An inflammatory process that affects one or more joints is called arthritis.
It has several varieties, differing in causes, symptoms and treatment. The rheumatoid form of the disease can appear at any age, but most often affects people over 30 years of age. It has been noted that the proportion of women among the sick is over 70%. The disease causes destruction of the synovial membrane of the joint, cartilage, and bone. In its chronic form, the disease causes pain for many years and interferes with leading a full life. Over time, the degree of damage to the knee joint will only increase, so treatment should begin as early as possible.
Symptoms of rheumatoid arthritis of the knee joint
Characteristic manifestations of the disease can be detected without the use of special diagnostic equipment:
- decreased mobility of the knee, which manifests itself at the initial stage of the disease only after an overnight rest;
- sharp or aching pain that intensifies with movement; may spread to the entire leg;
- inflammation, signs of which are swelling of the knee, local changes in body temperature;
- effusion in the affected area;
- fever;
- increased fatigue.
As the disease progresses, the symptoms of rheumatoid arthrosis of the knee joint will intensify, and its deformation will be visible even to a non-specialist. Start treatment without waiting for the problem to become disabling! At the initial stage, the destruction of the knee can still be stopped.
Symptoms
Signs of rheumatoid arthritis appear approximately 1-2 weeks after illness caused by acute streptococcal infection. Rheumatitis of the extremities is just one of the syndromes inherent in rheumatism. In the acute course of this disease, the following pathological conditions are possible:
- rheumatoid arthritis (inflammation of the joints);
- rheumatic carditis (inflammation of heart tissue);
- rheumatic chorea (damage to the nervous system);
- skin lesions (erythema, rheumatic nodes);
- rheumatic pleurisy (inflammation of the lining of the lungs).
Rheumatoid arthritis affects mainly the large joints of the extremities (elbows, knees and ankles), and somewhat less commonly it affects the small joints of the hands and feet. Since rheumatoid arthritis is a syndrome of post-streptococcal infection, the patient feels general weakness, shortness of breath, and body temperature rises to 38-39 °C.
A distinctive feature of rheumatoid arthritis is symmetrical damage to the joints, and it is benign in nature, that is, it does not lead to joint deformation. The patient feels pain in the joints, their mobility is lost, swelling and redness of the skin in areas of inflammation are possible.
Causes of rheumatoid arthritis of the knee joint
Absolutely anyone can get sick, regardless of gender, age, or lifestyle. Rheumatoid arthritis is caused by a combination of several factors:
- hormonal disorders - this is why women of puberty usually become ill;
- injuries, as well as unsuccessful operations or incorrect rehabilitation after them;
- hypothermia of the body;
- smoking;
- infectious diseases;
- allergy.
The bulk of officially registered patients are men and women aged 25 to 55 years.
Stages of rheumatoid arthritis of the knee joint
The disease develops gradually, so at first a person does not attach much importance to minor health problems. The course of the disease can be divided into 2 stages:
- Initial, when the victim is plagued by minor pain, and in the morning the knee joint is inactive. After a few hours, the victim forgets about the illness - exactly until its new manifestations.
- Transition to the stage of rheumatoid polyarthritis, which usually manifests itself symmetrically on the left and right limbs. The pain does not stop, and difficulties with movement appear.
Arthritis in severe cases is no longer just mild pain or inflammation. Destruction can affect muscles, affect the liver, heart, lungs and other internal organs. In this case, the patient’s life is at risk. The risk of disability increases.
Diagnosis of rheumatoid arthritis of the knee joint
The doctor, in addition to visually examining the patient and interviewing him, uses hardware diagnostic tools for rheumatoid arthritis. First of all, a blood test is performed to help detect signs of the disease, which include:
- increase in ESR;
- low hemoglobin levels and a decrease in the number of red blood cells (anemia);
- The level of C-reactive protein in the blood is higher than normal.
In addition to blood composition, the following are examined:
- X-ray of the knee, as well as the results of an ultrasound examination (ultrasound).
- Intra-articular fluid. If the diagnosis is confirmed, it has a reduced density, low transparency, and a high number of individual blood cells - neutrophils, leukocytes and others.
- Urine for the presence of protein.
- Test for the presence of antibodies to immunoglobulins. With a 70% chance of rheumatism it will be positive.
