Arthritis of the ankle
is an acute or chronic inflammatory process in the ankle area, which leads to metabolic disorders in the joint structures. This condition is accompanied by pain and stiffness when moving. But its main danger is that if left untreated, the disease causes degradation of cartilage and even bone tissue and spreads to ligaments, tendons and muscles. In advanced cases, ankle arthritis leads to disability and loss of ability to work.
Arthritis of the ankle joints is debilitating with constant pain and can lead to complete disability.
Since the ankle joint is one of the most loaded joints in the human body,
when it is damaged, a person instinctively transfers his body weight to the other leg. This starts a “domino effect” - soon other joints of the lower extremities and spine begin to fail. Can this condition be prevented and how can ankle arthritis be treated if it has already been diagnosed?
General information about the disease
Arthritis of the ankle joint is an inflammatory process that has different origins, symptoms and course. The disease can be independent (primary) or develop against the background of some existing process (secondary). Arthritis is divided into acute and chronic. ICD-10 code M00 – M99.
The ankle joint is a movable joint formed by three bone structures: the heads of the tibia and fibula of the leg and the talus of the foot. To the right and left of the talus are bony elevations - the ankles. The peculiarity of the joint is its resistance to external influences, in this it is much superior to the knee joint. It has a good blood supply and innervation and is protected by ligaments that firmly hold it in the desired position.
Arthritis of the ankle develops at any age. In children it is predominantly juvenile idiopathic arthritis (JIA), in women it is rheumatoid lesions, in men it is reactive arthritis.
X-ray of the ankle joint at the Yauza Clinical Hospital
X-rays of the ankle joint in our hospital are performed by experienced radiology specialists using the Digital diagnost digital radiographic system (Philips, the Netherlands), which provides:
- high-quality image at maximum research speed due to digital signal transmission;
- convenience of the procedure (flat panel detectors allow you to obtain images in the required projection without moving the patient);
- instant availability of the received images to the doctors treating the patient (all images are sent immediately via Wi-Fi to the hospital server).
The results of our radiation diagnostics comply with all strict international protocols and are accepted in any medical institution in the world.
You can see prices for services
The article was checked by radiologist M.A. Petrova. , is for general informational purposes only and does not replace specialist advice. For recommendations on diagnosis and treatment, consultation with a doctor is necessary.
Causes
The causes of ankle arthritis vary. Very often, joint inflammation develops after an injury. Closed injury is accompanied by aseptic inflammation, which can go away on its own.
The cause of the development of purulent arthritis of the ankle and foot is the consequences of coccal infection entering the joint cavity after open injuries, surgical interventions or intra-articular injections. Sometimes the cause of the pathological process is a sexual or intestinal infection suffered some time ago. This kind of arthritis is called reactive, and it has a hereditary predisposition. Another disease that has a genetic basis is rheumatoid arthritis, the development mechanism of which is associated with autoimmune processes (allergy to the patient’s own tissues). Infectious arthritis develops against the background of specific infections: brucellosis, syphilis, gonorrhea, tuberculosis. The ankle is affected relatively rarely, usually with gonorrhea.
Arthritis can also be caused by psoriasis, gout, diseases of the gastrointestinal tract (GIT), connective tissue, etc.
Hereditary pathology is characterized by the presence of trigger factors that give impetus to the onset of the disease. These are previous infections, hypothermia, stress, the presence of foci of infection and concomitant diseases, excess body weight, a sedentary lifestyle, heavy physical activity, and unfavorable living conditions. There are also occupational hazards. The risk of developing ankle arthritis increases in people in such professions as dancers, loaders, weightlifters, military personnel of certain branches of the military, etc.
Symptoms of Ankle Arthritis
Despite the significant differences in the course of different clinical forms of the disease, they also have many common symptoms that can be used to suspect arthritis of the foot or ankle. It's worth paying attention to them.
First signs
In the acute course of arthritis of the ankle joint, severe pain occurs in the ankle and foot, tissue swelling, redness of the skin and increased temperature over the site of inflammation. Sometimes the patient’s general condition suffers: fever, chills, and malaise appear. With such complaints, patients immediately consult a doctor. With adequate treatment, the inflammatory process can almost always be cured. If left untreated, the inflammation subsides, becomes chronic and gradually leads to dysfunction of the limb.
The situation is much more complicated with chronic arthritis of the foot and ankle. They begin gradually, imperceptibly. The patient does not always pay attention to such “little things” as moderate pain in the ankle and foot, stiffness of movement in the morning and does not immediately seek medical help. This usually happens much later, when more characteristic signs of the disease appear.
Obvious symptoms
Over time, the symptoms of ankle arthritis become steadily worse. The pain intensifies, often bothering you at night and in the morning. Morning stiffness lasts for at least half an hour and this period increases. Swelling in the area of sore joints, ankles and the entire foot can be so significant that the foot does not fit into the usual type of shoes. A crunch appears in the joints.
