Pyrophosphate arthropathy is a chronic, ever-evolving disease of the musculoskeletal system. The disease is associated with the fact that small crystals consisting of calcium and phosphorus salts begin to be deposited in the cartilage tissues of the joint. Microcrystalline arthritis causes severe pain and limited functionality. With severe dysmetabolic syndrome, secondary osteoporosis may develop and there may be a risk of increased bone tissue trauma.
Gradual deposition of calcium leads to calcification of soft tissues. The first to be affected are the cartilaginous synovial membranes of the bone heads. Chondrocalcinosis is characterized by a pronounced process of replacement of hyaline cells with microcrystals of calcium pyrophosphate. Subsequently, other periarticular soft tissues are also affected.
At the initial stage, pyrophosphate arthropathy manifests as an attack of gout. But when carrying out differential diagnosis, completely different clinical signs are discovered. There are no subcutaneous nodules. Calcifications and degenerative changes in cartilage tissue are detected. An X-ray image shows the spread of bone shadows on tissues that are not characterized by calcification.
Basic clinical guidelines for pyrophosphate arthropathy can be found in this resource. Here we talk about the symptoms and causes of the disease. General information about differential diagnosis and complex treatment of pathology is also given.
Pyrophosphate arthropathy is often diagnosed in older people. If in young people under the age of 40 more than 5 cases per 1000 examined patients are detected, then at the age of 70 this pathology is detected in 45% of patients. It is extremely rare that the deposition of calcium salts in the joints is detected in people under the age of 30 years.
In women, chondrocalcinosis occurs as a chronic subacute process with a sluggish course and rare exacerbations. In men, pathology always leads to the primary development of acute arthritis of unspecified etiology. With chronic development, periods of exacerbation are accompanied by impaired mobility and severe pain.
How does pyrophosphate arthropathy develop?
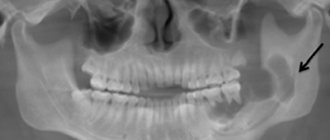
Let's look at the process of how pyrophosphate arthropathy develops. This process affects the middle layer of cartilage fibers. When calcified, it loses its ability to perform shock-absorbing function and quickly undergoes destruction. When conducting an X-ray examination in the advanced stage of pathology, a scattering of “pearls” of a fairly regular round shape is visible in the projection of the cartilaginous layer of the synovial membrane of the head of the bones. These are calcium pyrophosphate deposits.
Gradual replacement of chondrocytes and destruction of the cartilage tissue matrix tends to develop deforming osteoarthritis. This disease aggravates the course of chondrocalcinosis.
The appearance of crystals of calcium salts in the thickness of cartilage that is normal in structure can be provoked by the following pathogenetic factors:
- disturbance of diffuse metabolism with surrounding muscle tissue due to a sedentary lifestyle;
- stagnation of lymphatic and intercellular fluid, disruption of blood microcirculation leads to sedimentation of calcium salts with subsequent penetration into the thickness of the tissue;
- disturbance of the biochemical balance of blood with excess calcium levels;
- age-related hormonal changes in the body, which lead to calcium being gradually washed out of bone tissue and deposited in the form of calcifications in soft tissues in the human body.
After calcium pyrophosphate crystals penetrate into the thickness of the cartilage tissue, the process of inflammation begins, followed by the formation of erosion and lacunae. These hidden cavities are filled with salt deposits. Osteophytes appear. They disrupt the blood supply to the subchondral endplates. As a result of partial degeneration of cartilage tissue and cracking, the pathological process of destruction of the tissue of the heads of the bones begins.
When cartilaginous synovial tissue is completely encrusted with calcium salts, it loses its shock-absorbing ability. When squeezed, it does not release liquid, but cracks. There is no subsequent expansion with the absorption of joint fluid.
The primary symptom complex of the disease always includes signs of acute synovitis (inflammation of the synovial fluid inside the joint capsule). With this disease, differential diagnosis is always required to exclude pyrophosphate arthropathy.
Magazine "Child's Health" 5 (26) 2010
Crystalline arthropathy in children is detected extremely rarely due to the lower severity of metabolic disorders and the presence of only initial manifestations of secondary changes in the musculoskeletal system. Most often they manifest themselves as pain in the joints of the so-called mechanical nature. With this nature of the pain syndrome, arthralgia is absent at rest, appears only with relatively long walking (or standing) and subsides during rest; pain in the anterior part of the knee joint is typical when walking up stairs, over rough terrain, or getting up from a low seat. A change in the rhythm of pain to an inflammatory one indicates the addition of synoviitis or periarthritis [1].
