01.12.2020
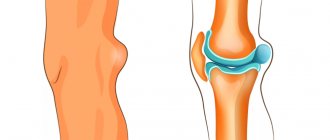
A Baker's cyst is a ball-shaped lump on the back of the knee joint. At its core, a cyst is a popliteal capsule filled with fluid. When the knee joint is bent, the ball is practically invisible. But when it is extended, the seal comes out and it becomes possible to palpate it.
The size of a popliteal hernia can reach 10 cm. Despite the fact that this disease is a benign tumor, at the same time this pathology can be classified as dangerous due to possible complications. The disease occurs in both adults and children. In its advanced state, Baker's cyst negatively affects a person's musculoskeletal system and can lead to the need for surgical intervention.
About the disease
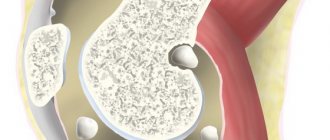
For more than 100 years, there have been discussions in orthopedics regarding the etiopathogenesis of the cystic element. Over time, based on many factors, scientists agreed on a common opinion: Becker cyst
under the knee is definitely of a synovial nature. Formation can occur not only after intra-articular damage to this part of the leg, but also against the background of complete well-being, without previous trauma.
Schematic illustration.
Prevention
To avoid the development of such a pathology, it is recommended to practice the following preventive measures:
- Avoid injury, and if you receive any knee injury, consult a doctor immediately.
- When practicing traumatic sports, use special bandages and knee pads.
- Timely diagnose and treat all diseases of the musculoskeletal system.
- Before starting any sports activity, do a warm-up, including stretching exercises.
- Do not overexert yourself during training, practice loads that are adequate for your health and age.
- Eat right, eating foods that are good for bones and joints.
- Choose high-quality and comfortable shoes.
Those who have undergone surgery to remove a cyst need to carry out the rehabilitation process correctly. As a rule, this period takes up to 10 days. At this time, it is important to follow all the doctor’s recommendations, engage in physical therapy, and take prescribed courses of physical therapy.
At first, you should walk less and, if necessary, move with a cane.
Reasons for development
Popliteal bursitis is characterized by various etiologies. Doctors associate the development of the pathology in question with previously suffered arthritis (usually of rheumatoid origin) and severe gonarthrosis. The causes of Becker's cyst in 1948 were even associated with brucellosis . It was also confirmed that neoplasms can form against the background of pigmented villous synovitis, chronic microdamage to the joints.
The relationship between popliteal protrusion and other pathological processes occurring inside the joint has been proven. They are degenerative-dystrophic or rheumatic in nature and lead to the development of chronic synovitis. It is recognized as a predisposing factor to the development of popliteal hernia. The condition contributes to increased intra-articular pressure.
Attention! At the stage of consultation with a doctor, you need to report all injuries to your legs, especially recent ones.
Many orthopedists and rheumatologists say that popliteal bursitis never occurs in people who do not have a history of any type of knee injury.
Pathogenesis
The mechanism of development of this pathology is associated with the structural features of the knee joint and popliteal fossa. Studies show that in approximately half of the cases in healthy people, intertendinous mucous bursae are located between the tendons of the semimembranous and gastrocnemius muscles. This is not considered a pathology, but an anatomical feature.
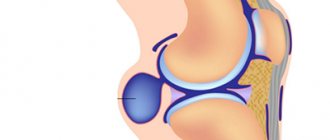
When, for certain reasons, a pathological process develops in the knee joint, the body reacts to it with the formation of excess fluid - a kind of protective reaction of the body from subsequent possible complications. When a relatively large amount of fluid accumulates, it leaks through the valve mechanism into the intertendinous bursa. As a result, its size increases.
Valvular manism allows fluid to flow from the knee joint into the cyst, but its reverse flow is impossible.
The walls of the cyst are similar to synovial tissue with obvious fibrosis, and signs of chronic nonspecific inflammation may also be observed. Due to the presence of fibrin, the fluid in the cyst may be thick. This suggests that the formation could be the result of a joint injury.