Arthritis of the ankle joint can have a progressive, constant or wavy course with exacerbations and remissions. Obvious symptoms of the disease force the patient to see a doctor. But this does not happen at the initial stage.
But don’t lose heart: this disease can be treated at any stage.
Indications
X-rays of the ankle joint are performed for the following indications:
In traumatology (after injury) :
- acute pain in the ankle area;
- swelling at the site of the ankle injury;
- bruising in the ankle area;
- deformity in the area of ankle injury;
- inability to stand on the injured leg;
- monitoring the effectiveness of treatment (after a fracture, dislocation).
In orthopedics:
- congenital pathology of the osteoarticular system;
- osteomyelitis and vascular calcification in diabetes mellitus.
In oncology, if you suspect:
- benign and malignant tumors of the ankle area;
- metastases to the ankle joint.
In rheumatology , if systemic diseases are suspected:
- rheumatoid arthritis;
- osteoarthritis.
Why is arthritis of the ankle and foot dangerous?
The disease is dangerous because it often goes unnoticed and leads to a complete loss of joint function, that is, the person becomes disabled. Acute purulent complications of ankle arthritis are also dangerous.
Arthritis of the foot and ankle begins gradually, unnoticeably
Stages
There are several stages of disease development. The inflammatory process develops gradually, turning into a degenerative-dystrophic one:
- Early – inflammation
. The synovial membrane swells, and inflammatory exudate appears in the joint cavity. Pain is moderate, swelling and redness are absent or only slightly expressed. - Explicit – inflammatory-proliferative process
. The synovial membrane increases in volume, erosions appear on the cartilage, and soft granulations of connective tissue grow in the articular cavity (the process of proliferation - growth). The inflammatory process intensifies. Externally, this is manifested by increased swelling, redness and pain. - Progressive - mild ankylosis
. The cartilage is destroyed, soft granulations turn into dense connective tissue that grows in the joint cavity. Bone growths appear. The joint gradually loses its mobility. Pain, swelling and redness continue to bother you constantly or during exacerbations. - Advanced - complete immobility (bone ankylosis).
There is no cartilage tissue, bone growths connect the articular surfaces of the ankle, which eliminates movement in the ankle and foot (ankylosis of the ankle). The pain is constant, arthritis of the foot develops with limitation of its function.
Possible complications
If ankle arthritis is left untreated or treated independently with home remedies, the following complications may develop:
- purulent processes - abscesses, phlegmon, sepsis;
- subluxations and dislocations of the ankle;
- development of foot arthritis;
- immobility of the ankle and inability to move without assistive devices.
Prospects for recovery after surgery
Endoprosthetics allows you to completely restore the range of motion in the ankle, which compares favorably with arthrodesis. In the absence of complications and good rehabilitation, working capacity is quickly restored and the person returns to his usual lifestyle after 4-6 months.
Today, the incidence of complications after endoprosthetics has decreased significantly. This is due to the advent of more advanced instruments and third-generation prostheses, which perfectly reproduce the anatomical, physiological and mechanical characteristics of the ankle joint.
Please note that in some cases endoprosthetics may be refused. This happens when the operation cannot be completed. For example, with comminuted fractures, massive bone destruction, severe joint instability. In such cases, it is either impossible to install the endoprosthesis at all, or there is a high risk of its loosening. Therefore, doctors always decide on the choice of surgical treatment method individually, separately with each patient.
Clinical types of ankle arthritis
The disease progresses differently depending on the cause that caused it. Based on this feature, several clinical types of arthritis are distinguished. In the ankle area most often develop: post-traumatic (including purulent), rheumatoid, reactive, juvenile idiopathic, psoriatic and gouty arthritis.
Any form of arthritis has serious complications, so you should not delay treatment.
See how easily the disease can be cured in 10-12 sessions.
Post-traumatic
Aseptic arthritis after injury can occur unnoticed and go away on its own. But sometimes it is complicated by the addition of a purulent infection. This is evidenced by a sharp rise in body temperature, chills, malaise combined with swelling, redness and severe pain in the ankle area. Complications: spread of the purulent process to surrounding tissues and through the bloodstream to the entire body.
Sometimes post-traumatic arthritis of the ankle joint initially occurs chronically in the presence of a minor but constant traumatic factor. This often occurs in people of such professions as dancers, loaders and athletes. Complications: gradual loss of function, dislocations.
Rheumatoid (RA)
The inflammation is autoimmune in nature. The triggering factor is usually some kind of infection. Arthritis of the joints of the foot and ankle develops some time after an illness, hypothermia or severe stress in genetically predisposed people. A common disease, most often affecting middle-aged women.
Characterized by a gradual onset with symmetrical damage to both ankles. The very first manifestations are morning stiffness of movement in the ankle and foot, and slight pain. The disease develops slowly, but progresses steadily. The pain intensifies, swelling appears in the area of the affected joint. Redness of the skin is much less common in acute cases of the disease.
