Author
: Grachev Ilya Illarionovich
Editor
: Efremov Mikhail Mikhailovich
Date of publication: 10/20/2014 Date of update: 02/13/2020
One of the most striking manifestations of rheumatism is rheumatic polyarthritis, otherwise called reactive. This disease is an inflammatory disease of the joints with further damage to internal organs or tissues, which significantly limits a person’s performance and becomes a serious reason for promptly seeking qualified medical help.
Symptoms of rheumatic arthritis
The main symptom indicating the appearance and development of the disease is the gradual damage to all joints. The most commonly affected areas are the hands, feet, ankles and wrists. An aching feeling of heaviness appears, the joints swell and swell. Other signs:
- Local increase in temperature, which is accompanied by impaired flexibility and mobility of joints
- Deformation of fingers
- When the form is advanced, there is acute pain that makes it impossible to move.
Crunching in joints - when to worry
Joint pain at rest
How does rheumatoid arthritis occur?
Rheumatoid polyarthritis occurs due to a malfunction in the immune system.
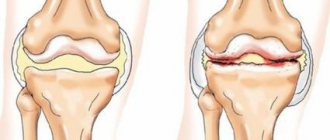
Immune cells mistake joint cells for viruses and bacteria, attack them and try to destroy them. This process lasts for years. Rheumatoid polyarthritis destroys the elements of the joint: synovial membrane, articular cartilage, articular capsule. Erosion appears on the articular surfaces of the bones. Over time, the joint becomes deformed and collapses without treatment.
The trigger for the onset of the disease can be hypothermia, acute respiratory infections, flu, sore throat, joint injuries, stress and prolonged experiences. The appearance of polyarthritis is provoked by infection: immune cells can “attack” microbes and viruses that remain in the joints after an infection.
Relatives of patients with rheumatoid polyarthritis have a 16-fold greater risk of developing the disease. During pregnancy, the risk of getting sick decreases.
Diagnosis of rheumatic arthritis
To identify reactive polyarthritis, it is very important to contact the specialists of our clinic at the first suspicion of the disease to undergo an MRI, pass the necessary tests and receive qualified advice from experienced doctors. After diagnosing the disease, you should begin to restore blood supply to the damaged vessels, simultaneously eliminating the root cause of the disease.
Treatment of rheumatic arthritis at the Paramita clinic
It is very important to begin treating rheumatic arthritis at the earliest stages, until lost ability to work can be restored. At the Paramita clinic, to eliminate this ailment, specialists use the following methods of oriental medicine:
- Jiu therapy – promotes relaxation and healing of sore joints
- Acupressure – affects biologically active points, improves blood flow to the joints
- Herbal medicine – has an immunomodulatory, anti-inflammatory and healing effect
- Pharmacopuncture – improves metabolic processes and strengthens the immune system
- Acupuncture – relieves pain and reduces swelling and inflammation
- PRP therapy is the latest method of stimulating regenerative processes. It is used to restore the functions of various organs after diseases and injuries, including to restore the function of the musculoskeletal system in polyarthritis.
Sign up for a free initial appointment
Epidemiology, features, pathogenesis, causes
The prevalence of rheumatoid arthritis in various regions of the former USSR varies within small limits and on average is about 1% of the surveyed population (M. G. Astapenko, T. M. Pavlenko, 1966). In Ukraine, such epidemiological studies were carried out by A.P. Oleksa (1972) in three western regions: from the high-mountain Carpathians (Dolina) to the low-lying, high-water Volyn (Lyuboml). Following Kellgren's tests, there was no difference in the incidence of rheumatoid arthritis in the population (1.25 per 1000) in these geographic areas.
A feature of rheumatoid arthritis is its progressive course, leading to severe disability, which ranks first among the primary disabilities of all diseases of the support and movement apparatus (23%).
The pathogenesis of the disease consists of systemic progressive damage to connective tissue (disorganization of mainly its basic substance) with frequent localization of the process in the joints.
The causes of the disease have not yet been fully elucidated. Most experts are supporters of the infectious-allergic theory, which explains the cause as a special allergic condition of the body, which is caused by hypersensitization by the breakdown products of bacterial or viral proteins, as well as their endotoxins. The disease is associated with streptococcal infection, which is predominantly localized in the nasal pharynx and oral cavity (carious teeth, sore throats, etc.). However, the source of infection can only be a trigger for the occurrence of sensitization and disruption of the body’s immunological reactivity, manifested by arthritis. The further course of the disease is determined by the degree of reactivity of the body and dysfunction of various systems and metabolism.
Autoimmune and autoaggressive processes occur in the synovial membrane of the joint capsule, in the vessels located near them, which is manifested by massive cellular infiltration and changes in the vascular bed of the membrane. This leads to impaired microcirculation, increased vascular permeability and progressive disorganization of connective tissue, exudative-dystrophic and sclerotic changes in tissues.