- Serum creatinine and urea levels.
If several symptoms of the disease have been identified, the doctor may prescribe an additional examination, based on the results of which treatment is prescribed. The first signs that attract attention are:
- nodules characteristic of rheumatism;
- positive result of rheumatoid testing;
- manifestation of arthritis in other joints (hands, etc.);
- joint deformation - visible visually or using x-ray examination;
- stiffness of movements.
Rheumatism in children: current state of the problem
Rheumatism , or acute rheumatic fever
according to the International Classification of Diseases (ICD), is a systemic inflammatory disease of connective tissue with a predominant localization of the process in the cardiovascular system, developing in connection with acute streptococcal infection in persons predisposed to it, mainly at the age of 7–15 years. While not a widespread disease, rheumatism nevertheless represents a serious problem in cardiorheumatology due to the frequent formation of heart defects and the development of temporary and permanent disability. In accordance with ICD-10, acute rheumatic fever is classified as a disease of the circulatory system (class IX) under the codes:
100 – Rheumatic fever without mention of cardiac involvement;
101 – Rheumatic fever with cardiac involvement;
102 – Rheumatic chorea.
Rheumatism was known already in the 5th century BC. Hippocrates in his work “The Four Books of Diseases” wrote: “With arthritis, fever appears, acute pain seizes all the joints of the body, and these pains are sometimes sharper, sometimes weaker, affecting first one or the other joint.” In ancient times, doctors believed that inflammation in the joints was caused by some toxic liquid spreading throughout the body. This is where the name of the disease came from - “rheumatism” (from the Greek “rheum” - flow). Damage to the cardiovascular system was considered a complication of articular syndrome. Only after the publication of the outstanding works of the French doctor Buyot (1836) and the Russian doctor I.G. Sokolsky (1838), rheumatism was identified as an independent disease involving heart damage.
Over more than a century and a half of studying this serious, often disabling disease, the connection between its development and streptococcal infection has been determined, and a system of diagnosis, treatment and prevention has been developed and implemented. This contributed to a widespread decline in the incidence of rheumatism by the middle of the twentieth century. However, in recent years, due to a number of negative socio-economic processes, there has been a tendency towards an increase in the incidence of rheumatism in all age groups, and more intensely in children
. This trend is also due to the presence of secular rhythms characteristic of aggressive streptococcal infections and a decrease in the sensitivity of streptococci to penicillins. The study of the dynamics of the epidemic process shows that in the last decade, streptococcal infection has appeared and is growing, which is an analogue of that of past times, which can contribute to the increase and severity of rheumatism. Therefore, in the future, the problem of rheumatism will not lose its relevance.
Etiology and pathogenesis
The development of rheumatism is closely related to a previous acute or chronic nasopharyngeal infection caused by group A beta-hemolytic streptococcus
.
A special role is given to M protein
, which is part of the streptococcal cell wall. Of the more than 80 known varieties of M protein, M-5, M-6, M-18 and M-24 are considered so-called rheumatogenous. In this case, a stable hyperimmune response to various streptococcal antigens is determined with the formation of antibodies - antistreptolysin O (ASL-O), antistreptohyaluronidase (ASH), antideoxyribonuclease, etc.
Genetic factors play an important role
, which is confirmed by the more frequent incidence of the disease in children from families in which one of the parents suffers from rheumatism.
The importance of genetic factors is to a certain extent evidenced by the results of studying the association of histocompatibility antigens, which revealed, in particular, the frequent occurrence of Dr5–Dr7, Cw2–Cw3 and a number of others in patients with different forms of rheumatism. The genetic marker of this disease, according to a number of researchers, is the B-lymphocyte alloantigen
, determined using monoclonal antibodies D8/17, which is found with high frequency both in patients with rheumatism and in their close relatives. It is associated with a hyperimmune response to streptococcal antigen.
In the pathogenesis of rheumatism, the direct or indirect damaging effects of streptococcal components and its toxins on the body with the development of immune inflammation are of no small importance. Anti-streptococcal antibodies that cross-react with heart tissue (molecular mimicry)
.