The muscles in the ankle area atrophy, the ligaments weaken, flat feet develop, the small joints of the toes are affected, and they become deformed with the foot deviating outward. At the last stage, subluxations of the ankle and foot joints appear. The disease is long-term and chronic, leading to limb deformation, loss of function and disability.
Rheumatoid arthritis of the foot and ankle joints is characterized by swelling in the area of the affected joint.
Reactive (ReA)
This clinical form of the disease develops within a month after a sexual or intestinal infection. Men who have a hereditary predisposition to the disease are more often affected.
ReA begins acutely, with fever, chills, painful swelling and redness of the ankle. Characteristic symptoms of arthritis of the foot and periarticular tissues – enthesitis – are added. Subcalcaneal bursitis develops with severe pain in the heel and feet, the first toe becomes inflamed and swollen. It is impossible to step on the foot because of the pain. The disease can last from 3 months to a year or more. A long-term chronic course with dysfunction of the lower extremities is characteristic of the urogenital type of ReA.
One of the subtypes of the disease is Reiter's disease, in which the inflammatory process develops simultaneously in the urethra, ankles and conjunctiva of the eyes. The disease is often chronic.
Read more about reactive arthritis in this article.
Juvenile idiopathic (JIA)
JIA develops in children and adolescents under 16 years of age. This includes all arthritis of unspecified origin, as well as rheumatoid, reactive, psoriatic and other chronic arthritis.
The ankle and foot are often affected, and the disease progresses both acutely and chronically. In this case, the limb quickly begins to lag behind in growth, muscle deformation and ligament weakness appear, which often leads to dislocations and subluxations of the foot.
Loss of limb function occurs quickly, the child becomes disabled if adequate treatment is not prescribed in a timely manner. Therefore, it is so important to consult a doctor in a timely manner.
Psoriatic (PsA)
It usually develops several years after the first skin symptoms appear. But sometimes the first manifestation of the disease is inflammation of the joints.
The ankles are often affected in PsA. The inflammation begins in one ankle, then rises up, as if climbing a ladder, and affects the knee. The small distal joints of the fingers and nails are often simultaneously affected. The onset of PsA is acute, with high fever, swelling and redness of the tissue over the affected areas. The course is undulating: relapses are replaced by remissions. Over time, this leads to impaired ankle function.
Chondroprotectors: what are they, how to choose, how effective are they?
Joint pain at rest
Gouty
Gout is a disease associated with impaired uric acid metabolism. During an attack of gout, salt crystals are deposited in the tissues, causing an acute inflammatory process.
Gout often affects the ankles. The attack develops acutely, suddenly with severe joint pain, swelling and redness of the tissues. The duration of the attack ranges from several hours to several days and weeks. Then the inflammation ends without any consequences. But with frequent recurrence of attacks in the ankle, its function is gradually impaired with the simultaneous development of arthritis of the foot and disruption of its function due to flat feet.
Deforming arthrosis-arthritis
It develops more often in old age against the background of injuries and thinning of the articular surfaces of bones (osteoporosis). It can also be the outcome of any type of arthritis of the foot and ankle if it lasts for a long time.
It develops gradually, leading to the proliferation of bone tissue, destruction and deformation of the ankles, flat feet and ankylosis.
YOU can call us: 8 (8452) 98-84-68 and +7-967-500-8468 or
Reactive arthritis is an inflammatory disease affecting the joints that develops after suffering certain infections (genitourinary, intestinal, nasopharyngeal).
The disease belongs to the group of seronegative spondyloarthritis. In most cases it is associated with acute or persistent intestinal (caused by Enterobacteriaceae) or urogenital chlamydial infection, but can also be associated with respiratory tract infections caused by mycoplasmas and chlamydia. There is evidence of a possible connection with some parasitic diseases.
A complex of symptoms including arthritis, conjunctivitis, urethritis or cervicitis, colitis and characteristic skin lesions is called Reiter's syndrome.
History The term “reactive arthritis” was first introduced by Finnish scientists K. Aho, K. Sievers and R. Ahvonen, who in 1969 described the occurrence of arthritis in enterocolitis caused by Yersinia. At the same time, the “reactive”, sterile nature of arthritis was emphasized and it was believed that there were no infectious agents and their antigens in the synovial fluid and synovial membrane.
Later, with the development of imaging and laboratory diagnostic methods, intracellular inclusions of Chlamydia trachomatis, microbial DNA and RNA fragments, as well as circulating immune complexes were discovered in the joint environment of patients. Later it was found that normally the joint is not sterile, and various microorganisms are often present in it.
As we studied, a close relationship between reactive arthritis and the HLA-B27 antigen was revealed. It has been found that antibodies to a number of microorganisms cross-react with HLA-B27 and can damage the body's own tissues during the immune response.