Diagnosis of rheumatic arthritis
Diagnosis in our clinic for rheumatic arthritis is carried out in 2 stages.
The first includes eastern methods that allow you to determine the general state of health and the exact location of the problem:
- Pulse diagnostics. Determines the functional state of all systems and organs.
- Load tests. Identify functional changes in the body.
The second stage of diagnosis is carried out using traditional methods:
- General blood analysis. It is carried out to confirm the presence of an inflammatory process in the body.
- Radiography. Makes it possible to detect bone growths and narrowing of the joint space.
- MRI. Allows you to identify the disease at its initial stage.
- ECG. It is carried out to assess the degree of influence of pathological changes on the cardiovascular system.
Rheumatoid arthritis
Rheumatoid arthritis (rheumatoid polyarthritis) is an autoimmune disease in which the synovium is attacked and destroyed by cells of the immune system, causing inflammation.
The pathology affects a large number of joints. The metacarpophalangeal and medial joints of the fingers, wrists, and metatarsophalangeal joints on both sides of the body are often affected.
Women are three times more likely to have this disease than men. The disease can occur at any age, but most often begins after 50 years in women and 10 years later in men. The disease in children is called juvenile rheumatoid arthritis.
Causes
Most often, the causes of this condition are genetic factors. Viruses or bacteria are also suspected. However, there is no convincing scientific evidence. In any case, in addition to hereditary factors, environmental influences also play a very important role. Studies have shown that smokers have an increased risk of developing pathology and severe symptoms. More is known about the inflammatory process in the joint. The immune system plays a major role in this. In rheumatoid arthritis, immune system cells attack the body's own tissues. This causes inflammation of the joints. Doctors call such an attack on one’s own body an autoimmune reaction.
Symptoms
Nonspecific symptoms appear at the initial stage of the disease:
- fatigue,
- states of exhaustion,
- lack of appetite,
- weight loss,
- fever, temperature rise up to 38.
Musculoskeletal symptoms
Typical symptoms in the musculoskeletal system of varying intensity:
- Morning stiffness and joint pain. Fingers are usually affected. Symptoms may persist for up to several hours, after which improvement occurs.
- Inflammation of the joints - swelling, overheating, severe pain in the second half of the night. The pain intensifies from pressure on the joint and with maximum flexion and extension of the joint. Typically, the metatarsophalangeal and median joints of the fingers, wrists and metatarsophalangeal joints of the toes are affected on both sides of the body, and later the inflammation also spreads to other large and small joints (polyarthritis). A noticeable deformation of the joints appears and their mobility decreases.
- Symptoms of tendinitis (tenosynovitis) appear - swelling and pain in the hand and ankle. Damage to nearby nerves can cause carpal tunnel syndrome, which causes numbness in one of the fingers;
- Decreased grip strength: This is often noticed early by patients and leads to increased difficulty in daily activities such as screwing on jam jars.
- Rheumatoid nodules: On the extensor sides of the joints, especially the elbows and hands, but also on the Achilles tendon and the front of the leg, benign, hard and partially mobile nodules appear that develop under the skin or directly on the tendons.
As the disease progresses, typical joint deformities develop, and in rare cases, rheumatoid arthritis can also affect other organ systems. Rheumatoid arthritis increases the likelihood of certain other diseases. These additional ailments can burden patients in their daily lives and, in certain circumstances, even shorten their life expectancy. These include:
- atherosclerosis (“vascular calcification”);
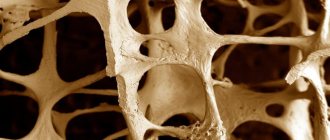
- osteoporosis (bone loss);
- chronic generalized pain syndromes;
- infections;
- depression and anxiety disorders;
- lymphoma (malignant diseases of certain immune cells).
Indications for visiting a rheumatologist
To effectively treat rheumatoid arthritis, prompt diagnosis is important. Only early therapy—within three months from the onset of the first signs of the disease—can prevent irreversible damage and secondary diseases.
The doctor makes a diagnosis based on a medical history, including symptoms (location and duration of joint pain and joint swelling in the family) and the results of a physical examination. Indications for early rheumatoid arthritis include:
- Swelling in more than two joints for six weeks or longer
- Symmetrical arrangement of the affected joints, that is, both halves of the body are affected
- 60 minutes or longer of persistent morning stiffness
Diagnostics
Physical examination includes all joints (not just the affected ones) for swelling, tenderness, functional impairment, rheumatoid nodes, as well as signs of organ damage and associated diseases.
Blood analysis
Based on measurable elevated levels of inflammation in the blood (erythrocyte sedimentation rate (ESR), C-reactive protein, it is possible to estimate how actively the disease is developing. However, these values are often normal at the onset of the disease and, on the other hand, are also increased in other chronic and acute inflammation or infections.
