects the ankle due to systemic connective tissue diseases or metabolic disorders. Predisposing factors are unbalanced diet, excess weight, bad habits.
Regardless of the cause, arthritis is always an acute process with pronounced symptoms. It’s easy enough to guess by examining the patient and hearing characteristic complaints. The diagnosis is finally confirmed by ultrasound, which detects fluid in the joint and inflammatory changes. In some cases, an MRI may be required.
In case of severe swelling, a fairly common research method is a diagnostic puncture. This is the insertion of a needle into the joint cavity and the collection of intra-articular fluid to study its composition and origin. Despite the diagnostic value of the test, it should be avoided unless absolutely necessary. When a needle is inserted into the joint cavity, additional trauma to the periarticular bursa and synovial membrane occurs; in the future, this can lead to recurrent arthritis. In addition, such a joint is more likely to develop arthritis in the future.
Patients with ankle arthritis usually see a doctor right away. Anti-inflammatory drugs are prescribed as treatment to relieve the severity of the condition, joint swelling and pain. These are drugs familiar to everyone: ibuprofen, diclofenac, meloxicam, ketoprofen. Additionally, pain-relieving injections, blockades, and physiotherapy—ultraviolet irradiation, electrophoresis, and paraffin therapy—may be recommended.
The acute process resolves within a few days, and many people stop treatment as soon as the pain goes away. This is the most common and dangerous mistake! After all, the treatment of arthritis does not end there, but the next, no less important stage begins - rehabilitation. If you do not engage in recovery, acute arthritis can become chronic. This entails not only repeated exacerbations, but also the risk that in the future, arthrosis occurs at the site of arthritis - irreversible damage to the joint.
Therefore, after relief of acute symptoms, it’s time to contact Dr. Bubnovsky’s Center. Regular classes at the Center are the most effective way to treat and prevent the consequences of arthritis. Experienced and highly qualified kinesitherapists work here, using the active recovery technique - kinesitherapy by Dr. Bubnovsky.
Before prescribing treatment, the doctor conducts an examination - a manual examination, special motor tests, myofascial diagnostics, studies MRI images of the joint and determines the required volume and type of loads. Based on this data, suitable sets of exercises and training plans are drawn up for the patient.
For greater safety and effectiveness of rehabilitation, multifunctional Bubnovsky simulators are installed in kinesitherapy rooms. Their design relieves the joint from excessive compression and tension, so performing the exercises is painless and comfortable for the patient.
Patients with ankle arthritis usually see a doctor right away. Anti-inflammatory drugs are prescribed as treatment to relieve the severity of the condition, joint swelling and pain. These are drugs familiar to everyone: ibuprofen, diclofenac, meloxicam, ketoprofen. Additionally, pain-relieving injections, blockades, and physiotherapy—ultraviolet irradiation, electrophoresis, and paraffin therapy—may be recommended.
Proper physical activity stimulates blood flow, lymph outflow and drainage of the joint. Good microcirculation provides nutrition to the articular cartilage, and the gliding of the articular surfaces is restored. In addition, muscles are strengthened and the elasticity of ligaments is improved. This is a good prevention of injuries, and, as a result, arthritis and arthrosis.
Additionally, local cryotherapy is used. As a result, the structure and function of the joint is completely restored without consequences or complications.
Signs of hip arthritis
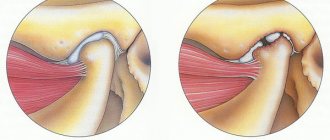
The symptoms of hip arthritis and arthrosis are very similar. To distinguish them, it is important to understand the mechanism of destructive changes in these diseases. With arthrosis, the joint fluid is produced in insufficient quantities, which is why the surface of the synovial cartilage begins to wear off, crack and lose its shock-absorbing properties. Symptoms of hip arthritis are caused by the fact that synovial fluid is produced in excess. This manifests itself in swelling, inflammation, poor blood circulation and nutrition of the cartilage. The type of disease also influences the nature of pain in hip arthritis and arthrosis. With arthrosis, they increase after physical activity, incl. static, dehydration, and with arthritis - at rest, especially in the morning.