According to the ICD 10th revision, crystalline arthropathy belongs to the group of inflammatory arthropathy of non-infectious origin and includes gout (M 10) and other crystalline arthropathy (M 11):
— hydroxyapatite deposits (M 11.0);
- hereditary chondrocalcinosis (M 11.1);
- other chondrocalcinosis (M 11.2);
— crystalline arthropathy, unspecified (M 11.9).
Their prevalence in adults is: gout - 1–28 per 1000; varies for different regions and gender; for other crystalline arthropathies it is precisely unknown [2].
The mechanism of development of the pathological process leading to the occurrence of lesions of the musculoskeletal system in crystalline arthropathy is complex.
If in gout the formation of urate crystals occurs in the synovial fluid or in extra-articular tissues (formation of tophi) against the background of a general increase in the level of uric acid in the tissue fluid, then in pseudogout and other crystal arthropathies the primary zone of crystal formation is the thickness of hyaline or fibrous cartilage or periarticular structures in normal the level of calcium in other tissues of the body [3, 4].
Typical morphological signs preceding pathological mineralization are hypertrophy of chondrocytes and their increased apoptosis. In hypertrophied chondrocytes, altered proteoglycans and shortened collagen chains are synthesized, the production of matrix metalloproteinase-13, alkaline phosphatase, and transglutaminase changes, which contributes to the development of secondary destructive changes and an inflammatory reaction. Genetic factors also play a certain role in pathogenesis [5].
In adults, the cause of salt deposition in joint-forming tissues is most often a disorder of purine metabolism, manifested by an increase in the content of uric acid in the blood and tissues - gout. The diagnosis of gout is practically not established in childhood. At the same time, according to the clinical register of the department of connective tissue diseases in children of the State Institution "IPAG AMNU", the presence of hyperuricemia is noted in 4.9% of cases when examining children with complaints of arthralgia, even without signs of inflammatory changes in the joints. The causes of identified uricemia can be secondary, caused by endocrinopathies, autoimmune diseases, taking certain medications, but they can also be initial gouty disorders, which clinically manifest only decades later [1, 2].
A pediatrician may be led to believe that there is a violation of mineral metabolism in a patient with complaints of pain in the joints by the detection of lime deposits in the tissues, most often detected during an X-ray examination.
The main cause of local calcification is tissue changes that promote the absorption of calcium salts from the blood and tissue fluid due to alkalization of the environment and increased activity of tissue enzymes. Lime deposits in tissues can also occur due to non-metabolic causes - in tuberculous foci of necrosis; gummah; in case of heart attacks at the site of dead cells; in foci of chronic inflammation. These causes must be excluded first when local deposits of calcium salts are detected in patients [6–8].
Areas of tissue calcification are typical of both gout and pseudogout. Today, two varieties of the latter are known, based on different metabolic defects [9].
The first type of pseudogout is pyrophosphate arthropathy (chondrocalcinosis), which practically does not occur in childhood and occurs in the form of attacks of acute arthritis resulting from subchondral deposition of calcium pyrophosphates (Ca2(P2O7)2H2O). Such deposits can occur in many joints, but the clinical significance is mainly in the knee joints. Pediatricians, however, need to remember about other possible causes of deposition of calcium pyrophosphate salts, for example, those observed with hemochromatosis.
Pyrophosphate arthropathy occurs in the form of pseudoosteoarthrosis, pseudorheumatoid form, pseudogouty variant, pseudoneuropathic arthropathy, asymptomatic chondrocalcinosis, which determines the spectrum of differential search.
Often with this disease, changes in skeletal muscles, tendons, ligaments, and synovial bursae are detected at the places of their attachment to the bones, mainly on the medial side of the knee joint. The pain in these cases is very severe, leading to lameness, and often persists at rest. In diagnosis, palpation and testing with isolated muscle tension are of primary importance. The diagnosis can be confirmed by ultrasound examination of tissues and identification of pyrophosphate crystals in the synovial fluid.
The cause of radiating pain in the knee joint with chondrocalcinosis may be changes in the hip joint. Therefore, for “unexplained” pain in the knee joint, an X-ray examination of the entire femur and hip joint is recommended.