Morphological changes
reflect systemic disorganization of connective tissue, especially the cardiovascular system with specific necrotic-proliferative reactions (Ashoff-Talalaev granulomas) and nonspecific exudative manifestations. The latter are more distinct in childhood, which determines the greater (compared to adults) severity and activity of the process, the severity of carditis and other manifestations of rheumatism.
Clinical picture
Rheumatism in children is characterized by a variety of clinical manifestations and variability of course. As a rule, it occurs at school age, less often in preschoolers
and practically does not occur in children under 3 years of age.
In typical cases, the first signs of rheumatism are detected 2–3 weeks after a sore throat or pharyngitis
in the form of fever, symptoms of intoxication, articular syndrome, carditis and other manifestations of the disease. It is also possible for the disease to have asymptomatic onset with the appearance of fatigue, low-grade fever, in the absence of noticeable disorders of the joints or heart, which can be mistakenly regarded as residual effects of a previous infection.
Joint syndrome
One of the earliest signs of rheumatism is articular syndrome (arthritis or arthralgia), detected in 60–100% of affected children. Rheumatoid arthritis is characterized by an acute onset, involvement of large or medium-sized joints (usually knee, ankle, elbow) in the form of mono- or oligoarthritis, volatility of the lesion, and rapid reversal of the process. Articular syndrome relatively rarely develops in isolation at the onset of the disease; more often it is accompanied by cardiac disorders.
Heart damage
Symptoms of heart damage ( carditis
) are determined in 70–85% of cases at the onset of the disease and somewhat more often during subsequent attacks, depending on the predominant localization of the process in the myocardium, endocardium, and the degree of involvement of the pericardium. Due to the difficulty of identifying signs of damage to one or another lining of the heart, the term “rheumatic carditis” is used in practice.
Complaints of a cardiac nature (pain in the heart, palpitations, shortness of breath) are observed in children mainly with severe cardiac disorders. More often, especially at the onset of the disease, various asthenic manifestations (lethargy, malaise, increased fatigue) are observed.
The first objective signs of rheumatic carditis are: disturbance of heart rate (tachycardia, less often - bradycardia); increase in heart size, predominantly to the left; muffled heart sounds, the appearance of systolic murmur.
Character of systolic murmur
, its localization is determined by the degree of involvement of the myocardium and endocardium in the process.
With myocarditis
, the murmur is usually weak or moderate and rarely extends beyond the heart.
In case of endocarditis
with the most characteristic lesion of the mitral valve in rheumatism (valvulitis), a prolonged blowing systolic murmur is heard with a maximum at the apex and at Botkin's point, intensifying on the left side and during exercise, conducted outside the heart. It is mitral valve valvulitis that plays the main role in the formation of valvular heart defects, the development of which can be established no earlier than 6 months from the onset of the disease. The development of rheumatic carditis may be accompanied by circulatory failure, usually not exceeding stage I.
On ECG
with rheumatic carditis, rhythm disturbances are often detected (tachy- or bradyarrhythmia, migration of the pacemaker, sometimes extrasystole, atrial fibrillation),
slowing of atrioventricular conduction
, mainly of the first degree, disturbances in ventricular repolarization, prolongation of electrical systole.
The phonocardiogram (PCG) records a decrease in the amplitude of the first tone at the apex and an increase in the amplitude of the third and fourth sounds. In case of myocarditis, FCG reveals a systolic murmur that is not associated with the first sound, variable in different cardiac cycles, and having a medium-amplitude, medium-frequency character. Mitral valve valvulitis is manifested by high-frequency pansystolic or protosystolic murmur of varying amplitude.
X-ray
in addition to the not always pronounced enlargement of the heart, signs of decreased tonic and contractile function of the myocardium, mitral (with valvulitis of the mitral valve) or aortic (with damage to the aortic valve) configuration of the heart are determined.
When performing an echocardiography, thickening, “shaggy” echo signal from the leaflets of the affected valves, a decrease in their excursion, signs of impaired myocardial contractile function and a number of other symptoms are revealed. With rheumatic carditis in children, the development of pericarditis is also possible, the clinical manifestations of which are determined much less frequently than instrumental signs on the ECG and especially EchoCG.
Currently, with timely treatment, primary rheumatic carditis ends in recovery in most children. The formation of valvular heart defects, often with the development of mitral insufficiency, is determined in 15–18% of cases during the first attack, mainly in severe, protracted or latent course of the disease.
