In most cases, recurrence of intervertebral hernia in patients occurs 2-3 years after the operation. The reasons for this phenomenon are that the operation is not inherently a therapeutic measure. They do not stop the process of destruction of the spinal column, do not eliminate defective areas of the intervertebral discs, and do not start the process of tissue regeneration. Surgery by removing part of the disc or the entire fibrous ring only worsens the patient's situation. But in the first two years this is not noticeable, since the crippled spine tries to adapt to new realities and redistribute the increased shock-absorbing load.
What happens during surgery? The herniated disc is removed and two adjacent vertebral bodies are fused. This rigid connection is no longer able to participate in the process of distributing the shock absorbing load. Accordingly, its functions are transferred to the adjacent intervertebral discs. If there are small damages, an accelerated process of degeneration starts in them. After 2-3 years, not single, but multiple hernias appear in neighboring discs.
This is how relapses occur after removal of an intervertebral hernia, which are almost inevitable. Full rehabilitation after surgery can be your salvation. Rehabilitation should be aimed at restoring the health of the spinal column. This can be done with the help of manual therapy. Those patients who underwent treatment with us after the operation did not return again for recurrent intervertebral hernia after the operation, since they completely restored the functionality of the cartilaginous tissues of the spine.
If you have a recurrent intervertebral hernia, then do not rush to make an appointment with the surgeon again. Visit our chiropractic clinic. Each patient has the opportunity to receive an initial consultation with a vertebrologist completely free of charge. During the appointment, the doctor will conduct an examination, study all the medical documentation you have and the results of the examinations performed. You will then be given individual recommendations for rehabilitation treatment and rehabilitation.
Remember that recurrent spinal hernia can be easily treated without surgery. Manual therapy techniques make it possible to completely restore the cartilage tissue of the spine and return the patient to complete freedom of movement.
Causes of recurrent vertebral disc herniation
Recurrence of a disc herniation is not an accident, it is a pattern. And all modern doctors know about this negative trend. The main reason for this phenomenon is that osteochondrosis is a constantly developing degenerative disease, which over time only worsens the patient’s situation. Until the cause of the destruction of the intervertebral disc is eliminated, the hernia will continue to occur.
It is worth paying attention to the following potential causes of the development of osteochondrosis, and, accordingly, the recurrence of a herniated disc:
- poor posture, habit of slouching and hunching, deformation of the spinal column;
- excess body weight, which does not allow you to lead an active lifestyle in which all the back muscles would actively work and supply blood to the cartilage tissue;
- improper diet, which does not allow the body to receive sufficient amounts of all amino acids, vitamins and minerals;
- improper organization of sleeping and working spaces;
- insufficient consumption of clean drinking water;
- degenerative systemic diseases of connective and cartilage tissue;
- inflammatory processes;
- tumors and serious, intractable infections of the tissues of the spinal column (tuberculosis, polio, syphilis, etc.).
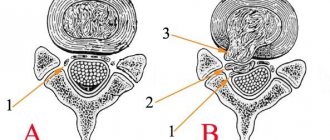
In order to better understand the potential causes of recurrent disc herniation, it is necessary to understand the structure and physiology of the spinal column. It is the main part of the musculoskeletal system of the human body. It consists of vertebral bodies, which are connected to each other by uncovertebral and intervertebral joints. Each vertebra is hollow inside and has an oval foramen. Together they form the spinal canal. In it, under the protection of the dural membranes, there is the spinal cord - the main structural part of the autonomic nervous system, which controls the performance of the entire body and its organs.
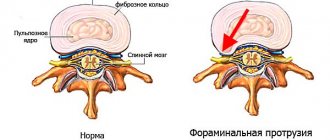
Root nerves, which are necessary for innervation of different parts of the body, depart from the spinal cord. They exit through the foraminal openings in the vertebrae. To protect them, as well as to evenly distribute the shock-absorbing load, cartilage discs are placed between the vertebral bodies.
Each intervertebral disc consists of a dense fibrous membrane (ring) and a nucleus pulposus located inside it in the form of a jelly-like gelatinous body. Taken together, this design provides excellent shock absorption and load distribution, protection from compression of the radicular nerves and surrounding soft tissues by the bone structures of the vertebral bodies.
The only “weak point” of the intervertebral disc is the lack of its own vascular network. Its nutrition is carried out through diffuse exchange between the cartilaginous fibrous ring and the surrounding muscle tissue. Diffuse exchange is possible only in the case of active muscle contraction and relaxation. If the muscular frame of the back is not subject to regular, sufficiently adequate physical activity, then it loses the ability to diffuse exchange.
As a result, the intervertebral disc begins to lose moisture and becomes dehydrated. It loses its usual height and goes beyond the vertebral bodies. This is the stage of protrusion, at which the patient already experiences quite severe pain. The next stage is the appearance of cracks on the surface of the fibrous ring. With strong physical stress (for example, when lifting unusual weights), the fibrous ring cracks and part of the nucleus pulposus comes out through it. This is an intervertebral hernia.
