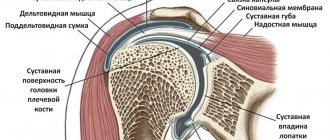
Shoulder joint
– one of the most mobile joints in the human body. The structure of this joint makes it possible to carry out various movements of the upper limbs in a wide range: rotational, flexion, abduction, extension and adduction actions.
Description of the disease
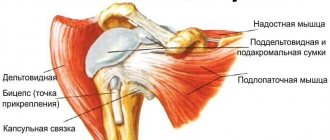
Rotator cuff
– anterior outer part of the capsule of the shoulder joint. It combines the tendons of the supraspinatus, infraspinatus, and teres minor muscles. Despite the difference in the functions they perform, such an anatomically close location of fixation of the muscles allowed traumatologists to identify them in a common group (the rotator cuff).
Damage to the rotator cuff can be considered a rupture of one or a group of tendons that make up its composition. Most often this is caused by injury, dislocation or previous chronic inflammatory process.
Our doctors
Samilenko Igor Grigorievich
Traumatologist - orthopedist, doctor of the highest category
24 years of experience
Make an appointment
Marina Vitaly Semenovich
Traumatologist-orthopedist, head of the minimally invasive traumatology and orthopedics service
Experience 36 years
Make an appointment
Zubikov Vladimir Sergeevich
Traumatologist-orthopedist, Doctor of Medical Sciences, doctor of the highest category, professor
44 years of experience
Make an appointment
Poltavsky Dmitry Ilyich
Traumatologist-orthopedist
Experience 28 years
Make an appointment
What Causes Rotator Cuff Injury?
As mentioned above, the most common cause of rotator cuff injury is trauma. Most often, ruptures occur in older people, but in young people, ruptures can also occur due to serious injuries, such as a fracture of part of the humerus or dislocations.
- A fairly common cause of rotator cuff injury is permanent tendon injury
, which is chronic. This mainly applies to people whose professional activities involve heavy physical labor. Tension and heavy stress on the joints, accompanied by repeated motor operations, leads to chronic inflammation and pain.
- Spontaneous tendon rupture or damage is usually preceded by period of degenerative-dystrophic changes
. Lack of blood supply is the main cause of tissue degeneration or tendinopathy. Many doctors attribute genetic predisposition to another possible reason for the development of degeneration.
- Another reason may be individual anatomy
. Sometimes, insufficient space between the head of the humerus and the tip of the scapula leads to constant friction and injury to the rotator cuff tendons. In addition, the hook-shaped shape of the acromion process and the presence of an accessory bone at the tip of the scapula that damages the tendons are anatomically determined.
Causes of tenosynovitis
There are many causes and factors for the development of inflammation. These include:
- Wound and injury to the tendon. In the absence of infection in the injury, the wound heals faster and less painfully. In case of infection penetration, the treatment period increases, requiring medication. During the disease with tenosynovitis, the patient experiences loss of motor ability of the limb. However, after recovery, this ability is fully restored.
- Rheumatic disease. Occurs when immunity decreases, since the body is unable to resist infection that has penetrated the outer shell of the tendon.
- Joint degeneration. Diseases such as bursitis often affect tendons.
- Genetic predispositions.
- Infectious diseases. In the case of tuberculosis, HIV, syphilis, herpes, etc., the infection is spread throughout the body by the bloodstream.
Symptoms of a rotator cuff tear
The rupture is always accompanied by a sharp attack of pain localized in and around the shoulder joint. The pain often radiates to the hand, neck and forearms. A characteristic symptom is increased pain when trying to make a certain movement with the arm, for example, lift it or move it to the side. In some cases, patients are completely unable to move their arm. The individuality of symptoms and the degree of their severity depends on whether the rotator cuff tear was complete or partial. Patients also very often complain of the inability to sleep on the side where the joint is damaged.
The location where the center of pain is located directly depends on the location of the damaged tendon. The most common rupture in clinical practice is the rupture of the supraspinatus tendon. This case can be diagnosed by asking the patient to move his arm to the side. If we are dealing with just such damage, the patient will not be able to complete this task. If abduction of the arm is possible, but pronounced pain is felt, it is most likely that the tendon is not completely torn, but only severely damaged.
Symptoms of tenosynovitis
The development of symptoms and signs of this disease occurs gradually. Initially, a person feels slight discomfort in the joint. Most do not pay attention to this, since people consider it a temporary phenomenon associated with the load on the limb. Since the transition from acute to chronic tenosynovitis occurs very quickly, the appearance of any of these symptoms is a reason to go to the doctor:
- Pain of any kind (acute, dull, prolonged, etc.).
- The appearance of a tumor, visible or palpable.
- Stiffness in joint movement.
- Redness in the tendon area.
- Increased pain during movement.
Diagnosis of rotator cuff injuries of the key joint
In order to make a correct diagnosis, the doctor carries out a set of measures to establish the clinical picture.
- The first method is patient interview
: the doctor needs to establish the circumstances under which the pain appeared, determine how long ago the patient experienced discomfort in this area and ask about the nature of his professional activity.
- Then you need thorough examination using specific tests
. In this way, the level and severity of the pain syndrome, the degree of weakness of motor function and the condition of the adjacent muscles are determined. Typically, a complete rupture has a number of pronounced symptoms, so it can be diagnosed without difficulty.
Below are several diagnostic tests to help your doctor understand the nature of your shoulder injuries.
Painful Dawborn arch
The arm is passively and actively retracted from the initial position along the body.
