- Causes of jaw inflammation
- What to do if the lower jaw is inflamed
- Diagnosis and treatment of jaw inflammation at the dentist
- Features of treatment for older patients
Inflammatory diseases are very common and are presented in all their diversity, from clinical manifestations to localization. Differential diagnosis is not always easy, especially if there are no specific signs. Often a dentist finds himself in this situation when a patient comes to him with inflammation under the jaw on the neck. In this case, it is very important to make a correct diagnosis and prescribe effective treatment.
Causes and symptoms of periostitis
Symptoms of periostitis include swelling of the gums and face, suppuration, fever, and severe pain. The severity of dental flux manifestations depends on the form and severity of the disease. Swelling and asymmetry of facial contours depend on the location of the inflammation. With periostitis of the upper jaw, swelling of the upper lip, cheek and infraorbital area occurs. With periostitis of the lower jaw, swelling can be observed in the lower part of the face.
The causes of flux can be:
- failure to comply with hygiene rules;
- diseased or untreated teeth;
- consequences of complex tooth extraction;
- jaw injuries;
- infectious and inflammatory processes in the body;
- weakened immunity.
Causes of jaw inflammation
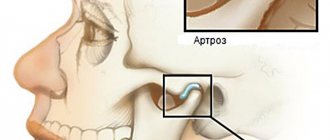
The lower jaw and the area under it have a rather complex anatomical structure. Muscles, lymphatic and blood vessels, bone structures, etc. are concentrated in this zone. Also, the temporomandibular joint or other anatomical zones may be involved in the inflammatory process, from which the lesion spreads to the neck area. Common causes of inflammation of the jaw are:
- Tooth root cyst.
- Osteitis.
- Inflammation of the lymph nodes.
- Tumors of blood vessels and soft tissues of the neck.
- Traumatic injuries.
- Inflammation of the middle ear.
- Gingivitis, periodontitis, periodontal disease, etc.
Given such a variety of causes, the approach to diagnosis and treatment must be individualized. Due to his ignorance, the patient may choose the wrong doctor and waste his time. In situations where something is inflamed under the jaw on the right or left and at the same time a tooth or temporomandibular joint hurts, you need to consult a dentist. If the pain is localized in the ear area, then you need to visit an ENT specialist.
Features of the treatment of dental periostitis
To treat tooth flux, conservative and surgical methods are used. The choice of treatment method depends on the causes and degree of neglect of the disease.
The conservative method (without surgery) is used:
- at the initial stage;
- caused by weak immunity;
- due to other inflammations in the body.
For non-surgical treatment of flux, anti-inflammatory and antibacterial drugs and physiotherapy are used. The tooth is not removed, but the gum is cut in the area of swelling and drainage is installed.
In the case of purulent inflammation associated with dental diseases (odontogenic periostitis), or when conservative treatment is ineffective, surgical intervention is used.
Causes of inflammation
Most inflammatory diseases of the maxillofacial area are associated with dental pathology. These include periostitis, osteomyelitis , lymphadenitis and others. As a rule, they arise as a result of various dental diseases or tissues surrounding the teeth. In addition, the causative agents of inflammatory infections can be staphylococci, streptococci, candida fungus and other microorganisms, including those that are present in the oral cavity of every person. Often, infection occurs due to defects in the surfaces of teeth: carious lesions. This becomes an entry point for infection. Complications are associated with the fact that tooth tissue is not able to recover naturally. Therefore, the longer you wait to go to the dentist, the higher the risk of developing inflammation.
Stages of surgical treatment of flux:
- anesthesia (usually local);
- opening the focus of suppuration (gum incision);
- removal of pus;
- drainage (installation of drainage to ensure the outflow of inflammatory fluid);
- X-ray (to determine the cause of periostitis);
- removal of a diseased tooth or drug treatment.
In addition, for acute purulent periostitis, antibiotics, physiotherapy and painkillers are usually prescribed. Treating periostitis with antibiotics at home without consulting a doctor can cause side effects and resistance of pathogenic bacteria to the drug.