Radiological features of pyrophosphate arthropathy include significant narrowing of the joint space in combination with osteosclerosis, especially when identifying an isolated lesion of the femoral-patellar joint or lateral femorotibial joint, the presence of intra-articular bodies of varying degrees of density, pronounced flattening of the medial or lateral surface of the tibial condyle [6] . The pathognomonic signs of pyrophosphate arthropathy are chondrocalcinosis (calcification of the menisci and articular cartilage). Pyrophosphate arthropathy affecting the knee may not be accompanied by clear calcification of the menisci or articular cartilage. In these cases, the diagnosis is established by detecting calcium pyrophosphate crystals in the synovial fluid.
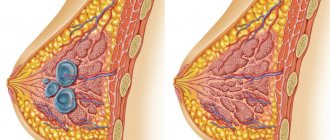
The second type of pseudogout is calcium phosphate deposition disease, in which calcium hydroxyapatite crystals are deposited primarily in the tendons and subcutaneously [10].
According to X-ray examination, the diagnosis of hydroxyapatite arthropathy is established in the following cases:
— multiple calcification of periarticular structures (with the exception of systemic scleroderma, dermatomyositis, mixed connective tissue disease, which can also be accompanied by the formation of calcifications);
- recurrent attacks of acute periarthritis, especially when calcification is detected in the tendon, decreasing or disappearing after the attack;
- exclusion of septic arthritis, Charcot neuroarthropathy, rheumatoid arthritis.
Hydroxyapatite, deposited in the periarticular tissues during pseudogout of the second type, is a mineral compound with the formula Ca10(PO4)6OH. Its crystals form in initially damaged tissue, which explains the fact that frequently injured and poorly vascularized areas of tendons are primarily affected by calcification Therefore, the area of the supraspinatus tendon near its attachment to the greater tubercle of the humerus is a favorite localization [6]. In turn, calcification contributes to the further progression of degenerative changes and the development of a secondary inflammatory reaction due to increased secretion of cytokines and proteolytic enzymes by phagocytes after their absorption of crystals. General predisposing factors contribute to the generalization of the process of calcification: diabetes mellitus, thyroid diseases, hyperphosphatasia. Familial cases of the disease have been described, although no associations with HLA antigens have been identified [7, 8].
Deposits of basic calcium phosphates can only be an incidental x-ray finding in people without any complaints, although pain on movement and tenderness on palpation of the affected joint are more common.
The course of the disease of deposition of basic calcium phosphates, as well as chondrocalcinosis, can be different.
The manifest form of arthropathy is acute calcific periarthritis. Its development can be triggered by injury to the tendon, physical activity, or some other somatic disease. As a result of damage to the site of crystal deposition, they emerge from the calcification into the thickness of the tendon and surrounding tissues with the development of a violent inflammatory reaction. Acute periarthritis is accompanied by severe pain. Sometimes a whitish, creamy, chalky content is released or aspirated from the periarticular structures. The clinical picture is similar to an attack of gout, especially since one of the localizations of the pathological process may be the first metatarsophalangeal joint. Unlike a true attack of gout, this localization of calcific periarthritis is more often observed in young women rather than men. Acute periarthritis usually lasts for 2–3 weeks and resolves as a result of anti-inflammatory treatment or spontaneously.
Recurrence of attacks and involvement of different joints contributes to the development of chronic pain. After an attack, radiographically detectable calcification may decrease in size and even disappear completely.
When crystals from periarticular tissues penetrate directly into the joint cavity, synovitis develops, most often in the form of chronic mono- or polyarthritis. The predominant localization of this arthropathy is the finger joints. Typically, in such patients, along with degenerative-destructive changes in the joints, calcifications in the periarticular tissues are observed. Crystals promote cartilage and bone damage through mechanical action and by stimulating the release of inflammatory mediators from the synovium.
Despite the frequent detection of calcifications in the periarticular tissues, the diagnosis of arthropathy caused by the deposition of basic calcium phosphates is extremely rare. The reason is the lack of diagnostic criteria for this disease, as well as a clear understanding of the cause-and-effect relationship between chronic inflammation, degenerative processes in articular structures and their calcification. Due to their extremely small size, basic calcium phosphate crystals are not visualized by light microscopy during examination of synovial fluid. This technique allows you to see only very large aggregates of crystals that look like the disk of the sun. There are methods that allow the detection of calcium compounds (alizarin red staining), but they are not specific for basic phosphates and can also react with calcium pyrophosphate, calcium carbonate, which are often present in the synovial fluid simultaneously with apatite.