Etiology Today, the ability to cause reactive arthritis has been identified in many microorganisms:
Pathogens of intestinal infections: Yersinia enterocolitica Yersinia pseudotuberculosis Salmonella enteritidis Salmonella typhimurium Shigella flexneri Shigella sonnei Shigella Newcastle Campylobacter jejuni Clostridium difficile Pathogens of urogenital infections: Chlamydia trachomatis Pathogens of respiratory tract infections: Mycoplasma pneumoniae Chlamydophila pneumoniae
Epidemiology After a chlamydial urogenital infection, reactive arthritis develops in 1 - 3% of cases. After intestinal - in 1.5 - 4% of cases. People aged 20 to 40 years old, most often men, become ill. Urogenital reactive arthritis occurs in men 20 times more often than in women, enterocolitic arthritis occurs 10 times more often.
There is evidence that carriers of the HLA-B27 antigen develop arthritis 50 times more often after an intestinal or chlamydial infection than those who do not have this antigen.
Pathogenesis In the development of reactive arthritis, the phenomenon of cross-reaction of antibodies to the pathogen with the HLA-B27 antigen of the host's major histocompatibility complex has been revealed. A possible explanation for this is the theory of “molecular mimicry” - the structural similarity of proteins in the cell wall of bacteria with proteins in the cells of a sick person.
There are several immunological hypotheses for the pathogenesis of reactive arthritis.
Antigen-presentation hypothesis: according to it, the HLA-B27 complex is capable of presenting microbial peptides that cause arthritis. By interacting with cytotoxic CD8 T lymphocytes, they cause lysis of cartilage cells and an inflammatory process. Disorders of heavy chain assembly of the HLA-B27 antigen: proposed in 2000 by RA Colbert et al. According to it, under the influence of polysaccharides of microbial cells, the synthesis of heavy chains of the HLA-B27 antigen is disrupted. This leads to disruption of macrophage activity, reduces the effectiveness of their immune response and destruction of bacterial cells, and can lead to the development of inflammation in the joint. Cytokine hypothesis. Proposed by J. Sieper in 2001. Based on studies showing cytokine imbalance in patients with reactive arthritis. A decrease in the Th1 immune response (production of IF-γ, TNF-α, IL-2 and IL-12) in favor of a Th2 immune response (synthesis of IL-4 and IL-10) was revealed. At the same time, in the macrophages of the synovial fluid, the production of IF-γ and TNF-α decreases and the production of IL-4 increases, which contributes to the persistence of bacteria in the joint. This hypothesis is under development and has not yet been fully formulated. Currently, the concept of reactive arthritis as sterile has lost its relevance. One of the important advances in the study of reactive arthritis at present is that arthritis-initiating microorganisms, in particular chlamydia, disseminate into the joint. Proof of this is the detection of viable chlamydia in the joint membrane and joint fluid by nucleic acid amplification. Despite this, during routine diagnostics it is almost impossible to isolate chlamydia from a joint. It is believed that chlamydia is “recruited” into the joint by the synovial membrane as part of macrophages and dendritic cells. The latter probably stimulate a specific T-cell immune response directly in the joint. This is confirmed by the fact that the synovial membrane consists of 50% macrophages, so that in the joint, as a rule, the capture of certain particles from the bloodstream is inevitable. More often this occurs in large and medium-sized joints (knees, ankles), which are subject to microtrauma as a result of the fact that they bear a supporting load. According to various authors, chlamydia is determined in the joint with subsequent cultivation in developing chicken embryos and in living cells in more than half of the cases (53%). During cultivation, both typical and L-forms are determined. Both of them, therefore, can persist in the synovium.
Clinical picture Joint damage: Develops within a month after the infection. Mostly large joints of the lower extremities (knees, ankles, big toes) are affected on one side. Other joints may also be involved, rarely more than six, and arthritis of the sacroiliac joints (sacroiliitis) and the overlying parts of the spine often occurs. Damage to the tendons: Along with the joints, the tendons, at the place of their attachment to the bone, and the tendon bursae of the toes and hands are often affected with the development of dactylitis. Damage to the mucous membranes: Conjunctivitis - often oligosymptomatic or asymptomatic, short-term. Non-infectious urethritis, annular balanitis, cervicitis, oral erosions, and uveitis may develop. Skin lesions: Keratoderma (keratoderma blennorrhagica) is a painless keratinization of the skin with rashes in the form of papules and plaques, most often on the plantar part of the feet and palms. Nail damage: More often detected on the toes: yellow discoloration, peeling and destruction of the nail. Systemic manifestations: Enlarged lymph nodes, especially inguinal ones. Pericarditis, myocarditis, leading to cardiac conduction disturbances; aortic valve insufficiency, pleurisy, kidney inflammation (glomerulonephritis). Possible development of polyneuritis. Reiter's syndrome Main article: Reiter's syndrome A classic manifestation of reactive arthritis, it combines the “Reiter's triad”: damage to the joints (arthritis, synovitis), eyes (conjunctivitis, uveitis), and mucous membranes of the genitourinary organs (urethritis). In the case of the addition of skin manifestations (keratoderma), it is called “Reiter's tetralogy”. It was first described by Benjamin Brody, and then in 1916 by the German military doctor Hans Conrad Reuther in a soldier who had suffered from dysentery.