Classification and symptoms
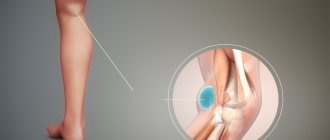
The neoplasm can be single-chamber, double-chamber and multi-chamber. Doctors have found that relapse of formation occurs in cases where there are multiple chambers in a cystic neoplasm. As the size of the bulge increases, the risk of it spreading to the lower leg increases. However, the considerable volume of the tumor provokes another consequence - rupture. A photo of a Becker cyst under the knee will help you understand the size of the formation that is considered threatening.
External sign.
The disease is classified into the following subtypes:
- Symptomatic form - the course of the pathological process is characterized by severe pain. Its localization is the knee joint.
- Idiopathic form - when the origin of the development of the disease is unclear, and it is not possible to establish the root cause even after conducting numerous types of research.
Absolutely asymptomatic development of popliteal bursitis is observed in no more than 28% of clinical cases . It is the absence of pronounced signs as atheroma forms and then develops that explains its late detection. Detection of neoplasms no earlier than stage 2 occurred when the inflamed areas were small in size.
Symptoms of a Becker cyst under the knee:
- Prolonged pain, often periodic, occurring inside the popliteal fossa immediately after physical activity.
- Feeling of discomfort, stiffness inside the limb, difficulty straightening the knee joint.
- Large formations compress the neurovascular bundle, causing swelling of the ankle joint.
- A rounded neoplasm can be felt under the knee - it is not fused to the skin.
- Performing several flexions and extensions helps to increase the size of the protrusion.
- Minor manifestations of neuropathy of the tibial nerve, when it, being large in size, pinched it.
The difficulty in identifying the etiological factor is associated with the anatomy of the knee joint, since synovial bursae, pockets, and inversions are located in this area. According to experts, the presence of multiple physiological structures complicates the early detection of the tumor. Also, this factor does not allow us to timely trace which particular anatomical part was the root cause of the development of the hernia.
The morphometric features of atheroma, regardless of the age and gender of the patient, are individual. Within the same age group, the volume of the hernia varies.
What is a Baker's cyst?
Baker's cyst is a pathological neoplasm that involves the accumulation of varying volumes of fluid in the synovial sac, which is localized on the back of the knee joint.
The morphological signs of the existing pathology allow us to assert the benign nature of the formation, without classifying it as a cancerous tumor.
Popliteal synovial cysts most often occur when the patient has an intra-articular disease, such as osteoarthritis. The formation can have a different size (from 2 mm or more) and occurs at any age.
Diagnostics
Before you plan how to treat a Becker cyst
under the knee, you will need to exclude the presence of a tumor process. To clarify the actual clinical situation, the following methods are used:
- Blood test (clinical, biochemical).
- Determination of blood sugar.
- X-ray research method.
- Ultrasound is a safe, very informative and inexpensive diagnostic method. Considering the high effectiveness of the method, the use of ultrasound has acquired leading importance in the examination program. The method is actively used for the purpose of differential diagnosis. The characteristics of synovial cysts are compared with other possible pathologies of the popliteal region. At the end of the procedure, the patient receives a photo of the Becker cyst.
- Computed tomography and nuclear magnetic resonance in clinical practice are not performed for popliteal hernia. They are discovered completely by chance, during the examination process. The reason for patients to consult a doctor is to clarify the cause of discomfort inside the popliteal region.
Cyst on MRI.
Diagnostic punctures and then examination of synovial fluid are carried out if there are appropriate indications. An ECG is performed during preparation for surgery.
Why is MRI better?
If a tumor is suspected, doctors recommend magnetic resonance imaging, especially if the nature of the tumor is not clear. This diagnostic method allows you to establish the exact size and location of the tumor, as well as find out the nature of the formation (whether it is malignant or benign).
MRI has the following advantages:
- The diagnostic process does not harm the body, since magnetic fields do not have a negative effect on the body.
- During magnetic resonance imaging, no pain or discomfort is felt.
- MRI does not cause side effects and has almost no contraindications.
Please note that magnetic resonance imaging has no age restrictions. However, it is not recommended to carry out diagnostics on infants - it is difficult for babies to lie still.
Conservative therapy
An orthopedist is involved in eliminating the type of pathology in question; if the need arises, surgeons are involved in the implementation of the therapeutic process.
Conservative treatment of Becker cyst under the knee involves the following approaches:
- unloading the joint;
- physiotherapeutic treatment;
- puncture of the tumor, followed by evacuation of the contents and administration of medications.
