Most people do not pay attention to the appearance of crunching in the joints. As a rule, during a consultation with a doctor, the patient cannot even remember exactly when the first signs of movement disorders, clicking or cracking in the joints appeared.
It should be remembered that a healthy small or large joint does not make any sounds during loads or movements. If a person hears them, then a pathological process is occurring, which sooner or later will develop into a traumatological or orthopedic disease.
Causes of crunching in joints
The main factor influencing the appearance of extraneous sounds in the joints is the wear and tear of the cartilage tissue that lines the joint capsule. Other causes of crunching include:
- collapse of air bubbles that form in the synovial fluid;
- dehydration – lack of water leads to drying of the joint capsule and excessive friction of the articulation elements;
- intense physical activity without appropriate preparation;
- infectious joint lesions;
- sudden movements in the joints;
- hereditary predisposition;
- period of physiological mobility in joints at the age of 16-18 years.
Why do the joints in my legs click when I walk?
Now let's move on to the most interesting part - why do the joints on the legs click if all the surrounding soft tissues (tendons, ligaments, muscles) are in perfect order? And here there are only two main reasons for the appearance of pathological sound:
- the first reason why the joints on the legs click when walking is a change in the composition, quantity and viscosity of the synovial fluid in the joint capsule;
- the second is the destruction of the cartilaginous synovial layer and exposure of bone tissue.
Both options are associated with serious pathologies occurring in the human body. The intervention of an experienced orthopedist is required to identify the disease and begin its effective treatment.
If the joints on your legs click, you must first eliminate those movements that provoke the appearance of such a sound. There is a popular opinion that if you do the same movement many, many times, during which a click occurs, then the joint will sooner or later develop. It is not true. In reality, nothing like this is observed. If you repeatedly injure the already affected tissues of the joint, you will thereby provoke their even greater destruction.
The only correct solution in a situation where the joints of the legs click when walking is to visit a doctor, and before seeing the doctor, use a fixing orthosis, which will reduce the mechanical load on the damaged tissues.
Crunching in the knee joint
The knee joint may creak for no particular reason. This symptom is not dangerous if there is no pain in the knee and mobility is maintained. Healthy knees have a normal shape and there are no signs of swelling in the surrounding tissues. In this case there is no cause for concern.
Crunching in the knee joint can appear as a symptom when:
- meniscus injuries;
- dislocation of the patella;
- the formation of osteophytes - bone growths inside the joint capsule;
- damage to the cruciate ligaments;
- arthrosis, when worn-out cartilage tissue impedes movement, causing pain, friction and crunching;
- diseases related to metabolism (obesity, gout);
- chondromatosis;
- bursitis.
Cartilage destruction occurs in several stages. Degenerative changes spread throughout the joint, leading to hyperplasia of the synovial membrane and thickening of the joint capsule. In advanced disease, severe deformation of the knee and a predominance of granulation tissue in the joint are determined.
When your knees creak
If your knee joints crunch when walking, then it’s time to take care of them. All their lives they are exposed to serious stress, from the fact that they hold the weight of almost the entire body, ending with overloads during active movements (running, jumping). The knees are one of the most vulnerable parts of the skeleton.
When all the joints of the legs click and crunch, at best, the cause of the pathology lies in wearing incorrectly selected shoes or being overweight. Shoes can be changed and weight can be reduced. It's worse if the problem is salt deposits. Although in this case, at the initial stage, you can still improve your health by adjusting your diet.
If the joint is very crunchy in only one knee, they look for damage to the bones or cartilage tissue. If pain is added to this symptom, the patient is checked for the presence of flat feet or osteophyte. Obesity can also trigger this problem.
In cases where, in addition to the indicated symptoms, swelling appears, you need to make sure that the inflammatory process has not begun. If you miss it, rheumatism, chondromatosis, bursitis or tendonitis may develop over time.
Clicking in the hip joint
Athletes and dancers, people engaged in physical labor, often hear their hip joints crunching. The sound occurs when the tendons come into contact with bone tissue during movement. But the problem also arises from dehydration or excess protein. In such cases, doctors will look for arthritis, arthrosis or other inflammatory processes.
