Injuries to the ankle, knee and wrist joints are the most common reasons for visiting a traumatologist. These joints suffer as a result of both sports and everyday injuries, and the degree of complexity of such injuries varies quite widely.
With serious joint injuries, cartilage is often destroyed, swelling and hemorrhage occur, and the joint can become blocked. All this is accompanied by severe pain. In addition, articular cartilage often suffers from inflammatory pathologies and degenerative diseases. Joint diseases should not be ignored under any circumstances, since advanced pathology leads to the development of arthrosis and a reduction in the patient’s motor capabilities.
Unpleasant sensations in the joint can be temporarily eliminated with the help of medications. Physiotherapy, massage and physical therapy will help with injuries. However, conservative methods of treating damage to articular cartilage are not always effective, and then it is necessary to resort to surgical intervention.
There are many methods of surgical treatment of damage to articular cartilage, successfully used in Israeli clinics, including by specialists from the Ilyssa Medical Group center. Let's look at some of these techniques in more detail.
Microfracture
In this procedure, the doctor uses a small drill or special cutter to make tiny holes in the cartilage. The body immediately tries to patch up these holes by producing new tissue, so after some time, fibrous cartilage is formed in the microfractured area, covering the defect site.
This method of articular cartilage restoration is minimally invasive and easily tolerated by patients. In addition, this procedure can significantly delay more serious interventions, such as joint replacement. However, this method has a significant drawback: due to the fact that the new cartilage has a completely different structure than normal hyaline cartilage, it cannot be a complete replacement.
Diagnosis of knee cartilage rupture
On the surface of the joint is the so-called hyaline cartilage. When it becomes damaged and begins to tear, its surface becomes uneven. This is why the symptoms appear: pain and difficulty in movement.
Damage to articular cartilage is difficult to detect because the tissue contains virtually no calcium and is not visible on x-rays. Diagnosis of cartilage rupture is a rather problematic task.
The best option would be to use the arthroscopy method to accurately identify all pathologies in the knee joint. Diagnosis by arthroscopy proceeds as follows: a specialist makes several incisions on the knee, into which an arthroscope is inserted, at the end of which a camera is placed. This way, a picture is displayed on the screen and you can clearly see all the problems in the knee joint.
Transplantation of your own cartilage tissue
Damaged tissue can also be “repaired” using small cartilage cylinders removed from the patient himself. Such fragments of healthy tissue are installed in the articular ends of the bone in a mosaic pattern, which is why the operation is called “mosaic chondroplasty”. As a donor tissue, they usually take a cartilaginous surface that does not have a load-bearing or supporting function, and they try to fill the affected area as tightly as possible. In such a situation, the formation of fibrocartilage will be fragmentary, only where there are no grafts.
This type of intervention is also performed arthroscopically. Its disadvantages include the fact that mosaic chondroplasty is not applicable on large surfaces due to the lack of a sufficient amount of donor material for autografts. In addition, a pathological process may also develop in the place where the donor material was removed.
Treatment
The goals and objectives of therapy are to reduce the frequency of inflammation, improve nutrition, eliminate provoking factors of injury, restore the integrity and smoothness of cartilage and the biomechanics of the joint. This is achieved by conservative and surgical methods. Taking anti-inflammatory drugs orally reduces inflammation. This therapy is complemented by oral administration of chondroprotectors and external use of ointments. If necessary, anti-inflammatory drugs are administered peri- and intra-articularly. Intra-articular injections of hyaluronic acid enriched with platelet-rich plasma restore the normal properties of synovial fluid, reduce the inflammatory response and promote cartilage regeneration. Surgical methods include arthroscopy, in which, after identifying the site of damage, removal of irregularities is performed, abrasive chondroplasty (restoring integrity by achieving the formation of a fibrous clot on its surface during microfracture of the subchondral bone), mosaic chondroplasty (introduction of osteochondral autografts). After surgery, a rehabilitation course helps to quickly restore joint function. All treatment together helps prevent the development of osteoarthritis and eliminate pain symptoms, improving the patient’s quality of life.
Transplantation of cartilage grown in laboratory conditions
Modern technologies make it possible to grow donor cartilage cells “in vitro”. The doctor, in the same way as with mosaic chondroplasty, removes small fragments of cartilage cells from an area where there are no large anatomical loads and places them in a nutrient solution. Cartilage tissue of the required size is grown there. This usually takes several weeks (on average about three).