Currently considered as a special form of reactive arthritis. The disease begins 2 - 4 weeks after a chlamydial or intestinal infection, most often with damage to the urogenital tract. The most common triggering agents are Chlamydia trachomatis and Shigella flexneri 2a, as well as their combination.
Diagnostics Diagnostic criteria Criteria of the III International Meeting on Reactive Arthritis (Berlin, 1996):
Peripheral arthritis : Asymmetric Oligoarthritis (affects up to 4 joints) Predominantly affecting the joints of the legs Infectious manifestations: Diarrhea Urethritis Occurrence 2-4 weeks before the development of arthritis Laboratory confirmation of infection: In the presence of clinical manifestations of infection - desirable In the absence of obvious clinical manifestations of infection - mandatory Exclusion criteria - an established cause of the development of mono- or oligoarthritis: Spondyloarthritis Septic arthritis Crystalline arthritis Lyme disease Streptococcal arthritis Differential diagnosis Septic arthritis: occurs in the form of monoarthritis. It is characterized by high leukocytosis of synovial fluid (20,000-100,000/μl), positive results of bacterial culture. Viral arthritis can be caused by rubella viruses, parvovirus, adenovirus, hepatitis B virus, herpes viruses of various types, mumps virus, enteroviruses, Coxsackie viruses, etc. History often shows a connection with a viral infection or vaccine. In the clinic, the syndrome is more pronounced: arthralgic syndrome (joint pain) than arthritic syndrome (swelling, hyperemia). Within 1-2 weeks, symptoms disappear without residual effects. Poststreptococcal arthritis : appears against the background or 1-2 weeks after a streptococcal infection, characterized by simultaneous involvement of the middle joints, an increase in the titer of anti-streptococcal antibodies. Patients often have chronic foci of infection in the nasopharynx (tonsillitis, pharyngitis, sinusitis). The effect of NSAIDs may be delayed, and the improvement in laboratory parameters is insignificant. Rheumatoid arthritis : the clinic differs. There are no special markers. With reactive arthritis, inflammation of the tendons occurs and a common symptom is heel pain. It is difficult to differentiate in the case of the onset of oligoarthritis in young people, asymmetry of lesions and seronegativity. A thorough search for trigger infections and dynamic monitoring are required. Ankylosing spondylitis : The only difference is the x-ray of the SIJ (sacroiliac joint) and hip joints: if sacroiliitis is unilateral or absent, then reactive arthritis (RA), and if bilateral, at least stage 2, or unilateral, at least stage three, then Ankylosing spondylitis. But this is not suitable for early diagnosis, since these changes appear only after several years of illness. There is every reason to believe that prolonged reactive arthritis will develop into Ankylosing spondarthritis, and may be considered a certain stage in the development of the disease. Psoriatic arthritis : Difficulties arise when arthritis develops before skin symptoms appear. To exclude reactivity, a search for trigger infections and monitoring over time is carried out. Lyme disease : has a characteristic epidemiological history: stay in endemic areas, tick bite. Antibodies to the genus Borrelia are detected in the blood. Tuberculous arthritis : there are general symptoms of tuberculosis: intoxication syndrome, low-grade fever, autonomic disorders. Joint pain, mainly at night, symptoms of arthritis. The diagnosis is confirmed by x-ray data, analysis of synovial fluid, and biopsy of the synovial membrane. Laboratory diagnostics Mandatory tests include: a general blood test, urine test, detection of chlamydia and antibodies to them, testing for the presence of HIV infection, gonococci, stool testing for Salmonella, Shigella, confirmation of the absence of antinuclear antibodies and rheumatoid factor.
Study for the result: Complete blood count: leukocytosis, increased ESR, normochromic anemia. General urine analysis: possible proteinuria, microhematuria, leukocyturia AT, PCR: often positive for chlamydia AT: positive for gonococci only in case of mixed infection Stool analysis: Possible detection of Salmonella, Shigella Antinuclear AT: Absent Rheumatoid factor: Absent Additional studies include analysis of synovial tissue liquids. Signs of a reliable diagnosis of reactive arthritis are: low viscosity of the synovial fluid, poor formation of a mucin clot, leukocytosis (5000-10,000/μl) with a predominance of segmented neutrophils. Unlike septic arthritis, a decrease in glucose concentration is uncharacteristic.
Instrumental studies Mandatory: X-ray examination of the affected joints. Characteristically: changes can be noticed only with a long course of the disease; it is possible to detect unilateral sacroiliitis, more often in carriers of the HLA-B27 antigen. Gross changes in bone and cartilage, ossifications are uncharacteristic.