Crunching in the hands
Those who have a habit of cracking their fingers should forget about it as soon as possible. A crunch initially indicates the presence of pathology. If you continue in the same spirit, you can injure the joint or damage the periarticular tissue. Sometimes inflammation even develops. The latter is especially dangerous, since the inflammatory process from the fingers will quickly spread up the arms. The more joints that make the sound, the worse it is.
Crunch in the shoulder joint
Clicks and crunches in the shoulders are a dangerous symptom of a number of pathological changes:
- humeroscapular periarthritis, affecting ligaments, muscles, and synovial bursa;
- tenditis – inflammation of the tendons of the shoulder joint;
- osteoarthritis, characterized by degenerative and dystrophic changes;
- cervical osteochondrosis of II-III degree, increasing static and dynamic tension in the shoulder joints;
- bursitis accompanied by pain;
- arthrosis with the proliferation of osteophytes.
The intensity of the pain syndrome and limitation of mobility depend on the root cause of the crunch in the shoulders and the severity of the disease.
Possible diseases and consequences
If the creaking is a deviation from the norm, it may be a symptom of one of the following diseases:
- arthritis;
- osteoarthritis;
- hip dysplasia;
- gout;
- rheumatism;
- joint instability;
- traumatic injuries (sprains, dislocations, bone fractures, etc.).
As the pathology progresses, complications arise that can cause loss of full motor ability. For example, untreated dysplasia and coxarthrosis can provoke curvature of the hip joint.
Rheumatoid arthritis and deforming gonarthrosis cause curvature of the knee joint. In addition, the patient suffers from constant pain, cases of injury become more frequent, and psycho-emotional stress provokes prolonged depression.
Crunching in the hip joint
Problems with mobility of the hip joint are often accompanied by a characteristic crunching or clicking sound. This symptom appears when:
- mechanical damage;
- arthritis and arthrosis;
- Bekhterev's disease;
- rheumatoid arthritis;
- spondylitis;
- osteoarthritis, which is most severely manifested in the hip joint;
- inflammatory processes – bursitis, tenditis;
- gout;
- endocrine disorders.
At the beginning of pathological changes, the patient notices weakness and stiffness in the morning. Later, a crunch begins to appear when moving in any direction, then the symptom is observed even with minimal mobility without tension. In the future, pain and discomfort occurs, which goes away after the click. Severe joint changes are accompanied by skin hyperemia and soft tissue swelling.
Surgical treatment
Surgical intervention for creaking knees is recommended only in situations where it is not possible to get rid of the problem using conservative methods.
In such a situation, the following is indicated:
- arthrotomy of the knee joint;
- arthroplasty
- punctures to determine the pathology and goal of therapy;
- tenorrhaphy
- meniscectomy
- arthroscopy
- synovectomy
- osteosynthesis
Typically, surgery is performed on patients who have the following problems:
- there is a foreign object in the joint cavity;
- received a fracture;
- you need to replace the knee joint with a prosthesis;
- ligamentous tissue is torn;
- damaged meniscus;
- diagnosed with rheumatoid arthritis that is not amenable to drug therapy;
- Hematomas do not heal well, which requires removal of the pathological contents.
Crunching in joints throughout the body
The appearance of specific sounds in various joints of the body can accompany intense physical activity, sudden weight gain or loss. Changes associated with weight cause transformations in the volume of adipose tissue, fluctuations in homeostasis and intra-articular pressure.
The main causes of crunching in all joints of the body are:
- chondrocalcinosis, in which calcium salts affect cartilage tissue and promote its mineralization;
- osteoarthritis that developed against the background of a hormonal disorder;
- bone tuberculosis;
- Bekhterev's disease;
- rheumatoid arthritis.
Each of these diseases begins asymptomatically. Over time, pathological changes worsen. Lack of timely treatment leads to disability of the patient.
University
→ Home → University → University in the media → “I’m worried about crunching and clicking in the joints, pain in the knees.” Rheumatologists answered readers' questions
How to minimize seasonal rheumatic attacks? What complications are possible after tonsillitis and how to avoid them? What causes pain and aches in joints? What blood test indicators can indicate joint problems? Is it worth visiting a rheumatologist if someone in your family suffers from rheumatoid arthritis? The online conference “Diagnostics and treatment of rheumatic diseases in children and adults” was held on the information portals “Healthy People” (24health.by) and TUT.BY.