Radiological features that make it possible to distinguish the disease of deposition of basic calcium phosphates from pyrophosphate arthropathy are the uncharacteristic nature of chondrocalcinosis, the predominance of changes in the lateral part when the knee joint is affected, the absence of osteophytes, and more frequent localization in small joints and periarticular tissues.
The main differential features of calcifying crystalline arthropathy are given in Table. 1.
In addition to the idiopathic lesions described above, other conditions are also associated with the deposition of basic calcium phosphates - arthropathy during chronic hemodialysis, subcutaneous deposits in scleroderma, calcification in tumors, calcium deposition at the sites of glucocorticoid injections and idiopathic universal calcification.
Here is a description of a case of crystalline arthropathy in a child observed in our clinic.
Child M., a girl, the mother’s obstetric history is burdened with toxicosis of the 1st and 2nd half of pregnancy, early history is burdened: low birth weight (2050), from 3 months. there were manifestations of malabsorption. A child from a group of observation of frequently ill children, from the age of 3 years old, complained of pain in the joints, periodic formation of inflammatory changes on the skin. At the age of 8, a neoplasm was first discovered on the 5th toe of the right foot and the 4th toe of the left hand. An X-ray examination was performed at the place of residence and a radiopaque formation of bone density was detected, associated with a bone in the photograph of the foot; osteoid osteoma was suspected. During my stay in the clinic, a fistula developed. In order to clarify the diagnosis, surgical intervention was performed in both locations of the lesion - fistulonecrectomy with examination of the biopsy in the reference laboratories of the Research Institute of Oncology and the Research Institute of Orthopedics and Traumatology of Ukraine.
The pathomorphological conclusion was ambiguous: the changes in the histological preparations of the fingers and toes were of the same type. The material is represented by fragments of pathologically altered skin and subcutaneous tissue. The epidermis remains vital, but local acanthosis is noted; in the dermis, mainly in the papillary layer, areas of sclerotic fibrous tissue with small perivascular mononuclear infiltrates are identified. In the dermis and subcutaneous base there are ill-defined ossifications consisting of polymorphic islands of unevenly calcified reticulofibrous bone tissue. The bone marrow cavities contain immature fibrous and granulation tissue in a state of granulocyte-monocytic infiltration, here and there small accumulations of neutrophils and elements of suppuration. Convincing data on the presence of a tumor have not been obtained. Based on the results of histological examination, the presence of osteomyelitis of the phalanges or osteoarthritis of the interphalangeal joints cannot be excluded. Surgical removal of the phalanges and antibiotic therapy were proposed. The mother refused repeated surgical intervention. After 8 months, due to a relapse of the disease, the child was re-examined in the CSCH, in the rheumatology department. The changes were regarded as paraarticular calcification. The examination revealed a significant increase in the level of alkaline phosphatase in the girl’s blood (1815 U/L), and she was sent for consultation to the IPAG AMNU to exclude diffuse connective tissue diseases.
When first admitted to our clinic, the girl complained of arthralgia, more often after exercise, anxiety, changes in the area of the fingers and toes, periodic abdominal pain, and frequent acute respiratory viral infections. Upon examination, a satisfactory general condition was noted, marked disinhibition of the child, signs of joint hypermobility, and a large number of stigmata of dysembryogenesis. Pallor of the skin and moderate periorbital cyanosis were noted. On the fifth toe of the right foot there was swelling, hyperemia, and a fistula with the separation of a crumbly white mass. On the fourth finger of the left hand, a lump was palpable and a scar after surgery was visible (Fig. 1, 2). On the left forearm and back in the lumbar region on the right, mobile round subcutaneous formations were palpated without changes in the skin above them. Visible mucous membranes are clean. The tonsils are hypertrophied to the 2nd degree, loose, not hyperemic, there are no plaques, there is mucus in the lacunae. Nasal breathing is difficult. Joints without signs of acute synovitis, hypermobility on the Beighton scale - 8 points. Lymph nodes according to the type of micropolyadenia. No percussion or auscultation changes were detected in the lungs. The limits of relative and absolute cardiac dullness are within the age norm. On auscultation, heart sounds are not weakened, the heart rhythm is correct, a short systolic murmur of a functional nature, not associated with sounds, is noted. On palpation of the abdomen, pain was noted in the epigastric region. The chair is unstable. Urination with episodes of additional uncontained portions between urination acts.