With repeated attacks, which, according to the recommendation of the American Heart Association (AHA), are considered as a new episode of acute rheumatic fever, and not a relapse of the first, the formation of heart defects, often in the form of combined and/or combined valvular lesions, reaches 100%. Due to rheumatic carditis, the formation of prolapse of the mitral (less often aortic) valves
, development
of myocardiosclerosis
with rhythm and conduction disturbances (extrasystole, atrial fibrillation, complete atrioventricular block), as well as
adhesive pericarditis
. Severe rheumatic carditis, its relapses, the presence of myocardiosclerosis, and heart defects contribute to the development of persistent heart failure, leading to disability in patients and possible death.
Small chorea is characteristic of childhood rheumatism
, occurring
in 12–17% of cases
, mainly in early puberty and in girls. Classic symptoms of minor chorea: hyperkinesis, hyper- or hyporeflexia, muscle hypotonia, impaired coordination of movements, changes in psychological state and various autonomic disorders.
The disease begins acutely or, more often, gradually. Children develop emotional lability, irritability, changeable mood, tearfulness, absent-mindedness, memory loss, and deterioration in academic performance. An objective examination reveals involuntary twitching of the muscles of the face and limbs with grimacing, jerky, awkward movements; slurred, unclear speech, changes in handwriting, gait, which makes feeding, dressing, and learning difficult. Hyperkinesis is often bilateral in nature, intensifies with excitement, weakens during sleep until it stops completely.
Often, minor chorea precedes the development of rheumatic carditis or proceeds without clear disturbances in cardiac activity, and is characterized by a torpid course and a tendency to relapse.
Other symptoms
Rarer symptoms of rheumatism include annular rash and rheumatic nodules
.
Annular rash
(ring-shaped erythema) - pale pink, dim rashes in the form of a thin ring-shaped rim, which do not rise above the surface of the skin and disappear with pressure. It is found in 7–10% of children with rheumatism, mainly at the height of the disease and is usually unstable.
Subcutaneous rheumatic nodules
– round, dense, inactive, painless, single or multiple formations localized in the area of large and medium-sized joints, spinous processes of the vertebrae, in tendons, on the aponeurosis. Currently, they are rare, mainly in severe forms of rheumatism, lasting from several days to 1–2 months.
Abdominal syndrome, damage to the lungs, kidneys, liver and other organs due to rheumatism in children is now extremely rare, mainly in severe cases.
Laboratory indicators
Laboratory indicators in patients with rheumatism reflect signs of streptococcal infection, the presence of inflammatory reactions and an immunopathological process. In the active phase, the following are determined: leukocytosis with a shift to the left, an increase in ESR, and often anemia; increased levels of seromucoid, diphenylamine reaction; dysproteinemia with hypergammaglobulinemia; increased titers of ASH, ASLO, increased immunoglobulins class A, M and G; C-reactive protein (CRP), circulating immune complexes, anticardiac antibodies.
Diagnostics
As is known, there are no specific tests for diagnosing rheumatism. In practice, the syndromic method of assessing the status of the patient
, the principle of which was proposed in 1940 by the domestic pediatrician A.A. Kisel.
The author identified such syndromes pathognomonic for rheumatism as migratory polyarthritis, carditis, chorea, annular erythema, and rheumatic nodules as the main diagnostic criteria. Later, A.I. Nesterov made additions to the criteria, and for a long time, when establishing the diagnosis of rheumatism, doctors used the Kisel-Jones-Nesterov criteria. Subsequently, this scheme was repeatedly modified, and currently, in accordance with WHO recommendations, the Jones diagnostic criteria
, revised by the AKA in 1992, are used as international criteria for acute rheumatic fever (Table 1).
The detection of two major or one major and two minor criteria in a patient, combined with data documenting a previous infection with group A streptococci, indicates a high probability of acute rheumatic fever. However, in the early stages, nosological diagnosis in conditions of vague and nonspecific symptoms presents certain difficulties.
The final diagnosis is often established after a thorough differential diagnosis and dynamic observation of the patient with assessment of the results of the therapy.