The questions were answered:
Irina Dmitrievna Chizhevskaya, chief freelance pediatric cardiorheumatologist of the Ministry of Health, head of the Department of Pediatrics of BelMAPO, Ph.D.;
Natalya Albertovna Martusevich, chief freelance rheumatologist of the Ministry of Health, associate professor of the Department of Cardiology and Internal Diseases of the Belarusian State Medical University, Ph.D.
— At the age of 15, I was diagnosed with chronic tonsillitis. I am worried about crunching and clicking in the joints, pain in the knees. What examinations and how often do I need to undergo?
Irina Chizhevskaya : Knee pain can occur with flat feet. If it is not corrected at an early age, it can cause joint pain and even cause osteoarthritis. Crunching and clicking in the joints is normal for a growing body, if not accompanied by pain. For chronic tonsillitis, you need to visit an ENT doctor twice a year and determine the ASL-O level at least once a year. If it is elevated, then the doctor will then give recommendations.
— A 6-year-old child is diagnosed with reactive arthritis. Compresses and non-steroidal anti-inflammatory drugs (NSAIDs) do not help. What is the reason and how to treat it? The child is often sick.
Irina Chizhevskaya : To understand what the reason is, you need to be tested for pathogens of enterocolitic and urogenital infections, for example yersiniosis, salmonellosis, chlamydia, mycoplasmosis. If positive results are obtained, antibacterial therapy is necessary taking into account the pathogen. Perhaps the dose and duration of treatment with NSAIDs was insufficient. Typically, NSAIDs are prescribed for 3-4 weeks. If symptoms of the disease persist after this course, it may no longer be reactive arthritis. And you need to see a rheumatologist.
My daughter (7 years old) has juvenile rheumatoid arthritis. The disease began in February 2021. Takes the drug intramuscularly once a week. Since May 2021, she has been in remission (this is according to the documents; in fact, the last exacerbation was in September 2017). The attending doctors say that the injections will continue until adolescence. Although they previously said that the drug would be discontinued after 3-4 years of remission. She is having a hard time with the treatment (her hair is falling out, she vomits on the day of the injection). How do you know when to stop taking the drug? The child is in a state of stress due to the injections and their consequences. Is it possible to switch to tablet form? Isn't this dangerous?
Irina Chizhevskaya : There is no consensus in the world when to stop the drug. The general recommendation for the earliest discontinuation is 2 years of stable remission, confirmed by laboratory and radiographic research methods. We can talk about the state of remission only after 6 months after the last exacerbation of the disease. And then we count down the drug remission. After discontinuation of the drug, an exacerbation of the disease is possible, which can occur at different times. If symptoms of the disease return, all therapy should be returned. It has been proven worldwide that subcutaneous administration of the drug is more effective than tablets. But since the child is in remission of the disease and does not tolerate injections well, you can switch to the tablet form. This is not dangerous.
— A daughter with JRA (juvenile rheumatoid arthritis) from twins, is there a risk of the twin sister or older sister getting the disease? Is it possible to somehow prevent the development of the disease? Can healthy sisters get vaccinated?
Irina Chizhevskaya : There is a risk, since JRA has a genetic predisposition. But this does not mean that all family members will have this disease. Among all the children we see with JRA, there are only two familial cases. There is no prevention. Lead a healthy lifestyle and avoid stress. Healthy sisters definitely need to be vaccinated.
My son is 2.5 years old. After an acute respiratory viral infection (there was only a runny nose, no fever), I could not step on my foot in the evening for half an hour, and the next day I could not do so for about 3 hours. No pain was detected upon palpation. This is an isolated case; after the next ARVI, this did not happen again. What could be the reason for this, and what tests need to be done?
Irina Chizhevskaya: It’s difficult to answer unequivocally. But since this was an isolated incident, there is no need to worry. If this happens again, you should consult a rheumatologist.