It is important to consult a doctor when you notice the first signs of hip arthritis
The “classic” signs of hip arthritis include:
- acute pain when walking, sudden voluntary movements and pulsating, bursting or shooting pain - in a calm state;
- pain from hip arthritis may radiate to the hip, knee, outer thigh, buttock, or groin area;
- stiffness (as if the joint was “covered”), which persists until warm-up, deterioration of mobility in the joint, numbness, regular crunching during sudden movements;
- lameness, careful stepping and other gait disturbances;
- redness and warmth of the skin over the joint;
- muscle weakness (trembling legs, muscle twitching);
- later, noticeable swelling and deformation of the joint appears;
- muscular dystrophy and shortening of the diseased limb are observed in the later stages of the disease or with tuberculous arthritis.
It is impossible to ignore the symptoms and treatment of arthritis of the hip joint - this is fraught with necrotic processes in the bone with destruction of the joint, severe diseases of the knee joints, the load on which increases, and bursitis (inflammatory processes in the synovial bursae).
Why physical therapy is necessary:
- Helps reduce the severity of pain.
- Improves the mobility of the affected joint and prevents the formation of contracture. An individually selected program allows you to develop the hip joint and restore full range of motion.
- Increases the strength of the muscles surrounding the joint. This is a very important point, since the muscles can take on part of the load and provide stability to the joint.
- Speeds up recovery. Physical activity allows you to quickly return to everyday activities, which is important for social rehabilitation.
- Helps correct abnormal movement patterns that further contribute to joint destruction.
In addition, exercise therapy is an important stage of recovery after hip replacement surgery. If the patient, for any reason, is unable to perform the exercises, this is a contraindication to endoprosthetics.
Where to start exercise therapy?
It is better to start physical therapy exercises for coxarthrosis with low-intensity loads:
- Walking. Measured walking at a comfortable pace in the fresh air has a beneficial effect not only on the physical condition, but also on the mood of the patient. For those who have problems with coordination of movements, you can use treadmills in the gym.
- Exercise on an exercise bike. The good thing about an exercise bike is that, firstly, it can be used at home, and secondly, adjusting the load allows you to slowly and gradually increase muscle strength.
- Classes in the pool. Exercises in water allow you to unload the joint and increase the range of motion.
Exercises to strengthen muscles
The exercise therapy complex must necessarily include exercises aimed at increasing muscle strength. This will help reduce stress on the joint and improve balance. Strength loads are performed no more than 2 times a week. The complex is determined by the doctor based on the condition of the affected joint.
Stretching exercises for the hip joint
These exercises are carried out to improve the mobility of the joint and restore the amplitude of its movement. They are usually prescribed for coxarthrosis of stage 2 and higher. It is recommended to do it every day. Such exercises will not only restore range of motion, but also improve the ability to move.
Exercises to coordinate movement and improve balance
Exercises help reduce the risk of falling, give confidence when moving, and also allow you to correct pathological postures that inevitably arise with pain in large joints.
Aerobic exercise
Aerobic exercise, or cardio exercise, is an intense workout that significantly increases your heart rate. Such exercises are useful for increasing cardiovascular tolerance and maintaining overall fitness. Patients with osteoarthritis of the hip joint need to be careful during such activities, especially if the disease is at an advanced stage. As part of your workout, you can use brisk walking, exercise on an exercise bike, or swimming.
Aerobic exercise promotes weight loss, which is very important for patients with coxarthrosis. With a decrease in body weight of only 4%, the severity of pain syndrome decreases by 25%. And reducing weight by more than 20% helps reduce the intensity of pain by half.
Stages of hip arthritis
There are 3 stages of coxarthritis:
- Stage 1
arthritis of the hip joint. There may be no pain; joint ill health can be noticed by minor manifestations - for example, discomfort when moving, crunching, morning stiffness. After warming up, the joint functions normally and does not cause problems during short walking. Discomfort with stage 1 arthritis of the hip joint can completely go away and recur after a long stay in one position, climbing stairs, etc. - Stage 2
arthritis of the hip joint. Pain in the joint appears or intensifies, which persists for a long time. The joint hurts at night and in the morning, which can affect the quality of sleep. With stage 2 arthritis of the hip joint, changes in gait appear (especially with fatigue), and the endurance of the affected limb decreases. Involuntary spasms may occur. Swelling is often observed. - Stage 3
arthritis of the hip joint. The pain plagues the patient almost constantly, and the pain syndrome covers the entire thigh. The range of motion in the joint is severely limited, the muscles become thinner. Lameness caused by inflammation and even shortening of the limb (in every 10th patient) due to joint deformation is noticeable. In this situation, treatment usually requires surgery.
