Radicular syndrome is a complex pathology, the etymology of which can be different. Destructive changes in the vertebral discs occur in stages, so they are most often diagnosed when pain occurs.
Causes of radicular syndrome:
- pathological changes in the spine due to osteochondrosis;
- defect of the posterior wall of the spinal column cavity in the form of a hernia;
- hypoactivity due to sedentary work and refusal to exercise;
- significant deformation of the spine due to spondyloarthrosis;
- tumors, injuries and scars in the area of the base of the axial skeleton;
- serious consequences of osteoporosis in the form of vertebral fractures;
- the course of infectious diseases: tuberculosis, osteomyelitis;
- excessive force on the spine for a long time;
- frequently repeated hypothermia of the body (working in the cold);
- genetic predisposition to the disease;
- feature of human age-related changes.
Location of pathology:
1. Cervical region. The main symptom of damage to this area is neck pain, felt in the subscapular region and shoulders. The patient regularly feels tingling in his hands, and he regularly has a desire to stretch his neck muscles. The patient's skin becomes pale and hair thins. It is easy to identify the problem yourself, because it is enough to raise your hand high from the side of the affected area. If the cervical spine is affected, then such manipulation will be difficult or impossible.
2. Thoracic region. When palpating this part of the body, the main lesions are easily identified. A common mistake people make is that they confuse the disease with intercostal neuralgia and begin to self-medicate. Symptoms of damage to the thoracic region are also similar to cardiac colic, so they try to eliminate them without consulting a doctor with Corvalol.
3. Lumbar region. The vulnerability of this zone is obvious. Radicular syndrome of the lumbar spine is characterized by exhausting pain and frequent complications of the pathology. As nerve compression progresses, it becomes difficult for a person to move without assistance.
Diagnosis of the disease:
1. X-ray. It is produced in a two-plane projection: oblique and straight.
2. MRI. If it is impossible to make a diagnosis of a spinal lesion, magnetic resonance imaging is used.
Disease prevention:
- a change in professional activity that involves regular stress on the spine;
- regular exercise without excessive strength exercises;
- visiting the swimming pool and massage sessions;
- eliminating signs of obesity with the help of exercise therapy and special diets;
- wearing clothes according to the season and weather conditions;
- choosing the right shoes and avoiding bulky models.
How do physiotherapy treatments work?
Electrophoresis. The method involves placing electrodes connected to a special device on the body. The supplied current, affecting the nerves and joints, acts along a fading trajectory without painful sensations for the patient.
Reflexology. Treatment with special needles is usually carried out by a chiropractor. The puncture sites are determined after identifying problem areas in the spine.
Ultrasound. It is especially effective in eliminating pain in the sacrolumbar area. The intensity of the waves is determined by a specialist. The patient may feel slight vibration. Contraindications for the procedure include malignant tumors, pregnancy and serious blood diseases.
Magnetotherapy. It is prescribed for swelling of areas of pinched nerves, inflammation and pain symptoms. A magnetic field created by special equipment affects problem points for 10-20 minutes. Features of the procedure include the possibility of carrying it out in clothing and a plaster cast.
Treatment with mud. Healing baths are necessary to calm the nervous system, which has suffered from periodic attacks of pain in the spine or neck.
Radon baths. Active treatment with their use eliminates inflammatory processes and solves neurological problems.
Massage. It is necessary to strengthen the spinal muscles and eliminate signs of poor circulation in the tissues.
Causes
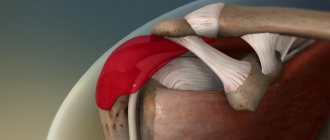
The most common cause of cervical CS is osteochondrosis. Against the background of a decrease in the height of the intervertebral discs, the diameter of the intervertebral foramina decreases, which predisposes to pinching of the spinal roots. Another compression factor is intervertebral hernia. This is one of the complications of osteochondrosis, causing severe health consequences, for example, discogenic myelopathy. This syndrome also develops with spondylosis as a result of pinching of nerve endings by osteophytes or deformed structures of the facet joints. The prerequisites for the CS are:
- spinal cord injuries, severe bruises, vertebral subluxations;
- congenital and acquired spinal abnormalities, including kyphosis and scoliosis;
- osteomyelitis;
- benign and malignant neoplasms;
- hormonal imbalances.