“Blood biochemistry showed an increase in uric acid”
- I am 36 years old. Blood biochemistry showed an increase in uric acid - 371 (normal 155-357), a year ago it was 365. For the last six months, my right knee has hurt when I squat completely, both knees crunch, my lower back hurts when I walk for a long time. I changed my diet, completely gave up white and red meat, and started drinking more water. A month later I did biochemistry again, uric acid was 247! Is it possible to reduce this indicator with diet and so quickly? Should this kind of nutrition become a way of life? Can the knee be checked using an ultrasound or is an MRI necessary? How often should uric acid levels be monitored? (all other indicators are normal, antistreptolysin - 131, creatinine - 65).
Natalya Martusevich : The diet could reduce the level of uric acid, since it is the end product of protein metabolism. And reducing meat consumption reduces uric acid levels. The level of 371 is not significant from the point of view of assessing the level of uric acid, since even with very serious disorders of purine metabolism, the target level during treatment is the level of 360. 371 - can be regarded as a slight excess only if the analysis is carried out correctly (within three days the patient does not should take meat foods or a lot of protein foods).
Without knowing the concomitant diseases and without seeing the type of constitution, it is impossible to answer the question of whether it is necessary to continue to adhere to this way of eating. For people with a thin build, eating meat, on the contrary, can be a way to improve their well-being. An MRI of the knee is ideal because it will give you information about the condition of the subchondral bone and structural changes in the joints.
On the right is Natalya Martusevich
I am 50 years old. The disease is ankylosing spondylitis, third group of disability. Six years ago I underwent treatment with Remicade. There was a remission for 2 years. After a new exacerbation, the hospital prescribed Humira. After the second injection, an allergic reaction occurred. Humira was discontinued and Enbrel was recommended. We have been purchasing Enbrel in Moscow for about 2 years now with our own money. Helps great. Is it possible to get Enbrel for treatment at the expense of the budget and where to go for it?
Natalya Martusevich: Enbrel or any genetically engineered immunobiological drug can be prescribed to a patient at the expense of the state budget in a situation where he has exhausted all possible methods of treating this disease with standard drugs used for this disease, which have shown ineffectiveness/intolerance. In this case, the patient continues to have high disease activity or has developed life-threatening complications (amyloidosis). The decision is made by a special commission of the Ministry of Health, which is appointed by order of the ministry. The patient is sent to this commission on the recommendation of the chief rheumatologist of the region (Minsk).
I have adult-onset Still's disease. I take Methylprednisolone. The work often involves night shifts. I noticed that I feel worst in the evenings. If you take, in addition to the morning dose (4 mg), a small dose of methylprednisolone (1-2 mg) in the evening, then the next day I feel much better. However, everywhere they write that it is recommended to take Prednisolone only in the morning. Is it possible in my case to take a small dosage at night, at least during night shifts, or should I avoid taking it in the evening and take the entire dose in the morning?
Natalia Martusevich: Despite the fact that the classic dose is as early as possible in the morning, taking a small dose of methylprednisolone at night is possible. At night, you are awake and your biorhythms are shifted, releasing your hormones. Night work is not recommended for patients with Still's disease.
- I am 45 years old. Diagnosis: rheumatoid arthritis. What modern medicine can replace Methotrexate? It doesn’t suit me: the gastrointestinal tract is already weak.
Natalya Martusevich: You can replace it with Sulfasalazine or Leflunamite. The choice of drug is determined by the doctor and depends on the activity of the disease, concomitant pathology, seropositivity/seronegativity of the disease. Before changing methotrexate, it is usually recommended to take it subcutaneously, which has minimal complications in the gastrointestinal tract.
— Should you trust the drug Instaflex (advertised on the Internet) for the treatment of arthritis/arthrosis?
Natalya Martusevich: It’s not worth it, because the information on the Internet about this medicine is fake. If this information is discovered, the Ministry of Antimonopoly Regulation closes the site. Despite this, advertising appears again from time to time.