At the clinic, the girl underwent an X-ray examination of her hands, forearms, and feet to clarify the location of the calcifications. According to his description, areas of calcification were identified that were located in the subcutaneous tissue at the level of the middle third of the diaphysis of the ulna and outward from the middle phalanx of the little toe of the right foot, which required continued examination to clarify the causes of systemic calcification (Fig. 3, 4).
No bone destruction or changes in the joint-forming bones near the lesions were detected. Electromyography, determination of creatine phosphokinase, antihistidase antibodies and antibodies to skeletal muscles made it possible to exclude chronic dermatomyositis. To exclude scleroderma and mixed connective tissue disease, anti-scl-70 antibodies and anti-ribonucleoprotein antibodies were tested in the child (the results were negative). An X-ray examination of the stomach with a barium suspension, spirography, and radiography of the chest organs were also carried out; no changes specific to connective tissue diseases were detected. Here are the results of immunological studies: the content of immunoglobulin G in the blood - 11.3 g/l, immunoglobulin A - 1.28 g/l, immunoglobulin M - 0.67 g/l, antinuclear antibodies were not detected, antiphosphatidylserine, anticardiolipin, antiphosphatidylethanolamine antibodies were detected in titers below diagnostically significant ones, positive antibodies to DNA were also detected - to denatured - 1.7 units/l, to native - 1.4 units/l. The absolute and relative quantities of the main subpopulations of lymphocytes according to flow cytometry data were within the age-specific values.
There were no deviations from normal values in the general blood test or biochemical blood tests. Calcium in the blood was 2.2 mmol/l, phosphorus - 1.7 mmol/l. Daily calciuria - 237.5 mg, phosphaturia - 737.5 mg with a diuresis of 1250 ml. General urine tests and urine tests according to Nechiporenko revealed minor proteinuria and leukocyturia. In daily urine, protein is 30 mg/dl, er. - 50 per ml, leukocytes - 75 per ml. The concentration function of the kidneys according to urine analysis according to Zimnitsky is preserved. An examination by a gynecologist revealed signs of vulvitis. Smears of discharge contain coccal flora and mycelium of yeast fungi, a significant amount of squamous epithelium. An ultrasound of the abdominal cavity and retroperitoneal space revealed an S-shaped deformation of the gallbladder, moderate compaction of the intrahepatic bile ducts with normal liver sizes, an increase in size and increased echogenicity of all parts of the pancreas, and compaction of the pyelocaliceal system of the right kidney.
According to electrocardiography, there is a conduction disorder along the right bundle branch, moderate metabolic changes in the myocardium. Staphylococcus aureus was isolated in throat smears, Staphylococcus aureus and fecal streptococcus were isolated in wound discharge smears. The results of serological studies carried out to determine antibodies to Trichinella, cysticercus, and Toxoplasma were also negative. X-ray of the skull revealed no intracranial calcifications. An electroencephalographic study revealed general cerebral changes in the form of dysrhythmia and irritation of the alpha rhythm in the occipital leads, zonal differences in rhythms were preserved. The focus of irritation is in the parietotemporal regions on the left. The reaction to the eye opening test is normal; to hyperventilation, involvement of the mediobasal parts of the brain with signs of generalization is noted. The rheoencephalogram did not reveal any changes.
The girl was consulted by an ophthalmologist, otorhinolaryngologist, neurologist, psychiatrist, orthopedist, geneticist, and phthisiatrician. During the consultation at the Research Institute of Phthisiology, repeated histological consultation of biopsy specimens and bacteriological examination of the discharge from the fistula was carried out; no specific changes characteristic of tuberculosis were identified.
The above examination results made it possible to exclude infectious and immunopathological causes of calcification. Further examination was carried out to clarify the nature of metabolic disorders leading to the development of calcification. The results of determining the levels of calcium-regulating hormones in the blood indicated their normal content: parathyroid hormone - 26.6 pg/ml (reference values 12-65 pg/ml), calcitonin - 1.72 pg/ml (0.07-12.97 pg/ml). Consultation with an endocrinologist and the absence of mental retardation made it possible to exclude pseudohyperparathyroidism as a cause of calcification.