Differential diagnosis
The differential diagnosis of rheumatism is carried out with a large group of conditions and diseases occurring with articular syndrome (reactive arthritis, juvenile rheumatoid arthritis, Lyme disease, leukemia, neoplastic processes); with a number of inflammatory cardiac diseases (non-rheumatic carditis, infective endocarditis); congenital and acquired disorders of the heart structure (mitral valve prolapse, congenital mitral valve insufficiency or anomaly of its development); autonomic dystonia syndrome. The diagnosis of minor chorea requires, first of all, the exclusion of thyroid hyperkinesis in children, Tourette's syndrome, and chorea in systemic lupus erythematosus.
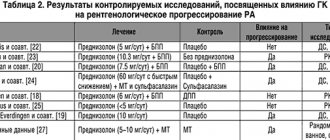
The formulation of the diagnosis and, accordingly, treatment is carried out on the basis of the classification developed by A.I. Nesterov and the nomenclature of rheumatism (Table 2).
Determining the degree of process activity
(I, II, III) is carried out taking into account the severity of clinical and laboratory manifestations.
The acute course
reflects the rapid development of rheumatism, polysyndromic nature, and vivid clinical and laboratory manifestations (duration – 2–3 months).
The subacute course
may (at its onset) resemble an acute one or is characterized by a slower onset of the disease, less pronounced clinical and laboratory manifestations (duration – up to 6 months).
The protracted course is characterized by moderate signs of activity, torpidity to the therapy (duration - more than 6 months). With a relapsing course,
polysyndromic nature, severity of clinical manifestations, and relapses are noted. The latent course is characterized by the progression of heart disease in the absence of signs of process activity.
Treatment
Treatment of rheumatism in children is based on the early administration of complex therapy aimed at suppressing streptococcal infection and the activity of the inflammatory process, preventing the development or progression of heart disease. The implementation of these programs is carried out according to the principle of stages: 1st stage - inpatient treatment, 2nd stage - follow-up treatment in a local cardio-rheumatological sanatorium, 3rd stage - dispensary observation in a clinic.
Stage 1
At the 1st stage in the hospital, the patient is prescribed drug treatment (antibacterial, antirheumatic and symptomatic), nutritional correction and physical therapy, which are determined individually taking into account the characteristics of the disease and, above all, the severity of carditis. Due to the streptococcal nature of rheumatism, etiotropic therapy is carried out with penicillin
.
Antirheumatic therapy involves one of the nonsteroidal anti-inflammatory drugs (NSAIDs
), which are prescribed alone or in combination with
glucocorticosteroid hormones (GCS)
, depending on the indications (Table 3).
Antibacterial therapy
penicillin is carried out for 10–14 days. In the presence of chronic tonsillitis, frequent exacerbations of focal infection, the duration of treatment with penicillin is increased, or another antibiotic is additionally used - amoxicillin, macrolides (azithromycin, roxithromycin, clarithromycin), cefuroxime axetil, and other cephalosporins in an age-specific dosage.
NSAIDs
apply for at least 1–1.5 months until signs of process activity are eliminated.
Prednisolone
in the initial dose is prescribed for 10–14 days until a clinical effect is obtained, then the daily dose is reduced by 2.5 mg every 5–7 days under the control of clinical and laboratory parameters, and subsequently the drug is discontinued.
Duration of treatment with quinoline drugs
for rheumatism, it ranges from several months to 1–2 years or more, depending on the course of the disease.
Chronic foci of infection are also sanitized in a hospital setting.
, in particular, tonsillectomy, carried out 2–2.5 months from the onset of the disease in the absence of signs of process activity.
Stage 2
The main task at the second stage is to achieve complete remission and restore the functional capacity of the cardiovascular system of children with rheumatism. In the sanatorium, the therapy started in the hospital is continued, foci of chronic infection are sanitized, and the appropriate treatment and health regimen is carried out with differentiated physical activity, physical therapy, and hardening procedures.
Stage 3
The third stage of complex therapy for rheumatism involves the prevention of relapses and progression. For this purpose, long-acting penicillin
, mainly bicillin-5, the first administration of which is carried out during the period of hospital treatment, and subsequently - 1 time every 2-4 weeks year-round. Regularly, 2 times a year, an outpatient examination is carried out, including laboratory and instrumental methods; prescribe the necessary health measures and physical therapy. For children who have had rheumatic heart disease and have valvular heart disease, bicillin prophylaxis is carried out until they reach the age of 21 years or more. For rheumatism without cardiac involvement, bicillin prophylaxis is carried out for 5 years after the last attack. In the spring-autumn period, along with the administration of bicillin, a monthly course of NSAIDs is indicated.