For therapeutic purposes, sclerosing agents are administered, in particular, a 5% alcohol solution of iodine, hormonal, and cytostatic drugs are used.
- Physiotherapeutic treatment . Electrophoresis and UHF are recognized as the most effective methods. It is permissible to implement these treatment options only after excluding an oncological process.
- Puncture . Performed to evacuate the contents of the hernia. When the tumor reaches stage 2-3, the contents of its capsule have a jelly-like consistency. The compacted neoplasm is difficult to puncture and subsequent evacuation of the internal part. Also in this case there is no point in administering corticosteroids.
- A positive result is provided by hormonal treatment . Cortisone therapy is effective in 50% of all clinical cases. The scientific idea of using hormonal drugs was first developed and applied by rheumatologists. Patients with a hernia that occurred against the background of rheumatoid arthritis were subject to observation. Therapeutic tactics made it possible to evaluate that after intra-articular administration of glucocorticosteroids, the size of the tumor decreased.
Pumping out liquid.
Since then, hormones have been injected directly into the popliteal swelling. Hydrocortisone emulsion was actively used, combining it with antibiotics.
Important! If the patient has hormonal diseases - problems with the thyroid gland, diabetes mellitus, a disorder of the adrenal cortex - it is necessary to inform the doctor about the existing disorders.
of Becker cyst is not always possible
leads to complete elimination of the tumor. Statistics show that in 6 out of 10 cases, the atheroma has to be excised surgically. Such results serve as the basis for the search for new therapeutic approaches and the development of more effective conservative methods of therapy.
How is an MRI performed?
Magnetic resonance imaging is performed in closed-type tomographs. Before starting the diagnostic test, the doctor gives a short briefing.
The operation of the tomograph is accompanied by loud noise. At the patient's request, earplugs or special headphones can be used.
To obtain clear and informative images, the patient must remain as still as possible.
There is lighting and ventilation inside the tomograph. To contact a specialist, use speakerphone. In cases where the patient feels unwell and wants to immediately leave the tomograph, you can use the panic button, which will stop the diagnostic process.
Upon completion of the instructions, you can begin magnetic resonance imaging. First, the patient needs to change into clothes without metal inserts, take off his shoes and lie on the table on his back. If necessary, the doctor injects a contrast agent into the vein. Arms and legs are usually fixed to avoid unwanted body movements. The duration of the manipulation is about 30-40 minutes, after which the patient must wait while the specialist interprets the results and prepares a conclusion.
Surgical intervention
The intervention can be open or endoscopic. Open surgery involves isolating the tumor from the surrounding tissues to the anastomosis with the knee joint, after which surgeons bandage the neck and cut off the atheroma.
Surgical intervention does not always immediately give a positive result, and the recovery period proceeds without complications or complaints.
Open removal of formation.
The main concern of patients is associated with certain pathological phenomena, including:
- some feeling of a foreign object under the knee;
- inability to straighten the leg;
- difficulties with limb function;
- pain syndrome of varying degrees of intensity;
- movement of goosebumps along the surface of the leg (paresthesia);
- the ankle joint becomes cold to the touch.
The degree of manifestation of symptoms depends on the individual characteristics of the human body and its sensitivity.
Criteria for evaluation
Outcome measures are used to define and evaluate the expected results of a therapy/procedure, which must be compared with the results found in the patient.
- Western Ontario and McCaster University Pain Subscale (WOMAC) : a multidimensional instrument that measures 17 functional activities, 5 pain-related activities, and assesses joint stiffness. It measures pain and dysfunction.
- Visual analog scale (VAS) : measures pain from 0 to 10 (no pain to severe pain). It is easy for the patient to determine what level of pain they have.
- Rauschning and Lindgren classification : used to evaluate outcome and therapeutic effectiveness (0 to 3).
- Newcastle-Ottawa scale : a simple scale for assessing the quality of non-randomized controlled trials.
Endoscopic treatment
Currently, the combination of endoscopic intervention and therapeutic and diagnostic arthroscopy of the knee joint
. This combination of techniques allows you to achieve the following results:
- Quickly relieve pain even of high intensity.
- Completely restore mobility of the knee joint.
- Minimize length of hospital stay.
- Reduce the likelihood of developing popliteal postoperative scars.
For several years now, doctors have been comparing the results of open and endoscopic surgery. The opinion of specialists is ambiguous, since all clinical cases are individual.