About 85 percent of patients have rheumatoid factors and/or anti-citrullinated protein/peptide antibodies (ACPA) in their blood. These are autoantibodies, that is, antibodies directed against certain endogenous substances. Rheumatoid factors are considered to be relatively nonspecific since they also occur in the normal healthy population during adulthood. On the contrary, antibodies are very specific. With a certain level of antibodies, there is a high probability that rheumatoid arthritis is already present or will develop in the next few years.
Hardware Research
X-rays of the affected joints, hands, and feet are usually taken to visualize the joint changes characteristic of this disease. Typical changes are bone defects on the outer edge of the articular surfaces, a lack of calcium salts in the bone near the joint (osteoporosis) and joint displacements.
With the help of ultrasound, inflammatory changes in the joints, optic nerve sheaths and bursa can be well assessed. Ultrasound can provide additional information about the joints, such as the occurrence of joint effusions (increased fluid accumulation in the joint), the extent of rheumatic tissue that has formed, and joint destruction.
Rheumatoid arthritis treatment
Therapeutic approaches are numerous and range from purely symptomatic painkillers and anti-inflammatory drugs to basic therapy that slows the progression of the disease, from physical therapy to surgery on the affected joints. An appropriate diet may also help reduce symptoms.
Treatment options for rheumatoid arthritis have expanded significantly over the past few years. The goal of therapy is to completely suppress symptoms or stop the disease if possible. The rheumatologist designs a therapy tailored to the patient's individual case.
Drug therapy
The most important thing in therapy is that the patient tolerates well the so-called basic drugs, which affect the immune system and slow down the destruction of joints, and in the best case, completely suppress it. The effect of the medications does not appear immediately, but only after a few weeks. If the disease begins with a large number of inflamed joints, glucocorticoids are used. They very quickly fight inflammation, and with it pain and swelling of the joints.
Non-drug therapy
- Physiotherapy - helps strengthen muscles, prevent joint stiffness and thus ensure joint flexibility. Orthotic devices such as insoles, crutches or splints can also make daily life easier for patients.
- A healthy diet can also influence the course of the disease. A healthy diet is small amounts of red meat, lots of fish, vegetables and fruits.
- Patients with rheumatoid arthritis should make lifestyle changes. This involves doing as much physical movement as possible to keep your joints mobile.
- Overweight people should aim for a normal body weight, and smokers should quit smoking.
Exercises for rheumatic arthritis
A very important point in therapy for rheumatoid arthritis is regular exercise therapy.
Damaged joints need to be loaded gradually, so exercise therapy includes 2 main stages:
- Preparatory. Lasts several days. Its purpose is to prepare the patient for subsequent stress. The duration of classes does not exceed 15 minutes.
- The main one. It is carried out to restore joint mobility and strengthen the musculoskeletal system. Duration: 14 days, 30 minutes per day.
Gymnastics should not be used without the advice of a doctor, otherwise it may aggravate the course of the disease. The clinic’s doctors describe in detail the treatment program for each patient.
Prevention of relapses of seropositive arthritis
To live without exacerbations in a state of stable remission, the patient must:
- be aware of triggers and avoid them;
- lead a healthy lifestyle, engage in exercise therapy;
- eat properly regularly, monitor your weight;
- Be sure to regularly observe a doctor and, on his recommendation, take courses of anti-relapse therapy.
Well, if an exacerbation does begin, run to the doctor! At the Moscow clinic "Paramita" they know a lot about the treatment of seropositive rheumatoid arthritis!
Literature:
- Nasonov EL, Karateev DE, Balabanova RM. Rheumatoid arthritis. In the book. : Rheumatology. National leadership. Ed. E. L. Nasonova, V. A. Nasonova. Moscow: GEOTAR-Media; 2008. pp. 290–331.
- Nasonov E.L., Mazurov V.I., Karateev D.E. and others. Draft recommendations for the treatment of rheumatoid arthritis of the All-Russian public organization “Association of Rheumatologists of Russia” - 2014 (part 1). Scientific and Practical Rheumatology 2014;52:477–94.
- Molina JT, Garcia FJB, Alen JC, et al. Recommendations for the use of methotrexate in rheumatoid arthritis: up and down scaling of the dose and administration routes. Rheumatol Clin 2015;11:3-8.
- Tornero Molina J, Calvo Alen J, Ballina J, et al Recommendations for the use of parenteral methotrexate in rheumatology. Reumatol Clin 2021. pii: S1699-258X(16)30162-0.
- Espinosa F, Fabre S, Pers YM. Remission-induction therapies for early rheumatoid arthritis: evidence to date and clinical implications. Ther Adv Musculoskelet Dis 2016;8:107-18.
Themes
Joints, Pain, Treatment without surgery Date of publication: 04/10/2020 Date of update: 11/12/2020
Reader rating
Rating: 5 / 5 (3)