Then another operation is performed, during which new tissue is transplanted into the patient. It is not rejected by the body. This technology is usually used to restore ankle cartilage
, but not used for severe arthrosis. The operation is indicated for young and healthy people in whom the new tissue will take root and be well supplied with blood.
The cartilage tissue transplantation operation itself lasts from an hour to two hours, after which the patient undergoes a long period of rehabilitation; for a month or two he has to walk on crutches so as not to put stress on the joint. Sports activities are permissible only one year after the transplantation of laboratory-grown tissue.
Causes of damage
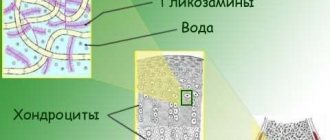
The destruction of cartilage and loss of its properties can occur in a natural mode for the body and under stress. In the first case, over time, there is a decrease in nutrition from the subchondral bone, where the structure of the vessels and their number change, and the bone layer becomes denser and regenerates more slowly. In addition, with age, the production of collagen and hyaluronic acid decreases, the amount of water decreases - cartilage tissue loses its properties and is damaged even with minor loads. In the second case, joint injuries occur, in which the integrity of one or another of its structures is disrupted by an impact or excessive sudden movement. Next, the body reacts to the deformation with an inflammatory process, as a result of which the resulting defects are replaced by scar tissue that does not have elastic properties. In addition, during the process of inflammation, the properties of the synovial fluid change, in which the amount of hyaluronic acid and chondroitin decreases. It also takes time to restore them. Until this happens, he is in a nutritional deficiency and is more susceptible to friction - which means microtrauma again. So, with each damage, the cartilage loses its properties, which means it becomes more vulnerable. A vicious circle arises. The result is its degeneration. This is exactly what happens with arthrosis.
Endoprosthetics
If there is a significant deterioration in joint function and severe pain, an operation such as joint replacement using artificial implants is usually prescribed. One of the methods of endoprosthetics - resurfacing - involves the removal of altered articular cartilage and its subsequent replacement with a cap-shaped prosthesis, which is placed on a specially prepared bone. Other arthroplasty techniques involve replacing not only cartilage, but also the bone elements of the joint.
Blood tests for arthritis Knee arthrotomy
Why do joints wear out?
Throughout life, the legs bear a heavy load; when running or jumping, the joints take on a weight two to three times greater than the body weight of the “owner”. Everything has a limit, so by the age of 60, the cartilage in the joints becomes thinner and wears out. For some, arthrosis begins earlier, for example, women are more susceptible to the disease due to hormonal changes, athletes - due to intense exercise, and people who lead an unhealthy lifestyle “kill” their joints with junk food, alcohol or drugs.
What is cartilage wasting
Arthrosis goes through several stages. At the initial stage, subtle changes appear in the joint. On the last one, they talk about complete wear of the cartilage and the impossibility of its restoration. His fate directly depends on the stage at which a person consults a doctor.
Normally, articular cartilage is elastic and dense, so in a healthy state it easily performs a shock-absorbing function during movement. As a result of degenerative processes, the height of the cartilage decreases, it loses moisture and ceases to be elastic, begins to crack and delaminate.
As cartilage depletes, the negative impact on surrounding tissue increases. Bone surfaces, tendons, muscles, and joint capsules suffer. Morning stiffness and pain after physical activity appear. The thinner and stiffer the cartilage tissue, the worse the joint functions.
Joint destruction begins with cartilage depletion
Is cartilage capable of restoration? What does science say?
Joint injuries
The most consistent symptoms are pain and swelling in the joint area. Hemorrhages are possible. Movement restrictions of varying severity are observed. In this case, as a rule, the more severe the joint injury, the more movement is limited. At the same time, with some injuries (ligament ruptures, fractures), excessive (pathological) mobility may be detected. In case of displaced fractures and ligament ruptures, visible deformation is determined: the contours of the joint are disrupted, the distal segment may deviate to the side.
A particularly pronounced deformity is detected during dislocations: the line of the limb is roughly bent, natural bony protrusions in the joint area disappear, and sometimes a protruding articular end of the distal and/or proximal segment becomes visible. Very often, with injuries, blood accumulates in the joint (hemarthrosis), in such cases the joint increases in volume, becomes spherical, its contours are smoothed, and fluctuation is determined.