- I am 53 years old. I have been suffering from chronic glomerulonephritis since 2002. Over the past year, severe pain in the ankle joints and elbows has become more frequent, I regularly take blood tests, they are within normal limits. At the Central District Hospital they diagnosed arthritis of the ankle joints, prescribed melaxipol and electrophoresis, during the procedures the pain subsided, then after a while the pain returned. The central district hospital doesn’t have its own rheumatologist; I live in a small village. What do you advise?
Natalya Martusevich: I would advise you to see a rheumatologist at the regional rheumatology center, since rheumatological care is provided at the regional and republican level.
“After the fracture, all joints began to hurt”
- I am 35 years old. At the age of 30, I broke my leg in several places and had surgeries. As a result, all joints began to hurt very much - from the fingers to the ankle. They ache and twist at any time of year and weather. What doctors and what tests are needed to solve the problem?
Natalya Martusevich: If the fractures occurred as a result of a fall from the height of one’s own body, then it is advisable to perform densitometry of the axial skeleton to clarify bone mineral density. The results of the study will show the feasibility of further examination. In the case of normal bone mineral density, the emphasis should be on a non-drug treatment method (physical therapy, massage, if there are no contraindications, swimming, sanatorium treatment, physiotherapy). Because the pain syndrome is based on a change in the load on the underlying bones, muscles and ligaments.
— Are joint diseases and hereditary hemochromatosis C282Y related? How to support joints, what methods and possibilities of prevention?
Natalya Martusevich: Connected. In patients with hemochromatosis, secondary osteoarthritis develops much earlier (earlier wear of articular cartilage and intervertebral discs). This requires correction of the underlying disease, long-term use of symptomatic slow-acting drugs (chondroitin sulfate, glucosamine sulfate or chloride as monotherapy or in combination with each other. Non-drug methods: exercise therapy, spa treatment, physiotherapy, mainly thermal in the absence of contraindications.
I am 49 years old. A year ago, I started having problems with my knee: it hurts to walk, it’s difficult to bend my leg, if you put your palm on it, you feel that the sore knee is hotter than the healthy one. The scan at the clinic did not show any pathology. The therapist prescribed NSAIDs and told me to take them for life. What additional tests would you recommend and where should I go for additional testing?
Natalya Martusevich: To determine the cause of a problem in the knee joint, the following is needed: a general blood test, a biochemical blood test with mandatory determination of the level of C-reactive protein, a general urine test, an examination by a gynecologist, and an ultrasound of the knee joint. If there are no structural changes in the joint, perform an MRI of the knee joint. Examinations can be performed by a therapist in a clinic; MRI is performed if indicated, usually in a hospital setting.
“Knee pain bothers me in spring and autumn”
— All my muscles hurt, I constantly take painkillers, constantly go to doctors, undergo tests and everything else doesn’t help. Tell me what to do, where to go, tell me possible causes or a presumptive diagnosis. Natalia Alexandrovna, born in 1954
Natalya Martusevich : The causes of muscle pain are varied. They can be caused by problems in the muscles, nervous system, or be the result of side effects of drugs, most often statins (drugs to lower cholesterol). To determine the cause, you need to consult a therapist and carry out the following examinations: determine the level of C-reactive protein, creatine phosphokinase, the level of vitamin D, thyroid-stimulating hormone of the pituitary gland, and a general urine test for inflammatory changes. You should also look into the side effects of the medications you are taking. If there are no changes in the tests, the general practitioner will refer you to a neurologist to rule out a neuropathic cause of the pain syndrome.
— Knee pain bothers me in spring and autumn. Should you visit a rheumatologist? If yes, what examinations do you need to come with? Victoria, 35 years old
Natalya Martusevich: Consultation with a rheumatologist is necessary, since some diseases can begin with joint pain without swelling. It is necessary to perform a general blood test, a biochemical study, C-reactive protein levels, a general urinalysis and an examination by a gynecologist. Before examining a gynecologist, you need to undergo an immunological study and determine ASL-O, antibodies to cyclic citrullinated peptide, RF (rheumatoid factor).
Photo: Healthy People portal
Share
What to do if you have cracking joints?
If you notice the appearance of crunching in your joints, you should monitor your condition. If possible, make notes indicating how, when and with what movements the extraneous sound occurs. Crunching in the joints can occur during bending, rotation, or physical activity. This information will be important for the doctor you need to contact.