Factors that provoke cervical CS include a sedentary lifestyle, excessive physical activity, and obesity. Inflammation of the spinal roots often occurs against the background of syphilis, tuberculosis, and spinal meningitis.
Physical therapy for nerve compression
It is better to prevent acute radicular syndrome than to eliminate its consequences. During the recovery period after a relapse, it is useful to perform the following exercises:
1. Lying down. Once on the mat, straighten your legs and place your arms along your body. The exercise consists of tensing and relaxing the abs at least 15 times. Next, the bent knees need to spring in the opposite direction from the upper body for a couple of minutes.
2. On all fours. After taking this position, you should, with leisurely movements, play like a cat, which arches and lowers its back. The exercise is performed until pleasant exhaustion occurs.
3. Roll on the ball. The item must not contain a traumatic surface. Having placed it behind your back, you should make smooth rolls on the ball back and forth on the floor.
4. Exercise with a hoop. The times of halahup have not yet come after the relapse. It is better to choose a light object with a flat surface. Spin the hoop for a couple of minutes.
5. Hanging on the horizontal bar. Ten minutes of this exercise twice a day is enough to strengthen the spine and obtain a positive result in case of frequent pain in its area.
Symptoms of the disease
Radicular syndromes differ in the combination of symptoms, the appearance of which is provoked by irritation of a specific spinal root. The severity of clinical manifestations is influenced by interradicular connections, individual characteristics of the localization of nerve endings, the degree of their compression, and the shape and thickness of the roots.
Constant headaches
Headaches usually occur with concomitant CS syndrome, vertebral artery compression syndrome and oxygen starvation of the brain. They can be reflected, that is, irradiate from connective tissue structures damaged by osteophytes. Headaches often resemble migraines, but unlike them, they disappear for a short time. Discomfortable sensations are initially localized in the back of the head, and then spread to the temples and forehead.
Headaches and dizziness are common signs of osteochondrosis.
Chin muscle atrophy
On the side of the affected root, muscle-tonic changes are more pronounced. This sometimes causes torticollis. But the muscles of the chin also undergo destructive changes, especially when there is compression or inflammation of the spinal roots located in the area of the C4 vertebrae, less often - C5. At the initial stage of CS, hypertonicity of the skeletal muscles is observed. Contractile functions gradually disappear, and a double chin forms against the background of muscle fatigue.
Numbness of skin, tongue
Cervical radicular syndrome is characterized by the appearance of paresthesia - a sensitivity disorder. Sensations of numbness and burning of the skin of the face and tongue occur spontaneously. Paresthesia is caused by irritation of the superficial nerve and can disappear with a change in body position. The only way to get rid of discomfort is by treating the underlying pathology - cervical osteochondrosis.
Burning tongue with cervical osteochondrosis.
Upper limb dysfunction
When the spinal root is severely pinched, a burning pain occurs, radiating to the forearm and then to the arms. To reduce its severity, a person deliberately limits movements. Feelings of “crawling goosebumps”, numbness, and tingling appear in the hands. Over time, the arm muscles weaken and motor functions become impaired.
Swelling
If connective tissue structures are injured by an osteophyte or hernial protrusion, inflammatory edema quickly forms. They provoke even greater infringement of the spinal roots and an increase in the severity of pain. Such swelling is not visualized, unlike those that form when large blood vessels located close to the surface of the skin are damaged.