Treatment of hip arthritis
Arthritis of the hip joint is treated comprehensively, and its chronic forms are treated consistently and for life. Treatment of hip arthritis involves pharmacotherapy and physiotherapy, the use of orthopedic devices, and physical therapy. In advanced cases, when drug treatment for hip arthritis does not help, the doctor may prescribe prosthetic surgery.
Drug treatment for hip arthritis
In the treatment of hip arthritis, medications are used to relieve pain, relieve inflammation, improve tissue nutrition, and improve tissue regeneration.
Drug treatment helps relieve inflammation and improve regeneration
Drugs for treating hip arthritis include:
- Nonsteroidal drugs (NSAIDs)
- relieve pain and inflammation. These are nimesulide, paracetamol, meloxicam, ibuprofen, ketoprofen and others. - Steroid (hormonal) drugs
- radically reduce inflammation and pain if NSAIDs are ineffective. These are prednisolone and methylprednisolone, hydrocortisone, mazipredone, triamcinolone. - Cytostatic and immunosuppressive agents
. Although they have primarily an antitumor effect, they are used for rheumatoid arthritis. These are sulfasalazine, metypred, methotrexate, cyclosporine. - Analgesics
. Dexalgin, askofen, indomethacin, movalis are used for pain relief for arthritis of the hip joint. You can also use ointments and gels - Nicoflex, Voltaren, Diclofenac, Fastum-gel and others. - Chondroprotectors
- for better regeneration of cartilage tissue. These are artracam, artracam, alflutop, teraflex, arthra.
In case of infection, drugs for the treatment of arthritis of the hip joint are selected individually for the specific pathogen - this can be rovamycin, cephalosporins and others.
Physiotherapy for hip arthritis
In the early stages of hip arthritis (1st-2nd), physiotherapy plays a major role along with medications. The following methods for treating hip arthritis are most effective:
- phonophoresis;
- electrophoresis;
- ultrasound therapy;
- magnetic therapy;
- shock wave therapy;
- hirudotherapy;
- myostimulation;
- ozone therapy;
- radon and mud baths;
- paraffin applications.
Physiotherapy for hip arthritis is an effective treatment modality
After removing the disease from the acute phase, the following is used to eliminate the symptoms of arthritis of the hip joint:
- manual therapy;
- massage;
- physical therapy (physical therapy for arthritis of the hip joint)
- mechanical traction (stretching) of the joint, muscles and ligaments.
Surgical treatment of hip arthritis
In the treatment of hip arthritis, minimally invasive techniques are predominantly used - for example, puncture (a puncture in which excess fluid is removed from the joint capsule).
In later stages of the disease, synovectomy and endoprosthetics may be required. Synovectomy is a complete or partial excision of the joint membrane, which is performed for autoimmune, infectious and degenerative diseases of the hip joint. If necessary, the lost tissue is replaced with prostheses.
Joint endoprosthetics involves the complete or partial replacement of the head of the hip bone. Often this is the only way to restore mobility to the joint and the patient to be able to move painlessly again. Rehabilitation after surgical treatment of hip arthritis usually takes 3 months, during which time it is necessary to walk on crutches.
Gymnastics for hip arthritis
Gymnastics for arthritis of the hip joint is performed mainly while lying on your back or stomach. At first, it is advisable to supervise the instructor. Here is an example of a short complex of exercise therapy for arthritis of the hip joint, which will help control the disease:
- Stand up straight. Smoothly move your leg in a circular motion without overloading the joint. Repeat 8 times. Then make soft alternating leg swings from the same position.
- Stand up straight and place your hands on a tabletop or other surface. Do a shallow half squat and straighten up. Up to 10 times. Perform exercises for arthritis of the hip joint without sudden movements.
- Stand up straight and smoothly rise on your toes, feeling how your thigh muscles tighten. Gently lower your entire foot.
- Lie on your back with your feet on the floor. Hold your leg under your knee with both hands and try to gradually pull your knee towards your stomach. 7-10 times.
- Lying on your back, bend your knees and place them first to one side and then to the other. 7-10 times.
- In a gentle mode, perform the “bicycle” exercise. Approximately 1 minute, until fatigue appears—gymnastics for arthritis of the hip joint do not need to be done through force.
We wish your joints health!