Periostitis of the jaw - symptoms and treatment
Treatment of periostitis is always surgical; if you deviate from this rule, there is a serious danger of a limited focus of inflammation flowing into a more dangerous - diffuse form, which will require different treatment tactics and often hospitalization of the patient.
Treatment of periostitis is standard and consists of eliminating the source of primary inflammation and evacuation of pus, i.e., removing the causative tooth (in cases of unfavorable treatment prognosis) and surgically opening the site to its entire width, followed by drainage.
The procedure is usually performed under local anesthesia; in some cases, drug sedation is indicated; anesthesia is also possible. You need to understand that the introduction of an anesthetic into tissues strained by exudate (fluid accumulation) is an extremely painful procedure, therefore, the method of pain relief before periostotomy (opening an abscess) has its own specifics: conduction anesthesia is preferable (a type of anesthesia when the nerve is blocked to the operation site) followed by local anesthesia performed superficially with a thin needle, without immersing the needle into the abscess.
The diseased tooth must be removed in the case of an unfavorable therapeutic prognosis: the presence of large foci of bone destruction, incorrect previously carried out treatment of the canals, resulting in their perforation or blockage by a fragment of an instrument, etc. In cases of a favorable prognosis, endodontic treatment is carried out, which involves the removal of pulp decay from the canals, appropriate mechanical and medicinal treatment of the canals with a special instrument and powerful antiseptics to eliminate infection in them, followed by temporary filling with calcium preparations and temporary filling of the tooth. Subsequent X-ray monitoring is very important in order to confirm the effect of the canal therapy: the focus of destruction in the bone should decrease and subsequently disappear.
To evacuate pus, periostotomy is performed (dissection of the mucosa and periosteum) along the entire length of the infiltrate along the transitional fold.
As a rule, the surgeon detects a characteristic symptom - detachment of the periosteum from the bone, whereas in a healthy state the periosteum is firmly attached to the cortex. At this stage, the abscess is emptied, or the absence of pus is detected along with the periosteal reaction. The surgeon uses a blunt instrument to probe the entire abscess cavity to identify isolated lesions. In the case of the presence of pus, irrigation (washing) of the subperiosteal space with antiseptics is usually carried out, followed by the introduction of drainage (usually a strip of glove rubber) into the wound to prevent its edges from sticking together. The wound is not sutured; the patient is given a dressing after a day or two to remove the drainage [8].
In the absence of contraindications, antibacterial therapy (in most cases, semisynthetic penicillins) and NSAIDs (nonsteroidal anti-inflammatory drugs) are prescribed. In case of severe edema, desensitizing drugs are prescribed. It is also necessary to prescribe analgesics or their direct intramuscular administration after surgery, since in the first hours after treatment, when the effect of the anesthetic wears off, severe pain symptoms appear. It also makes sense to locally cool the infiltrated area with ice for several hours to reduce bleeding and swelling. The cooling time must be assigned based on the patient’s subjective feelings, and not on specific time periods.
Almost always, this treatment leads to a positive result: within a few hours the patient experiences relief, decreased pain and swelling. Although the infiltrate in the form of a moderately painful compaction will persist for several days.
A follow-up visit the next day is necessary to confirm the results of the treatment and possible removal of the drain if there is no discharge from the wound. Subsequently, the patient is observed by a doctor for 3-5 days; it is quite legal to issue a certificate of incapacity for work for this period. After the pronounced symptoms of inflammation disappear, they begin to continue treatment of the causative tooth.
In rare cases, for example, when the incision is of insufficient length or when the drainage falls out and the edges of the wound stick together, treatment may be complicated due to a delay in the evacuation of residual pus from the lesion. In these cases, the incision should be widened and drainage should be ensured by introducing drainage.
Treatment of various types of periostitis
Treatment of serous periostitis
Serous periostitis can occur due to jaw trauma. No special therapy is required to treat serous periostitis. At this stage, it is possible to clean the dental canal and create the opportunity for the independent release of fluid (exudate) during inflammation.