Cardiac and pulmonary disorders, impaired swallowing reflex
Such neurological disorders usually occur with thoracic CS and are quite rarely observed with compression of nerves localized near the cervical vertebrae. The reason for the decrease in the functional activity of the cardiovascular and respiratory systems is a violation of innervation. Clinically, this is manifested by spontaneous shallow breathing and various arrhythmias. A violation of the swallowing reflex is often accompanied by an unproductive cough and a sore throat.
Mental disorders
Constantly expecting pain has a negative impact on a person’s psycho-emotional state. He becomes suspicious, irritable, apathetic, and feels exhausted in the morning due to developing insomnia.
In severe cases, doctors diagnose patients with neuroses and depression. Therefore, they often include sedatives, tranquilizers, and antidepressants in the therapeutic regimens of patients with cervical CS.
Pain
At the initial stage of development of the pathology, mild discomfort occurs. As destructive changes in the discs and vertebrae worsen, their severity increases significantly. Any awkward or sudden movement of the head (tilt, turn) leads to burning, sharp, piercing pain. Patients describe it to doctors as an “electric shock.” It spreads to the back, upper chest, shoulders, and is sometimes felt even in the fingers.
To reduce the intensity of pain, muscle spasm occurs. By limiting movement, the body tries to get rid of uncomfortable sensations. But usually tension in the skeletal muscles leads to increased compression of the spinal roots and increased severity of pain.
Manual therapy
With a mild effect on the muscles, radicular spine syndrome is treated as follows:
1. Warm up the muscles. To carry it out, they are initially relaxed, while acting on the trigger points of the back. The fascia is then released through myofascial release.
2. Treatment of the spinal column. It can be treated in this way using soft techniques (MMT), which are fundamentally different from classical methods. With the new approach, radicular nerve syndrome is blocked not by stretching the ligaments, but by bringing them closer together. In the same way, the effect on the muscle corset is carried out.
3. Impact on joints. Soft therapy techniques are also used to relieve pain. MMT according to the Mulligan system is carried out using a special belt. The advantages of the technique are the safe removal of load from problem areas during joint mobilization.
Symptoms and signs of nerve root compression
Clinical symptoms of root compression depend on the degree of development of the underlying disease and the severity of the compression process. Minimal signs of nerve root compression include pain, lack of sensation, paresthesia, and impaired reflexes.
In the absence of timely treatment, signs of nerve root compression gradually increase. At the peak of compression, a feeling of complete numbness and dysfunction of the part of the body for which the damaged nerve fiber is responsible may occur.
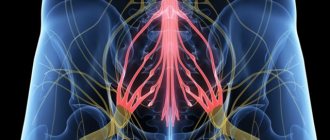
The pain with radiculopathy is acute. It can be burning, piercing, shooting. A distinctive feature is the tendency to quickly spread along the nerve fiber. Thus, when the roots in the lumbosacral spine are affected, the pain quickly affects the area of the buttock, thigh and lower leg. Gradually the unpleasant sensations reach the toes.
The next characteristic symptom is poor posture. The muscular frame of the back strives to compensate for the insufficiency (prolapse or protrusion) of the intervertebral disc by increasing tone. Therefore, excess tension occurs on one side and relaxation on the other. Poor posture can be persistent and develop into curvature of the spinal column.
Then secondary ischemic tissue degeneration begins. Dysfunctions of the internal organs of the chest, abdominal cavity, and small pelvis may occur. Patients suffering from chronic radiculopathy often experience colitis, enteritis, pancreatitis, biliary dyskinesia, overactive bladder syndrome, infertility and erectile dysfunction (in men).
Purpose of the bandage
A special corset is prescribed if necessary to reduce the load on the lumbar column. There are three types of therapeutic bandages:
1. Orthopedic. After surgery for radicular syndrome, you cannot do without such a supporting corset. If there are serious problems with the cardiovascular system, the use of an orthopedic design may be prohibited.
2. Radiculitis. When worn, the vertebrae will return to their correct positions. During the restoration of impaired blood circulation, muscle spasms will be eliminated.