To clarify the diagnosis of joint injuries, radiography, ultrasound, CT, MRI and arthroscopy are used. X-ray is the most accessible and informative technique that allows you to exclude severe skeletal injury or confirm the diagnosis of a fracture or dislocation, as well as determine the position of the articular ends and bone fragments. In most cases, X-ray data are sufficient both to determine the general treatment tactics (reposition, skeletal traction, surgery) and for detailed planning of treatment measures (choice of reposition method or surgical intervention method).
If necessary, for joint injuries with damage to bones and cartilage, CT of the joint is additionally used. For soft tissue injuries, radiography is prescribed only to exclude bone pathology, and to clarify the diagnosis in such cases, MRI of joints and ultrasound are used. For some joint injuries, arthroscopy becomes the best option - a therapeutic and diagnostic study, during which the doctor can conduct a direct visual examination of the intra-articular structures, and sometimes immediately eliminate the problems that have arisen.
Knee injuries
Knee injuries are very diverse - from bruises, meniscal injuries and ligament tears to fractures of the patella and the articular ends of the tibia and femur. For bruises, rest, UHF and elevated position of the limb are prescribed. In case of tears of the lateral ligaments, a cast is applied for a period of 3-4 weeks; in case of complete ruptures, surgical intervention is performed (suturing or plastic surgery of the ligament) followed by immobilization for 2-3 weeks.
For cruciate ligament tears, the immobilization period is 3-5 weeks. In case of complete ruptures, an operation is prescribed during which the damaged ligament is replaced with Mylar tape. In the postoperative period, immobilization is also carried out for 2-3 weeks. For fractures of the femoral and tibial condyles, reposition is performed followed by immobilization, skeletal traction is applied, or osteosynthesis is performed with a screw, bolt or nail.
In case of damage to the menisci, surgical intervention is necessary. Currently, preference is given to economical operations; if possible, the menisci are not removed, but resected, since this treatment tactic reduces the likelihood of developing post-traumatic arthrosis. Operations are performed both through open access and using arthroscopic equipment. For all types of joint injuries, physiotherapeutic procedures and exercise therapy are prescribed.
Ankle injuries
The most common ankle injuries are ligament injuries and ankle fractures. Tears and ruptures of ligaments are treated conservatively: depending on the severity of the injury, a pressure bandage or plaster splint is applied, painkillers and physical treatment are prescribed. An ankle fracture can be unimalleolar (only the outer or only the inner ankle is damaged), bimalleolar (the inner and outer ankles are damaged) and trimalleolar (both ankles and the anterior or posterior edge of the tibia are damaged).
Fractures with and without displacement of fragments, with subluxation and without subluxation are possible. Treatment is usually conservative. If necessary, reposition is performed and a cast is applied. The immobilization period is 4 weeks for each broken ankle: for a single-malleolar fracture - 4 weeks, for a double-malleolar fracture - 8 weeks, for a tri-malleolar fracture - 12 weeks. In case of irreparable displacement and unstable fractures, surgical intervention is performed - osteosynthesis with screws, knitting needles, or a two-bladed nail. Patients are prescribed analgesics, UHF and exercise therapy.
Shoulder injuries
The most common joint injuries are shoulder dislocations and fractures of the surgical neck of the humerus. Dislocations are more often diagnosed in men of working age, and surgical neck fractures are diagnosed in older women. Reduction of fresh dislocations is carried out under local anesthesia, stale ones - under general anesthesia. Then immobilization is carried out for 3 weeks, UHF and exercise therapy are prescribed. With weakness of the ligamentous apparatus and premature onset of movements, the formation of a habitual dislocation of the shoulder is possible. In such cases, surgical treatment is indicated.
Surgical neck fractures are usually extra-articular; sometimes cracks extending from the main fracture line extend under the joint capsule. Damage to the cervix can be impacted, abduction (abductor) and adduction (adductor). At the initial stage, reposition and immobilization are carried out. For abduction and impacted injuries, a roller is placed in the axillary area; for adduction injuries, a triangular splint is used. For both dislocations and fractures of the neck, painkillers and physiotherapeutic procedures are prescribed, and an almost similar complex of exercise therapy is used.
Elbow injuries
The elbow joint is considered one of the most difficult and “capricious” to treat. In the early period, with severe joint injuries, neurological and vascular disorders may occur; in the long term, contractures often form, and post-traumatic arthrosis may develop. Bruises are considered the mildest joint injury. Treatment of bruises is conservative: rest, analgesics, elevated position of the limb. The elbow joint does not tolerate intense thermal procedures well, so physiotherapy for bruises is usually not prescribed.