Additional : echocardiography (detection of damage to the aortic valves).
Treatment The outcome of the disease is closely related to the destruction (eradication) of the pathogen, which is why long-term use of antibacterial drugs is necessary. The goals of symptomatic treatment are to eliminate pain and inflammation in the joints.
Treatment is usually carried out on an outpatient basis; cases of severe arthritis with systemic manifestations and unclear cases requiring clarification of the diagnosis require hospitalization.
Non-drug treatment A motor regimen is indicated: rest of the affected limb during the first two weeks of the disease, but joint fixation and immobilization are not indicated. Cold on the affected joint. In the future, exercise therapy is prescribed according to an individual plan. There is no need to adhere to a special diet.
Drug therapy 1. Antibacterial therapy is of paramount importance in case of detection of chlamydial infection and is carried out for a long time. There are mainly three groups of drugs used that act on intracellular microorganisms: macrolides, fluoroquinolones and tetracyclines.
Drugs of choice:
Doxycycline 0.3 g per day, orally in 2 doses for 30 days; Azithromycin 1 g per day on the first day, then 0.5 g/day orally for 30 days; Clarithromycin 0.5 g per day, orally in 2 doses for 30 days; Spiramycin 9 IU per day, in 3 doses for 30 days. Second-line drugs (in case of intolerance or ineffectiveness of the above drugs):
Ofloxacin 600 mg per day orally in 2 doses for 30 days; Ciprofloxacin 1500 mg per day, orally in 2 divided doses for 30 days; Lomefloxacin 400-800 mg per day, orally in 1-2 doses for 30 days. In the case of enterocolitis, the effectiveness of antibiotics has not been proven.
2. NSAIDs - have a symptomatic effect: relieve pain and inflammation of the joints.
Diclofenac orally 2-3 mg/kg/day in 2-3 divided doses; Naproxen orally 15-20 mg/kg/day in 2 divided doses; Ibuprofen orally 35-40 mg/kg in 2-4 doses; Nimesulide orally 5 mg/kg in 2-3 doses; Meloxicam orally 0.3-0.5 mg/kg in 1 dose. Without exception, all NSAIDs have a negative effect on the stomach and kidneys! Therefore it is necessary to use the smallest possible dose.
When taking NSAIDs, you should monitor your blood tests to monitor your kidneys and liver. It is also necessary to use drugs to protect the stomach (Omeprozole...)
3. Glucocorticoids - for severe arthritis, they are used for intra-articular administration. A necessary condition is the exclusion of septic arthritis.
4. Immunosuppressors - used for severe and protracted course, signs of spondyloarthritis, high activity of arthritis.
Sulfasalazine 2 -3 / g/day. Methotrexate 7.5-15 mg/week. (Not used in modern treatment of reactive arthritis. Not a drug of choice since it has not shown effectiveness in studies in the group of seronegative spondiarthritis) Azathioprine 150 mg/day (Not used in modern treatment of reactive arthritis. Not a drug of choice since it has not shown effectiveness in studies in the group of seronegative spondiarthritis)
Course and prognosis The duration of the primary case is on average 3-6 months. Symptoms often persist for up to 12 months or more. There is a greater tendency to develop relapses in patients with Reiter's syndrome, both due to the possibility of reinfection and persistence of chlamydial infection.
The outcome of acute to chronic arthritis is observed in 20-50% of patients. In 15% of cases, severe joint dysfunction develops. The most severe course of reactive arthritis occurs in HIV-infected patients.
The period of temporary disability in acute cases is 30-60 days, in subacute cases 35-65 days, in case of exacerbation of chronic cases - 30-35 days.
With a protracted course of reactive arthritis, there is a high probability of its transition to one of the chronic diseases of the group of seronegative spondiarthritis (Ankylosing spondylitis)
Prevention Prevention of reactive arthritis comes down to preventing the infections that cause it: maintaining a hygienic regime regarding intestinal infections, boiling water, washing hands, following the rules of storing and preparing food. People who have a positive HLA-B27 antigen are recommended to take prophylactic antibiotics while traveling (norfloxacin 0.4 g 2 times a day). To prevent chlamydia, protective equipment is used during casual sexual contact.
What to do if the disease worsens
Arthritis of the foot and ankle occurs with painful relapses. In some clinical forms of the disease, exacerbations can be very painful. How to help yourself, reduce pain before the doctor arrives? This can be done like this:
- calm down by taking valerian or motherwort;
- take a tablet of any pain reliever - Analgin, Diclofenac, Ibuprofen, Nise, Paracetamol, etc.; the analgesic effect occurs very quickly after using a rectal suppository with Diclofenac;
- apply pain-relieving ointment (gel, cream), for example, Fastum-gel, to the ankle and foot area;
- call a doctor at home;
- lie on your back on a flat surface and elevate your sore leg, placing a pillow under your shin and heel;
- calmly wait for the doctor to arrive.