Treatment of acute purulent periostitis
In the case of acute purulent periostitis, the dentist cuts the gum, removes the pus and drains the suppuration. When draining, the tip of a rubber strip (drainage) is inserted into the cavity at the incision site. Drainage prevents the wound from healing too quickly and allows fluid to drain out. It is advisable to remove a diseased tooth, the source of infection of acute periostitis, if:
- severely damaged crown;
- obstruction of root canals;
- lost functionality;
- ineffectiveness of the non-surgical method;
- mobility.
In other cases, it is recommended to eliminate the relevant causes of infection (for example, inflammation of the tonsils and throat), as well as restore the immune system. The most effective approach to the treatment of acute purulent periostitis is complex therapy, combining surgery, drug therapy and physical therapy.
Treatment of diffuse periostitis
Diffuse periostitis is characterized by widespread infection, not limited to a local focus. This is a severe type of disease. As a rule, the patient needs the help of maxillofacial surgeons. In stationary conditions, an operation is performed to remove part of the periosteum or bone. Treatment of diffuse periostitis is complemented by drug therapy and detoxification.
Treatment of chronic periostitis
Chronic periostitis is a sluggish infection typical of patients with impaired immunity. If disease is present, the inflamed area is cleaned and physical therapy is prescribed to reduce symptoms and eliminate infection. In particularly difficult cases, the treatment of chronic periostitis may require serious surgical intervention to completely remove diseased tissue. In addition, with this form of flux, it is important to carry out therapy with vitamins and means to strengthen the immune system. An integrated approach stimulates an increase in the body's immunity.
Prevention of osteomyelitis of the jaw
The main role in preventing the development of osteomyelitis of the jaw is played by the following factors:
- prevention of dental diseases;
- timely treatment, prosthetics and dental implantation;
- regular examinations in dental clinics;
- competent and timely treatment of common infectious diseases, especially infectious lesions of the respiratory tract;
- thorough sanitation of wounds resulting from trauma or surgery.
Treatment of osteomyelitis of the jaw bone should be supervised by an experienced physician.
Treatment of periostitis with physical factors
The complex approach to the treatment of periostitis is complemented by the use of therapeutic physical factors:
- ultra-high-frequency therapy (an electromagnetic field, or UHF, acts as a therapeutic factor in inflammatory processes);
- magnetic applicators (magnetotherapeutic treatment of inflammatory processes);
- medicinal electrophoresis (using an electric current of low voltage and low strength, a medicinal substance is introduced into the body as an additional therapeutic factor);
- helium-neon laser rays (have anti-inflammatory, bactericidal, regenerative effects).
Causes of osteomyelitis
Penetration of bacteria into bone, which traditionally occurs as follows:
- against the background of tooth damage by caries, that is, by odontogenic means. First, microorganisms penetrate the pulp, after which they enter the hard tissue through the lymph nodes or canals;
- after fur. tooth damage: dislocations, fractures, operations, etc.
- due to the penetration of infection during ENT diseases, skin inflammation, when microorganisms from one source of inflammation pass into the bone.
Treatment of gumboil with folk remedies
In order not to harm the body, folk remedies for treating flux can only be used for temporary pain relief or as a supplement during the recovery period.
- Infusions of oak bark, sage, St. John's wort, and calendula are used to rinse the mouth (strictly warm solutions).
- Chamomile flower tea is taken orally and is also used as a mouth rinse.
- Honey or honey propolis products are used to lubricate the gums.
In case of treating periostitis at home, you should consult a doctor. In any case, you should not postpone a surgical visit to the dentist when the first symptoms of gumboil appear on the gums or replace medical therapy with self-medication. When treating flux only with folk remedies, inflammation can spread further or develop into chronic periostitis.
With a timely and comprehensive approach to the treatment of periostitis, the disease is successfully cured. However, full recovery will require the help of a qualified dentist, medical procedures and medications.
Why do my gums or cheeks swell?