An olecranon fracture belongs to the category of prognostically favorable injuries. This joint injury is almost always accompanied by severe displacement of the fragment and requires surgical treatment. Osteosynthesis of the olecranon process with a plate, screws or wires is indicated; the result of treatment is usually good - movements are restored in full, there is no limitation of function. The most severe injuries are intra-articular fractures of the distal humerus and proximal forearm, including comminuted fractures, displaced fractures and fracture-dislocations.
For intra-articular fractures without displacement, a plaster cast is applied; for complex U- or T-shaped fractures, open reduction and osteosynthesis are performed with screws, screws or knitting needles. After the operation, immobilization is carried out, antibiotics and analgesics are used. During the recovery period, exercise therapy, massage and gentle physiotherapeutic procedures are prescribed: ultrasound or interference currents. The rehabilitation period ranges from 1-2 months to six months or more, depending on the severity of the joint injury.
Drug treatment
- The doctor prescribes a course of injections or tablets that have an analgesic and anti-inflammatory effect.
- Chondroprotectors. They are necessary to prevent the process of cartilage destruction, as well as for its restoration.
- In rare cases, corticosteroid injections directly into the joint cavity are prescribed. The pain disappears for several months, but then returns with renewed vigor, so the method is not used often.
- Diet for arthrosis.
- Special orthopedic shoes that reduce stress on joints.
What symptoms indicate that the cartilage has worn away?
- Joint pain bothers me when walking and becomes more intense over time.
- If arthrosis is not treated, it progresses, and the pain sometimes bothers you even at rest.
- It feels like the bones are rubbing against each other in the joint.
- When straightening, a crunching sound is heard.
- Swelling of the tissues over the joint.
Be careful! If the skin over the joint is hot or the body temperature is elevated, the reason is not that the knee joints are worn out, this is not arthrosis. Most likely, you are dealing with gout, infectious arthritis, or rheumatoid arthritis.
How else to help cartilage
The rate of restoration of damaged cartilage tissue depends on the number and activity of chondrocytes. Therefore, they need to be provided with adequate nutrition through synovial fluid, as well as to speed up their metabolism. Active movements contribute to this in the best possible way.
The more you move, the faster cartilage tissue is restored
Prolonged immobility leads to muscle atrophy and reduction of cartilage tissue, since it does not receive enough nutrients. Therefore, the least you can do with arthrosis is to ensure that a sufficient amount of fluid enters the body and move - of course, without fanaticism, to the best of your ability!
What drugs do doctors recommend for restoring cartilage tissue?
Medicines for the restoration of joint cartilage tissue are produced in the form of tablets, capsules, sachets (powders), injections, ointments, gels and creams. What drugs are most effective for restoring cartilage tissue? Depends on the stage of the disease, the affected joint and the individual characteristics of the body. Injections have the highest bioavailability, but can be traumatic. Therefore, most patients prefer sachets and tablets.
Please note: all medications to restore cartilage tissue of the spine and joints must be taken long-term and systematically. The first noticeable improvements may appear only after several months of use - this is due to the slow metabolism of cartilage.
Chondroprotective drugs for restoration of joint cartilage tissue
To restore cartilage tissue, “building material” is needed - special proteins and natural polymers that ensure the strength and functionality of synovial cartilage. Since there are very few of them in the diet of a modern person, chondroprotectors come to the rescue to restore cartilage tissue.
These medications require lifelong use in long courses (from 3 months), but they are able to completely restore minor damage to the surface of the cartilage, facilitate recovery from injuries to cartilage tissue, slow down the progression of arthritis and arthrosis, and protect bones and joints.
The most convenient for restoring cartilage tissue are chondroprotectors in sachets - for example, Artracam
. The sachet contains a dose of powder for a single dose (this medicine for the restoration of cartilage tissue of the spine and joints is taken once a day). This is quite convenient, because... you don’t have to carry a whole blister, or even a bottle of pills, to work. At the same time, the bioavailability of glucosamine sulfate in artracam powder is 90-95%, practically not inferior to injections.
The following have proven themselves well as chondroprotectors for the restoration of cartilage tissue:
- artracs;
- structum;
- chondramin;
- chondroglucide;
- movex;
- arthra chondroitin;
- artradol;
- chondroguard.