For medicinal purposes the following is prescribed:
- correction of the diet with minimal consumption or complete elimination of salt;
- increasing the volume of fluid consumed;
- non-steroidal anti-inflammatory drugs that are taken orally and externally (in the form of ointments, gels, creams);
- chondroprotectors, which improve the quality of hyaline cartilage, prevent their destruction, and promote the regeneration of the inner lining of the joint capsule;
- complexes of minerals and vitamins that help eliminate deficiency conditions, normalize bone mineralization, and restore metabolism;
- preparations based on hyaluronic acid - help restore damaged cartilage, improve the elasticity of osteochondral joints;
- angioprotectors - to improve blood supply to the soft tissues surrounding the joint.
If indicated, it is possible to prescribe corticosteroids and anti-gout drugs that inhibit the synthesis of uric acid and eliminate acute manifestations of gouty arthritis.
People suffering from cracking joints should remember that without adequate physical activity and physiotherapy, taking medications will not lead to the desired result.
Methods of physical therapy and physiotherapy must be used:
- gymnastics that improves motor activity, sprains;
- swimming in the pool;
- exercise on an exercise bike;
- magnetic therapy;
- UHF;
- electrophoresis with anti-inflammatory, painkillers;
- shock wave therapy;
- laser treatment;
- barotherapy;
- mud therapy.
In some cases, the use of orthopedic devices, orthoses, and bandaging the limb with an elastic bandage is recommended.
A well-designed course of therapy helps eliminate inflammatory foci, improve local blood supply and tissue trophism, and relieve pain. Patients are recommended to undergo special therapy at least twice a year to maintain long-term remission.
Gymnastic exercises
Gymnastics helps prevent knee deformation and maintain muscle tone. You can perform the exercises when the doctor has cleared the load on your knees, since otherwise you can further harm your joints.
To get rid of crunching knees, you can do the following exercises:
- Sipping. While we are lying in bed, we stretch our upper and lower limbs.
- Bend your knees. We lie down on the floor face up and alternately bend our knees, and our feet should not leave the floor.
- "Bike". We lie on our backs, bend our knees and twist them, imitating riding a bicycle.
- Rotation. We stand near the chair, leaning on the back with our hands, alternately rotating our knees in one direction and the other. The exercise must be repeated 10 times.
- Squat. We stand near a chair, lean on the back and squat 10 times.
The movements must be slow and smooth, otherwise you can harm your knees. If sharp pain and swelling appear after completing gymnastics, it is better to stop exercising for a while.
Diagnostics
Before prescribing treatment, a traumatologist or orthopedist needs to find out the root cause of the appearance of crunching in small or large joints. For this purpose, hardware types of diagnostics are prescribed:
- Ultrasound of joints;
- MRI;
- CT;
- radiography;
- scintigraphy.
To exclude or confirm the infectious nature of the disease, puncture the affected joint, conduct a laboratory test of blood (clinical and biochemical analysis), and synovial fluid.
Prevention measures
To prevent the appearance of pathological creaking in joints and other unpleasant symptoms, you should take care of prevention. The sooner you start taking care of the health of your musculoskeletal system, the lower the risk of various kinds of problems.
The main preventive measures include:
- Weight control. You should not allow yourself to gain extra pounds, as obesity causes many health problems and significantly increases the load on your joints, accelerating their wear and tear.
- Proper nutrition. A balanced menu prevents weight gain, has a positive effect on health and saturates the body with all the necessary nutrients.
- Drinking enough. Dehydration impairs metabolism and provokes thickening of synovial lubrication in the cavity of the articular joint.
- Moderate physical activity. Playing sports and walking should become an obligatory part of a person’s life, but you still shouldn’t overload your joints.
- Use of prophylactic medications. With the approval of a doctor, chondroprotectors and various vitamin and mineral supplements should be regularly used.
- Timely treatment. Any health problems must be resolved immediately, as they have negative consequences for the entire body.
You can get more information about the problem of creaking in joints and methods for solving it by watching the video in this article.
