Pain in the liver refers to complaints ranging from discomfort in the right hypochondrium to intense (in some cases continuous) pain. Interesting fact: the liver itself cannot hurt - anatomy does not allow it. There are no pain receptors on it; nature did not provide them. The pain symptom is caused by its shell (capsule) or neighboring organs, which may signal a problem. The best way to notice the “approaching disaster” in time is to undergo a special diagnosis, which will be prescribed by a gastroenterologist.
Why does pain occur? Even the most minor deviations in the organ change its size, which contributes to the stretching of the membrane on which there are receptors. Pathology of the pancreas, gallbladder, bile ducts can also be accompanied by pain in the right hypochondrium.
Pain and discomfort in this organ are of a different nature: aching or cutting pain, constant or short-term, it can intensify from excessive stress, appear after taking even a small amount of fatty or spicy foods, or in stressful situations. Sometimes a painful symptom in the right hypochondrium is accompanied by flatulence, stool problems, heartburn and bad breath.
If the disease is in a period of exacerbation, the temperature may rise, severe weakness and headache may appear.
Why do my joints hurt?
Many infectious and viral diseases can cause quite serious complications on the joints.
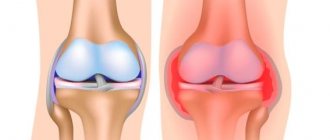
Coronavirus is no exception: many patients complain of persistent pain after suffering from COVID-19. There's nothing new about this, it's just a different virus. We often treat viral arthritis, in particular, and against the background of influenza, there is articular syndrome - an inflammatory reaction of cartilage tissue, the synovial membrane of the joints. Articular syndrome during treatment can go away completely without a trace, or it can turn into a chronic autoimmune pathology. Against the background of coronavirus infection, rheumatological diseases of the connective tissue (rheumatoid arthritis, systemic lupus erythematosus, gouty arthritis, osteoarthritis and others), which were not so much of a concern before, may worsen. Patients often complain about health problems that they have never had before. Why do joints suffer so much after coronavirus? Firstly
, COVID-19 “hits” our entire body.
The musculoskeletal system may also suffer, since all the forces of the human immune system are spent fighting the virus. Secondly
, the coronavirus targets where it is “weak”: perhaps you might not even be aware of some problems.
Thirdly
, any virus, when it dies in the body, “does not go away” without a trace: the components of the virus become a target (antigens) for immune cells, which begin to produce special proteins (antibodies) to neutralize them. These processes can cause the development of an autoimmune inflammatory process not only in the joints, but also in other structures of the human body.
Where do the roots of pain go?
Most people know only the loudest and most terrible diagnoses: arthritis, rheumatism, arthrosis. But, as a rule, such verdicts are made already at those stages when pain persists even after minor movements and at rest. The causes of discomfort after training are often not associated with pathological processes inside the joint, but cover the upper part of the chain - the joint capsule, ligaments, innervation.
h2>Pain in the elbow joint after physical activity
Pain in the elbow joint after physical activity often indicates the development of pathologies such as:
- Epicondylitis is inflammation of the tendons of the elbow tubercle. In this case, pronounced pain appears when bending the arm, and the root of the problem is considered to be injuries and professional characteristics - small but frequent loads on the elbow joint. Because of this, the disease is called “tennis elbow.”
- Sprain of intra-articular ligaments is diagnosed during training injuries; untrained people belonging to the first risk group are especially susceptible to this.
- Pinched nerve in the elbow area, a characteristic feature of which is numbness of the wrist and little finger.
- Osteochondrosis of the cervical and thoracic spine also often causes pain in the elbow joints. The basis for this is created by the infringement of the nerve roots by intervertebral discs.
- Bursitis is an inflammatory process in the connective tissue membrane surrounding the joint. Its roots grow from injuries to the elbow tubercle, overstrain of the ligaments and muscles of the shoulder.
The early stages of arthrosis and rheumatism can also manifest as increasing pain after physical activity. They are often the result of disorders in the joint-muscular mechanism.
Pain in the knee joint that occurs after running or squats represents a whole area of research for an osteopath: the complexity of the device, the presence of many predisposing factors require careful diagnosis not only on MRI and X-ray, but also by an osteopath, whose sensitive hands are able to determine the role of each link in pathological process.
Post-Covid difficulties
Often, joint pain due to covid infection can be localized in the hands - aching and pulling.