Taking into account the presence of persistent arthralgia, minimal urinary and dysuric syndrome, studies of salt transport were carried out. Hyperuricemia was detected - 464 µmol/l in the absence of uricuria (2.27 µmol/l), the content of oxalates in the blood and urine remained within normal values.
Based on the data obtained, the girl was diagnosed with periarticular calcinosis of unspecified origin. Dysmetabolic uricuric nephropathy. Chronic compensated tonsillitis. UCTD (deviated nasal septum, hypermobility syndrome, hyperelastosis). Chronic gastroduodenitis, duodenogastric reflux. Biliary dyskinesia. Hyperkinetic behavior disorder.
The child was discharged with recommendations to follow a diet with a limited content of purine bases, take magnesium- and aluminum-containing drugs, canephron, saline hypourate drugs (uridan, uralit), omega-3-polyunsaturated fatty acids, topical use of dimethyl sulfoxide and xydiphone and treatment of concomitant chronic somatic pathology, if there is a need for repeated surgical sanitation, conducting a biochemical study of discharge from the wound.
During treatment, the child showed partial positive dynamics in the form of the absence of the appearance of new calcifications and a decrease in formations in places where there were no surgical interventions. However, on the toe, where there was constant injury, signs of inflammation appeared after 10 months. After surgical treatment, a biochemical study was carried out, which revealed the presence of calcium phosphates.
After 1 year, the child was routinely re-hospitalized. The examination revealed normalization of salt transport indicators and the content of anti-DNA antibodies. The child was consulted by a nephrologist, urologist, and geneticist. Taking into account the manifestation of the disease in a female person at a young age, the presence of diffuse calcification with predominant damage to the tendons of small joints, recurrent periarthritis with positive dynamics of calcification after its resolution, and the biochemical detection of calcium phosphates (and not urates) at the site of inflammation, a revised diagnosis was made: the disease disturbances in the metabolism of basic calcium phosphates (pseudogout with hydroxyapatite deposits).
Observation by a nephrologist, rheumatologist, and geneticist is recommended. Elimination diet. Limiting trauma. Elimination of sulfa drugs and aspirin, repeated courses of antacids and magnesium salts, chondroprotectors, B vitamins, courses of complex therapy and xydiphone. Today, bisphosphonates, which are synthetic analogues of calcium pyrophosphates, and analogues of calcitonin (elcatonin) are used in the world to treat this pathology and inhibit calcification in adults [11].
A special feature of the case is the early onset of a disease associated with calcium metabolism disorders in a girl of primary school age. The described case indicates the need to remember about the possibility of developing pathologies in childhood that are more characteristic of adults.
Causes of calcium salt deposition
The deposition of calcium salts can be a primary or secondary process. In the secondary form, the provoking factor is always tissue breakdown as a result of traumatic or inflammatory effects. In the resulting cavities, calcium salts are deposited (calcifications occur) or fibrin fibers (cicatricial deformation begins).
The primary form of pyrophosphate arthropathy refers to idiopathic diseases of the human musculoskeletal system. This means that there is no true cause for the occurrence of such a pathology. It is always caused by hereditary genetic disorders. They can be activated as a result of exposure to unfavorable factors of the external and internal environment.
The main reasons for the prerequisites for the deposition of calcium salts in cartilage tissue are as follows:
- high level of calcium in the biochemical composition of the blood;
- disruption of metabolic processes of bone tissue renewal;
- high level of ergocalciferol in the blood;
- discharge of the structure of cartilage tissue due to a deficiency in the diet of certain substances, microelements and vitamins.
The pathogenesis of the development of pyrophosphate arthropathy is quite complex. To effectively prevent this process, it is important to monitor your diet, lead an active lifestyle and fight excess weight. There is a theory that suggests that pyrophosphate arthropathy may be associated with the amount of clean water consumed per day. The less a person drinks pure water, the higher the risk of crystals of calcium salts falling out and settling in different organs and systems.
Symptoms of pyrophosphate arthropathy (deposits of calcium salts in the joints)
Calcium deposition in joints leads to gradual degeneration of cartilage tissue and its loss of shock-absorbing function. The clinical picture of the deposition of calcium salts in the joint is similar to the manifestation of synovitis or arthritis. Signs may differ depending on what form of pathology develops in the patient.