Diagnostics
To establish the correct diagnosis, taking into account the origin of the disease, the doctor first asks the patient about the onset and duration of the disease, its symptoms, and diseases of close relatives. Then a thorough examination of the patient is carried out to identify painful areas, the state of the ankle and foot function. The diagnosis is confirmed by laboratory and instrumental studies:
- Laboratory tests
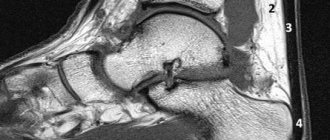
- blood, urine, joint fluid taken by joint puncture (puncture) or during arthroscopy. The following are revealed: the severity of inflammation, the presence of infection, metabolic and hormonal disorders, autoimmune processes. - Instrumental studies
:- Ultrasound
- an increase in the volume of the synovial membrane, the presence of a large volume of exudate; - X-ray of the ankle and foot
– bone changes: narrowing of the joint space, bone growths, deformities; - MRI and CT
are the most informative studies; they reveal any changes; - arthroscopy
- examination of the internal articular surface using optical equipment (arthroscope).
Modern diagnostic methods
Not all doctors can quickly and accurately diagnose reactive arthritis. This is best done by rheumatologists who specialize in joint diseases. The diagnosis can be established after collecting anamnesis and examination. Additionally, the doctor will prescribe blood tests, joint puncture and examination of joint fluid, and x-rays.
Take care of yourself, book a consultation now
Message sent!
expect a call, we will contact you shortly
Treatment of ankle arthritis
How to treat arthritis of the ankle joint in a particular patient is decided by the doctor. The main goal of treating ankle arthritis is to eliminate pain and suppress the progression of the disease. During remission, rehabilitation is carried out to restore the function of the ankle and foot.
Individually selected comprehensive treatment for arthritis of the foot and ankle includes drug therapy, various types of non-drug treatment and folk remedies.
Drug therapy
Drugs for the treatment of ankle arthritis
The selection of medications depends on the clinical form of arthritis of the joints of the foot and ankle, the characteristics of its course, and the presence of concomitant diseases in the patient.
To eliminate pain, inflammation and swelling, medications from the group of non-steroidal anti-inflammatory drugs - NSAIDs (Diclofenac, Nimesulide, Ibuprofen, etc.) are prescribed. Depending on the severity of symptoms, the medicine is prescribed in the form of injections (injections), tablets for oral administration, rectal suppositories (suppositories are not inferior in effectiveness to the injection method), external agents (gels, creams, ointments - Voltaren emulgel, Pentalgin gel).
For severe swelling and pain that is not relieved by NSAIDs, glucocorticosteroid hormones (GCS) are prescribed. They are administered in short intensive courses, which leads to the rapid elimination of swelling. Often, GCS solutions are injected directly into the joint cavity.
The pain syndrome is significantly increased due to muscle spasm. To eliminate it, muscle relaxants (Mydocalm) are prescribed. To improve metabolism in cartilage tissue, chondroprotectors (Chondroxid, Teraflex, Dona) are used. And to activate general metabolism - vitamins and minerals.
Arthritis of the joints of the foot and ankle, which is based on an autoimmune process, is treated with medications that suppress the activity of the immune system. These are drugs of basic therapy (Methotrexate, Sulfasalazine, Leflunomide), as well as drugs from the group of biological agents, which include antibodies and cytokines (rituximab - MabThera, Redditux).
If the cause of arthritis in the joints of the foot and ankle is an infection, antibiotics are prescribed.
Non-drug methods
Treatment of ankle arthritis with non-drug methods includes:
- Immobilization of the ankle and foot in severe inflammatory processes. Currently, for this purpose, the wearing of orthoses is most often prescribed - orthopedic devices that fix the ankle and foot in a certain position. The orthosis effectively reduces the load on the ankle and eliminates additional injury when walking. All this helps restore limb function.
- Physiotherapeutic procedures are included in the complex treatment of arthritis at any stage. Electrophoresis with analgesics and corticosteroids effectively eliminates swelling and pain, laser and magnetic therapy help restore joint function.
- Therapeutic exercise (physical therapy) - prescribed for the treatment of arthritis of the foot and ankle immediately after the elimination of severe pain and swelling, prevents the development of ankylosis. A set of exercises is prescribed by a doctor and mastered under the supervision of a physical therapy instructor. The result of systematic exercise is the restoration of ankle function.
- Massage is carried out at the stage of remission, improves blood circulation, promotes the restoration of joint tissues.
- Reflexology (acupuncture, moxotherapy, acupressure) - perfectly relieves inflammation, pain, and restores the function of the ankle and foot.