Comparison of endoscopic and traditional, open surgery (10 patients participated in the observation).
| Evaluation criterion | Endoscopic surgery | Open surgery |
| 55.6% of patients did not complain of pain in the knee joint on the first day after surgery. 33.3% noted pain of moderate intensity in the first 2 days after surgery, but the discomfort was quickly relieved with analgesics. 11.1% noted pain for the first time after knee surgery only on the 3rd day. | The pain was severe, attacks were repeated frequently, and required the mandatory administration of analgesics. |
| Minimum 5 days. | Minimum 7-8 days. |
| Minimal. | High. |
| Full extension in all patients was observed already in the first 24 hours after surgery. In 22.2% of them, flexion was absolutely painless, reaching over 90°. In 38.9% of patients, activity was restored within 2 days after the intervention. In 16, In 7% of patients, knee flexion began to be restored 72 hours after surgery. The functional ability of the knee joint was fully restored in 90% of those operated on within 14 days after the intervention. | The full range of motion in the joint was restored in only 1 patient by 14 days after the intervention. In 56.3% - after 30 days, in 25.5% - only after 60 days. |
| Swelling is insignificant, the likelihood of hemorrhages is practically absent, and the formation of postoperative scars is excluded. | During the postoperative recovery period, a subcutaneous hematoma occurred in 68.8% of patients. In 50.3% of patients, severe swelling was noted under the knee, which also extended to the medial head of the gastrocnemius muscle. In 18.7% of operated patients, a hypertrophied scar formed, which led to tissue adhesion under the knee. The pathological phenomenon caused the formation of flexion contracture at 165° and 175°. |
MRI with contrast
In some cases, your doctor may prescribe a contrast-enhanced magnetic resonance imaging scan. For example, this is relevant in cases where the Baker cyst has not completely formed and the nature of the neoplasm is not entirely obvious. Also, magnetic resonance imaging with contrast can identify concomitant diseases.
Contrast agents are absolutely safe for the patient's body. The drug is injected into a vein immediately before the start of magnetic resonance imaging. This makes it possible to improve the information content and clarity of images several times.
The contrast does not accumulate in tissues and completely leaves the body within 24 hours. The study is absolutely safe - however, only if you have consulted with your doctor in advance and ruled out any contraindications.
Possible complications
In the absence of timely adequate therapy, complications are possible. The most common consequences of the pathology in question are:
- Cyst rupture. After the integrity is broken, the liquid flows out of the formation. It penetrates into the interfascial spaces of the calf muscle fibers. A similar complication is recorded in every 10 sick people.
- Acute pain, swelling of the affected area. These signs appear after the cyst ruptures. Swelling is found in the back of the leg. The rupture is also accompanied by redness of the dermis of the lower leg. A local increase in temperature is possible.
- Thrombophlebitis (inflammation of the vein walls).
- Difficulty in the outflow of blood through the veins of the leg.
- Thrombosis. A blocked vein becomes blocked by a blood clot.
- Deposition of calcium salts inside the cyst. This process causes the cyst to become denser. It begins to put more pressure on the surrounding tissue.
- Varicose veins of the saphenous veins of the leg.
- Compression of the tibial nerve. In this condition, the patient feels weakness, tingling, and numbness in the lower part of the limb.
Education pathology
A special feature of education is its ability to develop back. A person may have a Baker's cyst in the popliteal region throughout his life. It is also possible that it will only exist for a few months. Self-resorption of fluid is observed when cysts form after constant physical exercise. loads during sports.
The pathology in question was called Baker's cyst because it was William Baker (Becker) who published the first detailed reports regarding synovial cysts. This happened in the 19th century. Baker was an English surgeon.
The specialist found that Baker's bubble (popliteal fossa) is more often found in older people. To know what a popliteal fossa synovial cyst looks like, check out the pathology photo.
Size
Education is small in size. Therefore, it is almost impossible to notice. If the bubble is large, it can be easily detected visually. It is represented by a dense, elastic formation. The tumor usually has an oblong shape. On top of the neoplasm, the dermis remains unchanged. Her color is normal. There is no adhesion to the underlying tissues.
Diseases of the knee joint that are inflammatory in nature, as well as injuries, can provoke such a pathology. But in most cases, doctors cannot accurately determine the cause of the tumor.