Treatment of cracking joints
At the Center for Restorative Medicine in Naberezhnye Chelny, an experienced orthopedist treats cracking joints of various origins. You can read more about the specialist at the link.
The clinic’s specialists use a comprehensive, systematic approach to the treatment of joint pathologies. The medication program is compiled individually for each patient. Modern physiotherapeutic procedures are widely used, which can be found here. Various massage techniques described here are used specifically to restore elasticity and mobility of joints. Prices for all services provided at the clinic are indicated on the page.
If crunching occurs in the joints, it is important to consult a doctor in time and prevent the development of severe pathologies that threaten limited mobility and disability.
Do not ignore the first symptoms, call the Center for Restorative Medicine by phone and sign up for a consultation.
What to do?
If the joint crunches from time to time, but there are no other symptoms, the function is completely preserved, then nothing needs to be done. It is enough to calm down, not perceive the crunch as a symptom of illness and not pay attention to it. The appearance of clicking sounds during exercise is not a cause for concern and is not a symptom of incipient arthrosis.
If pain comes along with the crunching, treatment is required. It can be completely different, depending on the origin of the pathological process. Most often, conservative therapy is sufficient. The patient is prescribed:
The main ways to eliminate pathological crunching
When an inflammatory or degenerative-dystrophic pathology is diagnosed, treatment begins immediately. If the crunch is accompanied by mild pain or no discomfort occurs at all, then the prognosis for a full recovery is favorable. The only exceptions are autoimmune diseases (gout, psoriatic and rheumatoid arthritis), which cannot yet be fully restored. Their therapy uses basic biological drugs, agents for dissolving and removing uric acid crystals from the body. The functional activity of the ankle is increased with medications for local application:
- ointments with non-steroidal anti-inflammatory components (nimesulide, diclofenac, ketoprofen, ibuprofen, indomethacin). Drugs with powerful anti-inflammatory, anti-exudative, analgesic effects stimulate the production of synovial fluid, which serves as a kind of shock absorber for bone surfaces;
- ointments with a warming effect: Finalgon, Capsicam, Viprosal, Apizartron, Nayatox. Used only after relief of inflammation to improve blood circulation in the ankle. The active ingredients of external products eliminate the deficiency of nutrients and biologically active substances, stimulate the regeneration of damaged ligaments.
Therapeutic regimens for any pathology of the musculoskeletal system necessarily include chondroprotectors with chondroitin, glucosamine, hyaluronic acid, and collagen. These are Teraflex, Artra, Dona, Structum, Chondroxide. It is useful to take such drugs to eliminate crunching that occurs for both pathological and natural reasons. Their ingredients accelerate the restoration of damaged tissues and prevent the development or progression of existing diseases.
Why is arthritis of the ankle and foot dangerous?
The disease is dangerous because it often goes unnoticed and leads to a complete loss of joint function, that is, the person becomes disabled. Acute purulent complications of ankle arthritis are also dangerous.
Arthritis of the foot and ankle begins gradually, unnoticeably
Stages
There are several stages of disease development. The inflammatory process develops gradually, turning into a degenerative-dystrophic one:
- Early – inflammation
. The synovial membrane swells, and inflammatory exudate appears in the joint cavity. Pain is moderate, swelling and redness are absent or only slightly expressed. - Explicit – inflammatory-proliferative process
. The synovial membrane increases in volume, erosions appear on the cartilage, and soft granulations of connective tissue grow in the articular cavity (the process of proliferation - growth). The inflammatory process intensifies. Externally, this is manifested by increased swelling, redness and pain. - Progressive - mild ankylosis
. The cartilage is destroyed, soft granulations turn into dense connective tissue that grows in the joint cavity. Bone growths appear. The joint gradually loses its mobility. Pain, swelling and redness continue to bother you constantly or during exacerbations. - Advanced - complete immobility (bone ankylosis).
There is no cartilage tissue, bone growths connect the articular surfaces of the ankle, which eliminates movement in the ankle and foot (ankylosis of the ankle). The pain is constant, arthritis of the foot develops with limitation of its function.