Orthosis for immobilization of the ankle joint and exercise therapy exercises for the treatment of ankle arthritis
Traditional methods
Treatment of arthritis of the foot and ankle with traditional methods can be part of a complex treatment as prescribed by a doctor:
- trituration; beat the white of one egg, add a teaspoon of dry mustard (without a slide) and camphor oil, 2 teaspoons of vodka; mix, store in the refrigerator, rub into the ankle and foot area overnight;
- pain-relieving compresses; Dry the elm bark, grind it into powder, add a little water to obtain a mushy mass, put it on a napkin, apply it to the ankle, cover it with plastic on top, insulate it and leave it overnight;
- anesthetic ointment; mix equal volumes of dried and powdered black currant leaves, sweet clover herb, and dandelion root; Mix 10 g of the mixture with 40 g of Vaseline and use it as an anesthetic ointment.
Crunching in joints - when to worry
Intra-articular injections of hyaluronic acid
What is arthritis
A joint consists of an articular capsule, a cavity filled with fluid, and articular surfaces of bones covered with cartilage.
With arthritis, inflammation occurs in the synovium of the joint. Then it spreads to other elements of the joint and periarticular space. The disease leads to changes in the articular cartilage, surfaces, ligaments and capsule. In severe cases, the joint becomes deformed. Arthritis (inflammation of the joints) first affects the hands, feet, shoulders and elbows, and then moves to the knees and hip joints.
Approach to treating the disease at the Paramita clinic
Treatment of arthritis of the foot and ankle in our clinic is carried out after a preliminary examination using modern laboratory and instrumental techniques. After the diagnosis is established, an individually selected comprehensive treatment is prescribed, which includes:
- the latest Western methods of treating this pathology;
- Eastern techniques that restore balance in the functioning of all organs and systems of the body, which helps eliminate the pathological focus.
This approach allows you to quickly eliminate inflammation and pain, suppress the progression of the disease and restore limb function. At the Paramita clinic they will help you even with advanced disease!
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating arthritis
General clinical recommendations
Arthritis of the foot and ankle is a progressive disease. To prevent its relapse, the patient should follow the following recommendations:
- lead a healthy lifestyle, move more;
- regularly perform physical therapy exercises, go swimming;
- avoid heavy physical activity, hypothermia and stress;
- promptly treat all acute and chronic diseases;
- give up bad habits - smoking and alcohol abuse;
- conduct courses of preventive treatment as prescribed by a doctor.
Prevention
To avoid the development of the disease, genetically predisposed persons, as well as persons whose work involves increased stress on the ankles, should avoid provoking factors that can become a trigger for the development of the disease. These are hypothermia, viral infections, prolonged stress and high physical activity.
Follow a diet: give up fried, fatty, spicy foods, sweets and baked goods, eat regularly. The diet should include: low-fat animal products, vegetables and fruits.
If symptoms of foot arthritis appear, you should immediately consult a doctor.
Frequently asked questions about the disease
I dance professionally, but recently my ankle joint has started to hurt on one side. Which doctor should I see?
You can start with a traumatologist. If necessary, he will refer you to another specialist.
Do you join the army if you have ankle arthritis?
If there is persistent impairment of articular function, do not take it.
Patients are often interested in how to treat arthritis of the joints of the foot and ankle. This is the wrong approach. You need to look not for a cure for this disease, but for a clinic that will help you cope with it. The Moscow Paramita clinic has everything necessary to help any patient with ankle arthritis. Contact us, you won’t regret it!
Literature:
- Grazhdanov K.A., Barabash A.P., Barabash Yu.A., Kauts O.A., Zuev P.P. Technology of treatment of purulent arthritis of the ankle joint // Modern problems of science and education. – 2021. – No. 3.
- Martinovich AB, Infected injuries and post-traumatic deformities of the ankle joint. // Diss. Candidate of Medical Sciences Minsk 1990. - P. 128.
- Perez Busquier M., Calero E., Rodriguez M. et al. Comparison of aceclofenac with piroxicam in the treatment of osteoarthritis. Clin Rheumatol 1997;16(2):154–9.
- Kornasoff D., Frerick H., Bowdler J. et al. Aceclofenac is a well-tolerated alternative to naproxen in the treatment of osteoarthritis. Clin Rheumatol 1997;16(1):32–8.
Themes
Arthritis, Joints, Pain, Treatment without surgery Date of publication: 12/14/2020 Date of update: 04/03/2021
Reader rating
Rating: 4.71 / 5 (7)
Can arthritis be treated conservatively?
Almost all reactive arthritis, as well as some types of infectious and post-traumatic arthritis, can be treated conservatively. But not all.
The accumulation of a large amount of exudate during purulent arthritis requires a therapeutic puncture. During the procedure, doctors remove pus and inject antibiotics into the synovial cavity. In the absence of positive dynamics, experts are considering more radical methods of surgical treatment (arthrodesis, endoprosthetics).
Surgery may be necessary for severe post-traumatic arthritis, which has led to the development of deforming osteoarthritis. In such cases, there may be a need for endoprosthetics or even arthrodesis.