These drugs for the restoration of cartilage tissue can be used not only for treatment, but also for prevention.
Metabolism correctors and homeopathic medicines for restoration of joint cartilage tissue
The pharmaceutical group of homeopathic remedies includes drugs for the restoration of cartilage tissue with both proven and unproven effectiveness. Therefore, the choice of these drugs should be approached carefully, focusing on the doctor’s recommendations. Of greatest interest for the restoration of cartilage tissue are bioregulatory anti-inflammatory and relaxing agents of plant, animal and mineral origin, as well as external warming and locally irritating drugs.
- traumeel (lozenges and gel);
- target T (tablets);
- bischofite (compresses);
- tinctures and ointments based on the fruits of capsicum;
- Horsepower for joints (balm);
- toad stone (balm with toad extract).
Correctors of the metabolism of cartilage and bone tissue, in addition to chondroprotectors based on glucosamine and chondroitin sulfate, also include such reparative drugs as:
- piascledine;
- adgelon;
- vitreous body;
- Super Calcium;
- tridin;
- alendronic acid preparations (for example, osterepar);
- others.
These medications for restoring cartilage tissue of the spine and joints do not replace full-fledged therapy.
Angioprotective drugs for restoration of cartilage tissue
Angioprotectors and blood microcirculation correctors strengthen capillary walls, improve nutrition and restoration of cartilage tissue. Everyone knows that there are no blood vessels in the cartilage itself. However, their dense network permeates the perichondrium (perichondrium), which is responsible for the division of chondrocytes, growth and repair of cartilage tissue in case of damage. It is from the blood of the perichondrium that it receives the nutrients so necessary for the restoration of the cartilage tissue of the joints.
It is also important to strengthen the circulatory system to avoid fragility of blood vessels and hemorrhages into the joint cavity. A capillary rupture can cause even a harmless, at first glance, bruise. And with blood, infectious pathogens can enter the joint and begin to destroy cartilage tissue. This is especially dangerous for those patients who suffer from chronic foci of infection in the body - tonsillitis, caries, cholecystitis, rhinosinusitis, intestinal dysbiosis and others.
Therefore, as auxiliary drugs for the restoration of joint cartilage tissue, doctors prescribe:
- pentoxifylline (trental);
- horse chestnut extract (aescusan);
- troxerutin;
- troxevasin;
- cinnarizine;
- Detralex;
- angionorm;
- Cavinton;
- betahistine (tagista).
Synovial Fluid Prostheses
If pockets of erosion have already appeared on the cartilage, and there is not enough synovial fluid in the joint, lubricating prostheses are required for normal sliding of the cartilage. They allow the surface of the cartilage to rest and recover. Such drugs for restoring joint cartilage tissue are injected directly into the articular capsule of each affected joint. They are used primarily for the treatment of large joints. Replacement drugs for the restoration of joint cartilage tissue include:
- synvisc;
- fermatron;
- sinochrome;
- suplasin;
- ripart;
- Duralan;
- giruana;
- hyalrepayer.
Surgery for arthrosis
- The most popular is endoprosthetics of the affected joint
. This is the replacement of damaged areas with a prosthesis that looks like a healthy joint. - Arthroscopic joint debridement
. This operation is effective only at the initial stage of arthrosis. Using an arthroscope, the doctor makes several punctures in the joint and cleans its surfaces, removing the affected areas. Walking becomes painless and smooth, but the results will last for a maximum of two years, since the disease cannot be completely cured, only stopped, and then a more complex operation has to be performed.
Periarticular osteotomy
. The intervention is complex - both the operation and rehabilitation after it take a lot of time. But after periarticular osteotomy, the patient forgets about arthrosis for at least five years! The operation is performed under anesthesia. The surgeon saws the bones around the affected joint and fixes them at a different angle so that the joints do not touch the worn areas.
Patients who decide to undergo surgery and undergo treatment remain satisfied with their improved quality of life.
Causes of the disease.
Chondromalacia patella in athletes can occur as a result of injury to the knee joint. But more often its cause is chronic overload of the joint due to improper or excessive long-term load. The position of the kneecap is fixed by the quadriceps muscle of the thigh (quadriceps). The strength and tone of the muscles that form the quadriceps become imbalanced with prolonged tension. As a result, the position of the patella is incorrect, and the joint tissues wear out.