Grade
. Pain occurring during abduction between 70° and 120° is a symptom of damage to the supraspinatus tendon, which is compressed between the greater tuberosity of the humerus and the acromion process during this phase of movement (“subacromial impingement”).
Test of arm abduction from zero position
The patient stands with his arms down and relaxed. The physician grasps the distal third of each patient's forearm with his or her hands. The patient tries to spread his arms, while the doctor resists.
Grade.
Abduction of the arm is carried out by the supraspinatus and deltoid muscles. Pain and especially weakness during abduction and deviation of the arm strongly confirm a rotator cuff tear.
An eccentric position of the humeral head in the form of its superior displacement during a rotator cuff tear occurs due to an imbalance in the muscles surrounding the shoulder joint. Partial ruptures, which can be functionally compensated, impair function to a lesser extent with the same severity of pain. Complete ruptures are invariably characterized by weakness and loss of function.
Jobe Supraspinatus Test
This test can be performed with the patient standing or sitting. With the forearm extended, the patient's arm is placed in a position of 90° abduction, 30° horizontal flexion and internal rotation. The examiner resists this movement by applying pressure to the proximal humerus.
Grade.
If this test causes significant pain and the patient is unable to independently hold the arm abducted to 90° against gravity, this is called a positive drop arm sign. The upper portions of the rotator cuff (supraspinatus) are assessed primarily in the position of internal rotation (the first finger looks down), and the condition of the anterior portion of the cuff is assessed in the position of external rotation.
Falling hand test (symptom of falling flag, chess clock)
The patient sits, the doctor passively abducts the patient's extended arm approximately 120°. The patient is asked to independently hold his hand in this position, and then gradually lower it.
Grade.
Inability to hold the arm in this position with or without pain, or a sudden drop of the arm confirms a rotator cuff injury. The most common cause is a defect in the supraspinatus muscle. With pseudoparalysis, the patient cannot independently lift the injured arm. This is the main symptom confirming rotator cuff pathology.
External rotation abduction test for infraspinatus tendon rupture
The patient's arm is placed in a position of 90° abduction and 30° flexion. In this position, the action of the deltoid muscle as an external rotator is eliminated. The patient is then asked to begin external rotation, which the doctor prevents.
Grade.
A decrease in active external rotation in the abducted position of the arm is characteristic of clinically significant injury to the infraspinatus tendon.
Next, the patient is required to receive a referral for an x-ray. With the help of an X-ray examination, the doctor obtains a picture typical of a particular case. Unfortunately, the gap is not clearly defined; only a number of indirect signs can indicate it. The most informative diagnostic method today is magnetic resonance imaging. It can be used to visualize the tendons, muscles and ligaments of the shoulder joint. This method provides the clearest and most vivid picture of the condition of the patient’s soft tissues.
Examination methods
- MRI (magnetic resonance therapy). This examination technique is the most informative to date. This is due to the fact that it allows you to obtain a complete clinical picture of the condition of the soft tissues. Thanks to MRI, the doctor can visualize not only the tendons, but also the ligaments and muscles of the shoulder joint.
- Radiography. This examination does not allow visualization of soft tissue. It is prescribed to confirm or refute the fact of a limb fracture.
If necessary, other examinations may be prescribed. Thanks to them, the doctor receives a complete picture and can decide on further therapy.
Treatment options for rotator cuff tears
The very first action of the doctor will be measures to relieve pain: usually, these are anti-inflammatory painkillers and ointments. It is recommended to completely rest the injured arm and fix it using a bandage or abduction splint. Applying cold, such as an ice pack, will help relieve swelling.
Surgery
A complete rupture of the cuff cannot heal on its own, and therefore immediate surgical intervention is required so as not to lose the motor function of the joint. In this case, it is important to perform the operation as early as possible, because an old injury leads to shortening of the muscle and the inability to stretch it to its original length. In such cases, it is very difficult to return the tendon to its place and will require a lot of effort from the surgeon. The optimal period for performing the operation is several months from the moment of rupture.
During surgery, the damaged tendon is stretched, attaching it to its original position, and also sutured, if necessary. All lifeless tissue that has undergone degeneration is removed so that the tendon can better adhere to the site of artificial attachment. Anchors are mainly used to attach the tendon. The anchor is screwed into the area of the bone where the soft tissue will subsequently be connected. The sutures attached to the anchor are passed through the rotator cuff and pulled to the bone using interrupted sutures. Thus, the sutures hold the tissue until the tear sites heal completely. Surgery to restore the function of the rotator cuff can be called quite complex and is performed through an incision.
Arthroscopic treatment
Arthroscopy is the most progressive method of surgical treatment of rotator cuff tears. It is performed without an incision by creating a special puncture with a diameter of 1-2 centimeters. A camera, an arthroscope, is inserted into the joint through the puncture cavity, allowing the surgeon to see a clear picture of the internal space of the joint. The image obtained from the surface of the arthroscope is transmitted to a screen, looking at which the surgeon carries out all the necessary manipulations and simultaneously controls them.
An operation performed in this way is most preferable, since healing occurs much faster, and the tissues surrounding the joint are practically not damaged during the intervention. After surgery, the patient's arm is immobilized for several weeks by applying a splint. This will protect against the possibility of re-rupture and allow the tissues to heal after surgery.
Rehabilitation after injury
Rehabilitation after this injury cannot be called quick: as a rule, it can take from 3 to 6 months. The load on the damaged joint must be accurately dosed so as not to disrupt the healing process.
Special exercises and restorative gymnastics are indicated as rehabilitation. Developing the joint should begin with passive movements. Active exercise may not be allowed until 6 weeks after surgery. Physiotherapy is prescribed to relieve tissue swelling and pain after surgery.