Prevention of rheumatism is divided into primary and secondary.
Primary prevention
is aimed at preventing rheumatism and includes:
1. Increasing immunity (hardening, alternating exercise and rest, good nutrition, etc.).
2. Detection and treatment of acute and chronic streptococcal infections.
3. Preventive measures for children predisposed to the development of rheumatism: from families in which there are cases of rheumatism or other rheumatic diseases; often suffer from nasopharyngeal infection; having chronic tonsillitis or having had an acute streptococcal infection.
Secondary prevention
is aimed at preventing relapses and progression of the disease in children with rheumatism under conditions of clinical observation (see earlier: “Third stage of therapy”).
Key Concepts
Rheumatism is a disease that develops in connection with a streptococcal infection, mainly at the age of 7–15 years. It is characterized by polymorphism of clinical manifestations and variability of course.
The clinical picture of the disease is primarily characterized by heart damage, articular syndrome and minor chorea; Its other manifestations are less common. Cardiac symptoms are caused by the predominance of endo- or myocardial damage with the possible, but more rare, development of pericarditis. A characteristic feature of rheumatic carditis is the development of mitral valve valvulitis. Articular syndrome is often determined already at the onset of the disease in the form of unstable arthritis or arthralgia. The priority of rheumatism in children is minor chorea, which has quite characteristic clinical symptoms.
Primary rheumatism with timely treatment usually ends in recovery. The development of heart defects, as a rule, is manifested by mitral insufficiency with the possibility of subsequent addition of other valvular disorders. Repeated attacks of rheumatism much more often lead to the formation of heart defects.
Treatment of children with rheumatism is carried out on the basis of the principles of staged therapy, depending on the nature of the existing pathology, the degree of activity of the process and the characteristics of its course. For these purposes, antibiotics, NSAIDs, and glucocorticosteroids are used.
An integral part of preventive measures for rheumatism is primary and secondary prevention, aimed at preventing the development of the disease, the occurrence of relapses and the progression of the pathological process.
Literature
1. Belov B.S. “Modern aspects of diagnosing acute rheumatic fever in adolescents.” Det. rheumat. 1996; 2.
1. Belov B.S. “Modern aspects of diagnosing acute rheumatic fever in adolescents.” Det. rheumat. 1996; 2.
2. Belov B.S. “Modern aspects of acute rheumatic fever” Lecture for doctors. Moscow, 1998.
3. Dolgopolova A.V., Kuzmina N.N. “Primary rheumatic carditis in children.” M., Medicine, 1978.
4. Kuzmina N.N. “The problem of rheumatism in children at the present stage.” Det. Rheumat., 1996; 2.
5. Nasonova V.A., Kuzmina N.N., “Rheumatism” in the book. “Rheumatic diseases” (a manual for doctors edited by Nasonova V.A., Bunchuk N.V.). M., “Medicine”, 1997.
6. Nesterov A.I. "Rheumatism". M., Medicine, 1973.
| Applications to the article |
| Risk. In type I diabetes mellitus, diabetic retinopathy occurs in 70% of cases (proliferative retinopathy - 45%, blindness - 10%), in type II diabetes mellitus - in 39% of cases. |
| cost $10.5 million from 1972 to 1982. The study generated a net benefit of $231 million to society and provided patients with a total of 279,000 years of vision. |
| Therapeutic treatment of myopia includes drugs that affect accommodation, improve hemodynamics of the eye, and stimulate metabolic processes in the tissues of the eye. |
| Patients with primary dyslexia (the inability to read with intact intelligence, unimpaired visual functions and normal motivation) have a defect in the visual memory center, which makes it difficult for the child to retain visual information about symbols. |
| Fact. The number of nerve fibers in the optic disc varies from 800,000 to 1,200,000 and gradually decreases with age. |
| Possible oligosymptomatic onset of rheumatism with the appearance of fatigue and low-grade fever |
| The formation of valvular heart defects is determined in 15–18% of cases during the first attack |
Treatment of rheumatoid arthritis of the knee joint
The methods used to combat the disease are divided into non-drug and drug-based. Surgery (surgery) is used in extreme cases.