3. Shants collar. This type of orthopedic neck brace does not cause allergies and is prescribed for neurological disorders. There is a choice between an inflatable version of the corset, a rigid design and a soft model.
Radicular osteochondrosis: preventive measures
It is almost impossible to completely cure osteochondrosis that has already developed. With adequate therapy, it is possible to achieve long-term remission, which can last for years or even decades. However, to avoid exacerbation of osteochondrosis, it is necessary to reconsider your lifestyle and strictly follow the doctor’s recommendations.
Measures to prevent osteochondrosis are:
- a rational balanced diet, including all the necessary microelements and vitamins for the normal functioning of the body;
- rejection of bad habits;
- dosed physical activity (therapeutic exercises, swimming, walks in the fresh air);
- reducing the load on the spine;
- if you have a sedentary job, take breaks every hour and change your position (you can do a simple set of exercise therapy exercises);
- normalization of body weight;
- use comfortable shoes (it is recommended to avoid high-heeled shoes).
Diet for illness
Compression of the nerve roots often occurs in those who like to eat quickly. It will not do any harm if we are talking about a light salad. The list of prohibited foods for the above-mentioned pathology includes fatty-based dishes flavored with seasonings and salt. The exceptions are bay leaves, dill and coriander.
Radicular syndrome symptoms will weaken if you fast for a couple of days at the peak of the disease. After the stated period of food abstinence, you can without fanaticism include berries, fruits and vegetable juices in your diet. When the manifestation of the disease significantly weakens, you should diversify the menu with fish, lean meat, and soups without legumes. With complete remission, you can eat everything except salty foods, which can cause swelling. As for drinks, it is recommended to opt for dried fruit compotes.
Diagnostic methods
The primary diagnosis is made based on the results of a series of functional tests that are performed to assess sensation and limitation of movement. Upon palpation, trigger points located near the spinous processes and tonic-muscular changes in the area of the affected spinal segment are determined. Damage to a particular root is indicated by the localization of pain and areas of reduced sensitivity. The location of the radicular syndrome is also revealed by conducting electroneuromyography, which determines the general functional state of the peripheral nervous system and muscles.
The main task of diagnosis is to detect the cause of cervical CS. For this purpose, instrumental studies are carried out:
- Spinal radiography is prescribed to assess the condition of vertebral structures, detect osteochondrosis, spondyloarthrosis, spondylolisthesis, congenital and acquired anomalies of the cervical spine;
X-ray of the cervical spine.
- MRI and CT are the most informative in identifying intervertebral hernias, hematomas, hemorrhages in the spinal cord, meningoradiculitis, benign and malignant neoplasms.
MRI of the cervical spine.
If infectious inflammation of the spinal roots is suspected, laboratory tests are performed. They make it possible to identify the species of pathogenic microorganisms or viruses and their sensitivity to pharmacological drugs.
Consultation with a specialist
During a patient’s visit, the doctor carries out the following work:
1. Conversation. By asking leading questions, the specialist finds out the history of the disease. Next, he clarifies the patient’s general condition and conducts a dialogue about current health problems.
2. Study of photographs. If the patient brought them with him, the doctor analyzes the information provided. Then, based on the data obtained, the patient’s individual card is filled out.
3. Palpation. It includes a careful examination of the affected areas of the spine. After a visual examination, the patient is offered to undergo muscle testing.
4. Selection of treatment option. All its principles are spoken out loud, and the patient’s questions are answered.
When to see a doctor
The pain that occurs when the cervical spinal nerves are damaged is so severe that immediate medical attention is necessary to relieve it. But neurologists and vertebrologists recommend contacting them at the first signs of the development of osteochondrosis. This is discomfort in the neck after physical activity, when the weather changes, or after intense sports training. If treatment is carried out at this stage, it will be possible to avoid severe, sometimes irreversible complications of osteochondrosis.