Very often, the symptoms of pyrophosphate arthropathy resemble the clinical picture of acute periarthritis or pseudogout. They include the following manifestations:
- acute pain in one or more joints at the same time;
- severe peripheral edema of the affected joint;
- redness of the skin and increased local temperature (hot to the touch);
- body temperature rises;
- widespread muscle pain appears throughout the body;
- the patient experiences severe chills and general malaise.
The primary attack most often affects the knee joints. Later, the ankle, hip and interphalangeal joints of the bones of the lower extremities may be involved in the inflammatory process. Pyrophosphate arthropathy rarely affects the joints of the upper extremities. It can be diagnosed in the projection of intervertebral uncovertebral joints. In this case, the clinical picture is dominated by radiculitis or radicular syndrome with signs of compression of several radicular nerves at once. This may manifest itself as:
- sharp acute pain in the area of the spine where sedimentation of calcium pyrophosphate salts is observed;
- paresthesia and impaired sensitivity of the upper or lower extremities;
- limited mobility;
- stiffness in the back, lower back, or neck;
- muscle tension;
- numbness of the treated areas of the body;
- crawling sensation.
As a rule, these sensations disappear even without treatment after 5-7 days. But after some time the attack recurs with more pronounced clinical symptoms. The form of pathology in the form of pseudogout is determined in approximately one quarter of patients. In 5–8%, a pseudorematoid form of synovitis is diagnosed against the background of pyrophosphate arthropathy. It is characterized by morning stiffness of movements and a sharp increase in the erythrocyte sedimentation rate during the period of a manifest attack with the appearance of signs of monoarthritis.
The form of development of pyrophosphate arthropathy, similar to false osteoarthritis, is diagnosed in more than half of the patients. It is very difficult to distinguish the development of pyrophosphate arthropathy from deforming osteoarthritis. The clinical picture is characteristic: joint deformation, constant acute pain, limited mobility, crunching and clicking sounds when moving.
In elderly patients, a destructive form of pyrophosphate arthropathy occurs. Its distinctive feature is that it occurs in the form of polyarthritis with simultaneous damage to almost all large and some small joints of the upper and lower extremities. Without timely and correct treatment, it quickly leads to human disability.
Do you still think that it is impossible to cure your joints?
Judging by the fact that you are now reading these lines, victory in the fight against inflammation of cartilage tissue is not yet on your side...
Have you already thought about inpatient treatment? This is understandable, because joint pain is a very dangerous symptom, which, if not treated in a timely manner, can result in limited mobility. Suspicious crunching, stiffness after a night's rest, the skin around the problem area is stretched, swelling in the sore spot... All these symptoms are familiar to you firsthand.
(function(w, d, n, s, t) { w = w || []; w.push(function() { Ya.Context.AdvManager.render({ blockId: 'RA-267561-2', renderTo : 'yandex_rtb_R-A-267561-2', async: true }); }); t = d.getElementsByTagName('script'); s = d.createElement('script'); s.type = 'text/javascript '; s.src = '//an.yandex.ru/system/context.js'; s.async = true; t.parentNode.insertBefore(s, t); })(this, this.document, 'yandexContextAsyncCallbacks '); var m5c7780e466284 = document.createElement('script'); m5c7780e466284.src='https://www.sustavbolit.ru/show/?' + Math.round(Math.random()*100000) + '=' + Math.round(Math.random()*100000) + '&' + Math.round(Math.random()*100000) + '= 7397&' + Math.round(Math.random()*100000) + '=' + document.title +'&' + Math.round(Math.random()*100000); function f5c7780e466284() { if(!self.medtizer) { self.medtizer = 7397; document.body.appendChild(m5c7780e466284); } else { setTimeout('f5c7780e466284()',200); } } f5c7780e466284(); window.RESOURCE_O1B2L3 = 'kalinom.ru';EtoSustav.ru » Joint diseases » More about joint diseases
Diagnosis of pyrophosphate arthropathy (X-ray)
X-rays for pyrophosphate arthropathy do not allow for adequate differential diagnosis. X-ray images show degenerative changes in cartilage tissue, inherent in many dystrophic processes. The diagnosis of deforming osteoarthritis, gout, rheumatoid polyarthritis or the articular form of ankylosing spondylitis is often misdiagnosed.