Non-drug treatments for rheumatoid arthritis of the knee:
- Pharmacopuncture. Designed to relieve inflammation and provide nutrition to the damaged joint.
- Shock wave therapy, which serves to restore normal blood supply. Returns the ability to bend the leg at the knee.
- Vacuum therapy is a type of massage based on the organization of low pressure zones in a certain area.
- Magnetotherapy. It has an analgesic and anti-inflammatory effect on affected joints.
- Laser therapy. Increases local immunity, has anti-inflammatory and sedative effects, improves blood circulation.
In contrast, some medications, in addition to the obvious effect (relieving pain, inflammation, etc.), may also have side effects:
- non-steroidal anti-inflammatory drugs;
- basic medications, the use of which begins immediately after diagnosis and can continue throughout life;
- hormonal agents.
How to treat rheumatoid arthritis of the knee joint and in what ratio to use Eastern and Western methods, the doctor must determine individually.
Treatment
First of all, sanitation of foci of inflammation is carried out in chronic diseases of the ENT organs and the oral cavity (sinusitis, tonsillitis, caries). Treatment of acute streptococcal infection is carried out in a hospital. To combat it, antimicrobial and anti-inflammatory (nonsteroidal and corticosteroid) drugs are used. Symptomatic manifestations are neutralized with analgesic ointments and compresses, and ultraviolet irradiation procedures may be prescribed. To prevent relapses of streptococcal infections, drug prophylaxis is prescribed under the supervision of a physician.
Proper nutrition for rheumatoid arthritis of the knee joint
The diet for rheumatoid arthritis is based on several principles:
- you need to eat in small portions, at least 4 times a day;
- You should avoid cold dishes and limit the consumption of highly heated foods;
- it is necessary to reduce salt intake to the amount indicated by the doctor;
- drink about 2 liters of liquid per day.
Healthy foods that should form the basis of your diet:
- fruits and vegetables;
- bread - rye or bran;
- cereals;
- fresh greens are a source of vitamin C, iron, calcium;
- lean meat;
- sea fish;
- dairy products;
- green tea, natural juices.
You should limit yourself to sour, salty, spicy foods, coffee and alcohol, and avoid fatty foods.
Gymnastics for rheumatoid arthritis of the knee
Physical exercise will help keep muscles toned and maintain joint mobility. The intensity of the exercises is determined by the doctor, who can supplement the list of basic exercises:
- lying on your back, bend your leg at the knee joint, without lifting the sole off the floor;
- bending your knees, make rotational movements, as when riding a bicycle;
- bending your knees, spread them apart and bring them back;
- swing your legs without bending them at the knee (lying and standing);
- make circular movements with the leg bent at the knee;
- spreading straight legs to the sides in a lying position.
When prescribing gymnastics for rheumatoid arthritis of the knee, the doctor takes into account the presence of concomitant diseases and the degree of damage to the joint.
Causes
In modern medical practice, the name “rheumatism” has been replaced by the term “acute rheumatic fever.” This name of the disease more accurately characterizes the etiology of the disease - it is caused by a previous infection with streptococcus A. As a rule, infection with streptococcus is associated with a previous sore throat, scarlet fever, and the presence of chronic inflammatory diseases of the ENT organs.
The cause of rheumatic joint damage when infected with streptococcus A is not only the toxic effect of its enzymes on connective tissue, but also the similarity in the structure of proteins of some strains of streptococcus and body tissues, which is more important. When an immune response to streptococcal infection occurs, the body begins to produce antibodies that attack the person’s own tissues. First of all, as we wrote above, the membranes of the heart are affected, then the pathological changes “spread” to the rest of the body, affecting the connective tissues. By the way, it was this method of spread that gave the name to the disease - “rheuma” is translated as “flow/flow”.
No matter how strange it may seem, most often it is not only elderly people who suffer from rheumatism, including the limbs, but also schoolchildren. The reason is a weak immune system and the infectious nature of the pathology. According to statistics, this disease affects schoolgirl girls 3-4 times more often than boys.