Images designed by Freepik
If you have osteoarthritis of the hip joints, you must perform special exercises every day. These exercises strengthen the cartilage itself, which requires movement for normal nutrition. Regular exercise therapy should transform from an unpleasant chore into a healthy habit, which is the best way to maintain normal joint function. You need to practice for at least 30–40 minutes. per day, it is better to divide this time into several times for 10–15 minutes. A noticeable effect occurs within 2–3 months. - pain decreases, vitality increases.
Exercises for patients with osteoarthritis of the hip joints
For osteoarthritis of the hip joints, exercises should not be done through pain; it is better to start them after taking painkillers. The intensity of the exercises and frequency of repetitions are determined by the severity of joint pain. Vigorous movements are contraindicated. There are no age restrictions for physical activities. It should be remembered that in addition to the positive emotional charge, physical activity also helps strengthen the cardiovascular system and bone tissue. The range of movements should be increased gradually. The main principle is to repeat the exercises frequently throughout the day for several minutes. Exercises should be performed slowly, smoothly, gradually increasing the range of movements. In this case, it is better to focus on the sore joint, think about how, during movements, blood flows to the joint, bringing with it nutrients that, when the limb relaxes, nourish the cartilage, and during movements are squeezed into the joint cavity, providing good “lubrication” to the joint. For most patients, these exercises will not cause increased joint pain. If, however, significant pain continues more than 20 minutes after performing the exercises, then you need to reduce the number of repetitions to 5 exercises at a time, then gradually increase their number to 15 when your health allows.
Set of exercises No. 1
Lying on your back
- Both legs are bent at the knee joints to the maximum, the feet do not lift off the floor. In this position, the knees are spread apart and brought back again. Try to gradually increase the range of movements. Repeat 10–15 times.
- Exercise "scissors". Legs straightened. One leg lifts off the floor and moves from side to side with the greatest possible amplitude. At the same time, try not to bend your leg at the knee joint. The same is repeated with the other leg. With good training, you can perform movements with both legs at the same time. Repeat 10 times.
- We lift the straightened leg off the floor to the maximum possible height, then lower the leg. Repeat 10 times with one leg, then change legs.
Sitting on a chair
- Try to bend your torso forward and touch your toes with your hands, then straighten up. Repeat 10 times.
standing
- One leg stands on a low stand (step), and we rest our hands on the table. We swing the other leg forward and backward, gradually increasing the amplitude. Later, sideways leg movements are added. Repeat 15 times.
Set of exercises No. 2
standing
- Active flexion at the hip, knee and ankle joints.
- Rolling the ball back and forth with the foot of one foot while the other foot maintains balance.
- Sitting down and getting up from a medicine ball. In this case, friendly training of the muscles of the hip joint is carried out, coordinating the tension of the muscles of the torso and lower extremities.
Lying on your back
- Legs straight. Hands along the body. Flexion and extension of the feet are performed (8–12 times).
- Legs straight. Perform alternating bending of the legs at the hip and knee joints with pulling the knee towards the stomach (8–10 times).
- Legs bent at the knees, hands under the buttocks. Perform alternate leg extensions (legs suspended) at the knee joints at a slow pace (4–8 times).
- "Self-extension." Legs straight. The right (left) arm and left (right) leg are abducted to the sides, stretched behind the arm and heel while inhaling. The foot is in a flexed position.
- Legs straight, shoulder width apart. Internal and external rotation of the feet is performed with tension.
- Legs straight. The straight leg is abducted to the side (4–8 times).
- Legs are bent. Leaning on your feet, raise your pelvis (4–8 times).
- Legs are bent. Feet and knees together. Spread your knees with muscle tension (4–8 times). The feet are in place.
- Repeat “self-stretching”. Legs are bent at the knees. Arms straight. Palms pressed to the floor. Perform head lift (4–8 times).
Lying on your stomach
- Hands under the chin. Alternate extension of the straight legs at the hip joints when the stomach is pressed to the floor (6–8 times).
- Legs bent at the knees (knees shoulder-width apart). The knees are crossed with muscle tension. Hold this position for 2-3 seconds (10-12 times).
- Legs straight. Hands at the shoulders. Pulling the right (left) arm forward and the left (right) leg with the maximum possible amplitude (6–10 times).
Standing at the support
- Walking in place is simulated without lifting your toes (10–12 times).