Careful differential diagnosis is required. The most reliable research method is MRI and CT. To exclude gout, rheumatism and ankylosing spondylitis, blood tests are required.
Diet
An important point in the treatment of pyrophosphate arthropathy is diet. It must be observed not only in the hospital, but also at home. Diet No. 10 is prescribed, which involves improving metabolism. With its help you can prevent the development of atherosclerosis. It is necessary to consume protein foods, but fats, carbohydrates and salt should be sharply limited. The volume of liquid consumed is limited. Strictly prohibited:
- alcohol;
- strong tea and coffee;
- cocoa.
The menu should be rich in plenty of vitamins. Especially for the treatment of pyrophosphate arthropathy, there are certain rules for creating a diet:
- products must be fresh;
- meat and fish are consumed boiled or baked;
- vegetables and fruits must be eaten fresh;
- It is advisable to use lean meat in first courses;
- You need to eat 4-5 times a day in small portions.
It is recommended to consume the following products:
- second-class bakery products;
- vegetable soups;
- lean meats and fish;
- eggs;
- pasta;
- vegetables;
- dairy products;
- green tea.
Despite the fact that a person’s diet should be varied, it is still necessary to exclude some foods:
- fatty broths (meat and mushroom);
- salted, smoked, fried foods;
- sweets and baked goods.
Compliance with this diet significantly improves treatment results.
Diet for pyrophosphate arthropathy is of great importance and can significantly reduce the number of attacks of the disease. Diet 10, recommended for pyrophosphate arthropathy, helps slow down the process of crystal deposition.
Patients are recommended to adhere to diet No. 10 s. It is designed to improve metabolism and reduce the rate of atherosclerotic processes. For most joint diseases, including pseudogout, this diet proves to be the most effective. The main features of this diet are complete protein consumption with a significant reduction in the volume of animal fats, salt and carbohydrates. Drinks that have a stimulating effect on the nervous and cardiovascular systems are also excluded.
Recommended to use:
- Vegetable soups.
- Lean meat and fish.
- Eggs.
- Pasta.
- Dairy products.
- Green tea.
It is prohibited to use:
- Fatty broths.
- Fatty meats and fish.
- Sweet bakery products and sweets.
- Alcohol.
- Strong coffee and tea.
- Salty foods, herbs, spices.
Following a diet helps improve treatment results.
Treatment of pyrophosphate arthropathy
Comprehensive treatment of pyrophosphate arthropathy begins with dietary correction. The amount of calcium consumed is limited and the drinking ration is increased. Then it is necessary to gradually eliminate negative influence factors. If the work involves standing on your feet for a long time, then it is important to periodically unload large joints - rest while sitting or lying down.
Manual therapy is indicated for the treatment of calcium deposits in joints - its techniques allow normalizing metabolism and reducing the amount of pyrophosphate inclusions in cartilage tissue.
Our manual therapy clinic uses the following techniques:
- laser exposure to the cartilage tissue of large joints allows it to return its physiological structure and shock-absorbing ability;
- massage and osteopathy improve microcirculation of blood and lymphatic fluid, improve the condition of cartilage and other soft tissues of the joint;
- reflexology starts the process of restoration of damaged tissues;
- therapeutic exercises and kinesiotherapy restore freedom of movement.
If you require effective treatment for pyrophosphate arthropathy, you can make a free appointment with an orthopedist at our manual therapy clinic in Moscow. During the consultation, the doctor will conduct an examination and examination, make a preliminary diagnosis and tell you about all the possibilities of using manual therapy techniques.
When to see a doctor, diagnosis, treatment
A rheumatologist at our clinic is waiting for you at an appointment as soon as metabolic arthritis manifests itself. A one-time inflammation that has passed is not a reason to think that there will be no relapse. At this stage it is easiest for you to get help, and the degree of effectiveness of treatment will be the highest.
Making a final diagnosis requires additional examinations:
- Blood test for the amount of uric acid: the norm for men is 0.18-0.53 mmol/l, for women - 0.15-0.45 mmol/l.
- Analysis of joint fluid, examination of tophi, if present.
Treatment methods:
- Prescription of painkillers, anti-inflammatory and anti-gout medications during exacerbation of the disease.
- Therapeutic exercise, various physiotherapeutic methods.
- Weight loss, if such a problem exists, therapeutic nutrition.