In most cases, swelling of the gums or cheeks is caused by purely dental reasons:
- Flux
During gumboil, the gums become swollen and painful, and the temperature rises. The development of a tumor begins with an ordinary carious cavity. It gets infected, which eventually leads to tooth decay. Pus accumulates and begins to look for a way out. The cheek swells greatly and a white spot appears on its surface. Without treatment, a fistula forms in this place, and the cheek turns into a huge purulent wound. If you do not seek help from a doctor in time, blood poisoning may occur.
- Removal of a tooth
This operation inevitably involves damage to soft tissue, and swelling is a natural phenomenon. After a while it subsides. If this does not happen, and the gums swell more and more, then you need to urgently visit a doctor. Causes of severe swelling can be:
- a large accumulation of pus,
- incipient periostitis (inflammation of the periosteum),
- infection in the wound.
If you notice swelling of the cheeks and gums, or tissues of the oral cavity, then you need to consult a dentist.
The doctor will determine the exact cause, begin treatment or refer you to another specialist.
Leave your phone number. The clinic administrator will call you back.
By leaving a request on the site, you consent to the processing of personal data
Make an appointment
Initial consultation with a dentist
For free!
- Inflammatory infiltrate
It usually occurs against the background of pulpitis or periodontitis. Pus begins to accumulate in the soft tissues, which causes the appearance of phlegmons and abscesses. It is considered a very dangerous disease because it can lead to big troubles.
- Periodontal disease
Swelling is accompanied by aching or sharp pain. There is no conservative treatment; surgical intervention is necessary. Often it is necessary to remove some teeth and install dentures.
- Teeth chips
The sharp edges of a destroyed tooth begin to scratch the inner walls of the cheek, which leads to inflammation and severe swelling.
- Wisdom tooth growth, pericoronitis
The eruption of the figure eight often leads to inflammation of the gingival hood. Swelling, as a rule, extends to both the cheek and gum.
- Carious teeth
Advanced caries often causes not only the gums to swell, but also the tonsils and cheeks. After eliminating the cause, the swelling gradually goes away. Folk remedies are useless here; urgent medical help is needed.
- Cyst
Depending on the type of cyst, its shape, and location, the doctor decides on conservative or surgical treatment. In some cases, a consultation with an oncologist may be required.
- Gum disease
Swelling is one of the main signs of inflammation of periodontal tissue. Without treatment, the disease quickly becomes chronic and difficult to treat. There is a high chance of losing a tooth.
In addition to the reasons listed, swelling of the gums and cheeks can be caused by:
- inflammation of the facial nerves;
- pathologies of the maxillofacial skeleton;
- allergies;
- disruption of the immune system;
- inflammation of the submandibular and parotid lymph nodes as a result of an infectious disease;
- malignant neoplasm;
- facial injury;
- diseases of internal organs, such as the heart;
- eye diseases;
- blood pathologies.
Diagnosis of osteomyelitis
It is carried out exclusively by a dentist, based on clinical and laboratory studies. Differential diagnosis is also involved.
Basic methods for diagnosing pathology:
- general and biochemical blood tests;
- general urine analysis;
- X-ray of the jaw;
- MRI of the jaw;
- bacteriological examination of purulent contents of fistulas;
- research for diseases that led to bone destruction.
Classification of the disease, depending on the location of inflammation. process
- Jaw osteomyelitis after tooth extraction. The nerve endings of the periodontium and gums remain irritated, pain can be felt immediately or after several days.
- Odontogenic osteomyelitis of the lower jaw is the most common form of the disease at an advanced stage of caries. Quite common in young children.
- Odontogenic osteomyelitis of the upper jaw is caused by the anatomical structure of the bone. The infection can provoke inflammation of the maxillary sinuses. If the fang becomes inflamed, it swells, including the infraorbital area.
- Osteomyelitis of the socket is an inflammation of the bed where the extracted tooth was located. A more correct name for the disease is alveolitis, which is accompanied by destructive changes in the bone.
- Hematogenous osteomyelitis of the jaw - affects mainly the upper jaw, after which it affects the cheekbones and nasal bone. The clinical picture is characterized by sepsis, which is accompanied by inflammation in more than half of patients with this diagnosis.