Possible complications
If ankle arthritis is left untreated or treated independently with home remedies, the following complications may develop:
- purulent processes - abscesses, phlegmon, sepsis;
- subluxations and dislocations of the ankle;
- development of foot arthritis;
- immobility of the ankle and inability to move without assistive devices.
Frequently asked questions about the disease
I dance professionally, but recently my ankle joint has started to hurt on one side. Which doctor should I see?
You can start with a traumatologist. If necessary, he will refer you to another specialist.
Do you join the army if you have ankle arthritis?
If there is persistent impairment of articular function, do not take it.
Patients are often interested in how to treat arthritis of the joints of the foot and ankle. This is the wrong approach. You need to look not for a cure for this disease, but for a clinic that will help you cope with it. The Moscow Paramita clinic has everything necessary to help any patient with ankle arthritis. Contact us, you won’t regret it!
Literature:
- Grazhdanov K.A., Barabash A.P., Barabash Yu.A., Kauts O.A., Zuev P.P. Technology of treatment of purulent arthritis of the ankle joint // Modern problems of science and education. – 2021. – No. 3.
- Martinovich AB, Infected injuries and post-traumatic deformities of the ankle joint. // Diss. Candidate of Medical Sciences Minsk 1990. - P. 128.
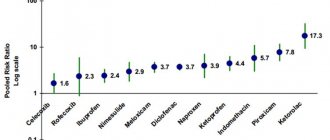
- Perez Busquier M., Calero E., Rodriguez M. et al. Comparison of aceclofenac with piroxicam in the treatment of osteoarthritis. Clin Rheumatol 1997;16(2):154–9.
- Kornasoff D., Frerick H., Bowdler J. et al. Aceclofenac is a well-tolerated alternative to naproxen in the treatment of osteoarthritis. Clin Rheumatol 1997;16(1):32–8.
Themes
Arthritis, Joints, Pain, Treatment without surgery Date of publication: 12/14/2020 Date of update: 04/03/2021
Reader rating
Rating: 4.71 / 5 (7)
How to deal with natural crunching
If no pathologies are identified in a child with a crunching ankle, then no treatment is required. The condition of the joint will normalize over time, and sound phenomena will no longer accompany all movements of a small child or teenager. Pediatricians recommend enriching the diet with fresh vegetables and fruits, which contain a high concentration of substances necessary for the formation of the skeleton. To improve the functioning of all joints, doctors prescribe balanced complexes of vitamins and microelements: Supradin, Alphabet, Complivit, Vitrum, Selmevit, Multitabs. For babies from 12 months, Pikovit is available in the form of a sweet syrup.
It’s a completely different matter if the ankle joint in adults cracks for natural reasons. This causes not so much physical as psychological discomfort, especially when in public places. One of the effective ways to eliminate it is the use of systemic or local drugs, dietary supplements with chondroprotectors. How to be treated without using medications:
- massage. To eliminate crepitus, various massage techniques are used, since they all improve the condition and functioning of the ankle. The greatest therapeutic effectiveness of massage is typical for classic, acupressure, cupping, and Swedish. During and after treatment procedures, blood circulation in the joint cavity accelerates, preventing the accumulation of carbon dioxide;
Ankle massage.
- correction of diet. The more a person weighs, the more often crackling sounds are heard when walking. But even in people with low weight, movements are often accompanied by crunching. Especially for girls and women who follow a diet and exclude foods with carbohydrates and fats from the daily menu. The diet should be balanced, containing all the necessary nutrients;
- drinking regime. When the ankle is “exploited,” harmful salts, tissue breakdown products, and toxins accumulate in its cavity. Slagging of the joint can lead to crepitus due to impaired trophism. Therefore, orthopedists recommend drinking at least 2-2.5 liters of fluid daily. Drinks with a mild diuretic effect help cleanse the joint cavity. These are berry fruit drinks, fruit compotes, vegetable juices, non-carbonated lightly salted mineral waters.
Another good way to get rid of crunching is an active lifestyle. For people over 50 years old, physical therapy doctors recommend yoga, swimming, long walks in the fresh air, physical therapy or gymnastics. You should avoid only those sports that can lead to serious injuries - skiing, hockey, football. There are no such restrictions for young people. Any kind of sport except weight lifting is suitable for them.