In the morning, my fingers seemed to be constrained, as if they were wrapped in tight gloves. Some patients complain of muscle pain, a feeling of weakness, lethargy and migrating pain in large joints. A sick person cannot remain in an upright position for a long time or sit without support, and it is often difficult to move without assistance. This unpleasant feeling persists even after discharge from the hospital; patients will need a lot of recovery time to return to their normal lifestyle.
Coronavirus can “trigger” an autoimmune reaction that will develop into a chronic disease. For example, rheumatoid arthritis: a person’s immune system has been “broken” when it begins to attack its own tissues, “confusing” them with a virus. An infectious disease becomes one of the provoking factors for the development of disease in the joints.
Rheumatoid arthritis often manifests itself as stiffness in the affected joints - usually goes away in the morning with a light workout, but sometimes persists throughout the afternoon. Joint pain is constant and worsens with movement. Most often, at the onset of the disease, the small joints of the hands are affected, followed by pain and swelling in the larger joints.
Shoulder pain after a fall? Reason to consult a specialist
Fans of alpine skiing, snowboarding and many other “extreme” sports often encounter a rupture of the acromioclavicular joint (ACJ). Usually it happens like this: I was rolling, fell, and got bruises on my shoulder and shoulder blade. When performing an R-graphy of the shoulder joint, it turned out that the AC joint was damaged. The formulation of the diagnosis can be different: complete or partial rupture. In the first case, surgical treatment is indicated, in the second, it is possible to limit oneself to conservative therapy.
Damage is classified according to severity:
- I degree - a tear of the acromial clavicular ligament is characterized by pain in the projection of the acromial clavicular joint. No visible damage is noted on R-grams; sometimes there is a slight (2-3 mm) widening of the joint space compared to the healthy limb. The coracoid ligament is intact;
- II degree
-
rupture of the acromial clavicular ligament, tear of the fibers of the coracoid ligament. The injury is characterized by pain in the projection of the clavicular-coracoid joint, protrusion of the acromial end of the clavicle, and a positive “key” symptom. On R-grams there is a widening of the joint space of more than 5 mm. The upper edge of the clavicle projects above the acromion to half its diameter; - III degree
-
rupture of the acromial clavicular and coracoid ligaments is characterized by pain and dysfunction of the upper limb. The “key” symptom is sharply positive, abduction of the upper limb is limited. On R-grams there is a pronounced widening of the joint space (more than 7 mm). The clavicle is displaced upward by more than the diameter of the acromion; - IV degree
-
rare cases - posterior dislocation, enucleation of the acromial end of the clavicle like a “banana peel”, etc. (2) Based on the time elapsed from the moment of injury, injuries are divided into: fresh - no more than 3 days have passed since the injury; stale - from 3 days to 3 weeks; old - more than 3 weeks.
First and second degree ruptures are treated conservatively, using a scarf or bandage on the shoulder joint. The patient is prescribed nonsteroidal anti-inflammatory drugs in ointment and tablet forms, and simple local hypothermia (applying an ice pack to the site of pain on the first day after the injury).
The main symptom of injury to the AC joint is pain in the shoulder joint and shoulder girdle, from mild pain with a minor sprain of the shoulder ligaments to severe pain with a complete rupture of the AC joint. The second and third degree of rupture is accompanied by local swelling and the formation of a bruise - a hematoma. A “highness” appears in the area of the shoulder girdle, and clicking sounds in the shoulder when moving the hand.
The treatment option for a third-degree tear is chosen by a traumatologist. Conservative treatment or surgical intervention is possible. Complete rupture of the ligaments triggers degenerative post-traumatic changes in the acromioclavicular joint and contributes to the development of arthrosis. In sports medicine, a complete 3rd degree rupture of the AC joint is almost always eliminated with the help of surgery (bone reposition and fixation in the anatomical position with a metal structure). After restoring the integrity of the ACJ, the metal structure is removed.
After the operation, physiotherapy (laser therapy, electroanalgesia and magnetic therapy) is prescribed. Superficial massage is useful to relieve muscle spasm and swelling.
The development of movements in the shoulder joint begins with passive exercises (the movements of the patient’s arm are performed by a physical therapy doctor) and active movements 6-8 weeks after restoration of the anatomical integrity of the injured segment.
It is important to understand that “clavicle subluxation” is a relative term. When the AC joint ruptures, all ligaments in this area are affected. A frivolous attitude towards shoulder pain after a fall or incorrect therapy can lead to very sad consequences.
Make an appointment with a traumatologist-orthopedist
Traumatologist-orthopedist - Tarasov Roman Alekseevich
Traumatologist-orthopedist - Gorbachev Oleg Nikolaevich
How to treat joints
First of all, it is worth noting that there is no universal treatment regimen for joint disease, including after coronavirus.
Post-Covid joint syndrome manifests itself in very different ways; the treatment and rehabilitation program will be selected individually. “The treatment will require comprehensive treatment. If after coronavirus a patient experiences severe joint stiffness, pain and swelling, they should consult a doctor to rule out the onset of rheumatoid arthritis. You shouldn’t self-medicate,” comments Leonid Kurzov, chief physician at the Canon clinic.
The primary task of the doctor in this situation is to clarify the cause of the joint syndrome, alleviate the symptoms, and stop the further development of the joint disease. Alas, in approximately every third case, reactive arthritis and some other joint inflammations can become chronic. But with active interaction between the attending physician and the patient, who strictly follows the recommendations of doctors and takes care of his health, joint disease can be in remission for many years.
Treatment
To temporarily relieve pain in the liver, patients take painkillers and antispasmodics on their own. Always remember that they can only be used after examination and recommendations from a specialist. Treatment is prescribed only after thorough diagnostic studies. Since many liver diseases have a similar course, it is necessary to make a correct diagnosis.
Before visiting a doctor, do not take painkillers or antispasmodics. They will mask important symptoms and make it difficult to make a diagnosis during examination.
Under no circumstances should you select medications yourself. And especially do not take medications prescribed to your friends in similar situations. There is no guarantee that the drugs that help them won't make things worse for you. Treatment is selected strictly individually.
To deal with this situation, consult a doctor as soon as possible. Our center is equipped with modern research equipment. This helps specialists make an accurate diagnosis and prescribe effective treatment as soon as possible.
Before visiting a doctor to relieve pain symptoms (instead of taking medications), pay attention to your diet. You can independently reduce the load on the organ.
The diet to eliminate pain in the liver should be gentle and low in fat.
- It is recommended to eat: black bread, low-fat dairy products, various cereals, vegetables and fruits, boiled meat and poultry (beef, chicken).
- it is necessary to completely exclude: fried, spicy smoked, and fatty foods, baked goods, mushrooms, pork, duck, canned food, confectionery, coffee.
In some cases, diet helps much more effectively than drug therapy.
The best diagnosis of pain in the liver is MRI of the liver and MRI of the gallbladder. To identify health problems in the early stages, doctors recommend periodically undergoing a full comprehensive examination of the body.
The contents of this article have been checked and confirmed for compliance with medical standards by a gastroenterologist of the highest qualification. category Grankova Tatyana Mikhailovna.
Prices
| Name | Price |
| Primary appointment (examination, consultation) with a general practitioner | 2 200 ₽ |
| Repeated appointment (examination, consultation) with a general practitioner | 1 900 ₽ |
Harmful exercises
Below you will see harmful exercises and their replacements.
Abduction of arms with dumbbells to the side above parallel with the floor
A particularly dangerous option is lifting the dumbbell to the side while being at an angle to the support - in this position the arm automatically rises above the shoulder line:
A safe option: lifting dumbbells to the sides until your shoulder is parallel to the floor. Raising dumbbells to the sides on an incline bench.
Bench press
Safe: Barbell chest press, dumbbell overhead press.
Close-grip barbell row to the chin
Safe: row with dumbbells with a shoulder-width grip strictly until the shoulder is parallel to the floor.
Sources:
- 1972. Cunningham's Textbook of Anatomy. Oxford University Press, London.
- Almekinders, L.C. 2001. Impingement syndrome. Clin. Sports Med. 20:491-504.
- Behnke, R. S. (2006). Kinetic anatomy. (2 ed., pp. 35-56). Champaigne, IL: Human Kinetics.
- Bigliani LU, Morrison DS, April EW: The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans 10:228, 1986.
- Morrison DS, Bigliani LU: The clinical significance of variations in acromial morphology. Orthop Trans 11:234, 1987.
- Page, P., Frank, C. C., & Lardner, R. (2010). Assessment and treatment of muscle imbalances the janda approach. (pp. 195-207). Champaigne, IL: Human Kinetics.
- Sahrmann, S. A. (2002). Diagnosis and treatment of movement impairment syndromes. (1 ed., pp. 193-261). St. Louis, MO: Mosby.
- Wilk, K. E., Reinold, M. M., & Andrews, J. R. (2009). The Athlete's Shoulder. (2 ed.). Philadelphia, PA: Churchhill Livingstone.