Lack of rehabilitation after surgery leads to the fact that all these processes of disruption of diffuse metabolism between cartilage and muscle tissue are further disrupted. Osteochondrosis progresses rapidly and soon the operated patient experiences a relapse of the intervertebral hernia.
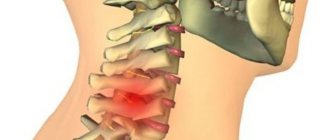
The importance of the cervical spine
The neck, also called the cervical spine, is a long, flexible column that extends across most of the body. The upper part of the cervical spine is connected to the skull, and the lower part of the cervical spine is connected to the upper back at shoulder level. This area is commonly known as the spine or spine. The cervical spine or neck is made up of muscles, nerves, ligaments and tendons of seven stacked bones, which are separated by intervertebral discs, thanks to these discs the spine can move freely.
However, the cervical spine is a small area, but it is one of the most complex areas and plays several important roles in the human body, such as protecting the spinal cord, supporting head movement, and facilitating blood flow to the brain.
How does relapse manifest after surgery to remove a hernia on the spine?
Recurrence of a hernia after spinal surgery appears in a separate perspective. In the first year, the patient experiences some discomfort due to the fact that the process of habitual distribution of shock-absorbing load is disrupted. In most cases, this is a potential reason for further restriction of physical activity. But ultimately, this “careful attitude” regime leads to total degenerative changes in the cartilaginous structures of the intervertebral discs.
How does this condition manifest itself? First of all, you should pay attention to stiffness at certain hours. For example, in the morning, immediately after waking up, you feel a certain stiffness throughout your body and the inability to bend forward or turn in different directions. This is a sign that during night sleep the fluid balance in the intervertebral discs has not been restored and they will try to receive nutrition during the first hours after waking up.
Also, a relapse after removal of a spinal hernia can manifest itself in the form of a constantly present dull pain in the back muscles. It is rarely associated with damage to the radicular nerve structures. Weakness and increased fatigue of the muscular frame of the back gradually develops. The patient notices that it is difficult for him to keep his back straight for a long time, and there is a need for back support while sitting. This sign indicates that the processes of microcirculation of blood and lymphatic fluid in the structure of the muscle fiber are disrupted. Metabolites and lactic acid accumulate in it, and there is no sufficient capillary blood supply. This will inevitably lead to the appearance of new intervertebral hernias in the near future.
At the moment of culmination, relapses after removal of an intervertebral hernia give the following clinical symptoms:
- acute piercing pain at the time of the appearance of a new herniated protrusion of the intervertebral disc;
- a feeling of numbness in certain areas of the body on the affected side;
- sharp limitation of mobility due to the development of radiculitis and compression of the radicular nerve;
- the appearance of areas of hyperesthesia and paresthesia;
- decreased muscle strength in the limb on the affected side.
In severe cases, dysfunction of the cardiovascular, respiratory, urinary, and digestive systems may be observed. When a recurrent hernia is localized in the lower parts of the spine, cauda equina syndrome often occurs. it can cause complete paralysis of the large intestine with the absence of the process of emptying and the bladder, manifested by urinary retention.
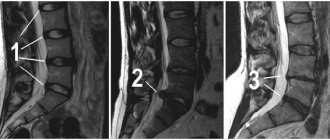
To confirm the diagnosis, it is advisable to take an x-ray of the affected part of the spine and an MRI. An urgent consultation with a neurologist and vertebrologist is also necessary. You can make an appointment for a free appointment with these doctors right now. In our manual therapy clinic, initial consultation with a vertebrologist and neurologist is provided completely free of charge for all patients.
What is cervical spine surgery?
Cervical spine surgery is usually indicated for various types of spinal problems. Neurosurgeons or orthopedic surgeons recommend cervical spine surgery to relieve long-term neck pain, stop unusual head movements, weakness and tingling, numbness, and restore full nerve function.
The surgery is usually performed when the spinal cord or the supplying nerves from the spine are under enormous pressure due to injury, instability, or degenerative disorders. for degenerative disorders, trauma or instability.
Contraindications
However, even if there are strong indications, surgical intervention may not always be performed. If the potential risks from removing a hernia are higher than the likelihood of developing complications of the disease, the operation is not performed. But this does not mean that you will have to forget about it forever and continue to live with constant pain and other symptoms of a hernia.
If there are contraindications, treatment is carried out appropriate to the situation, helping to normalize the body’s condition and sharply reduce the likelihood of unforeseen situations, both during surgery and during the rehabilitation period. If with its help it was possible to achieve normalization of the body’s functioning, the operation is performed. Otherwise, it can only cause harm to the patient or lead to dire consequences.
Surgery is contraindicated if:
- severe general condition of the patient, requiring constant monitoring of vital functions;
- decompensated heart failure and diabetes mellitus;
- hypertensive crisis;
- blood clotting disorders;
- acute infectious diseases, including skin.
Indications for reoperation
The persistence of pain for more than 2 months after surgery, despite anti-inflammatory therapy, is a direct indication for an MRI examination and possibly surgical intervention. That is, it is required for any of the above reasons, except for psychosomatic disorders and the development of spondylitis or spondylodiscitis (risk of development 1-2%).
With prolonged compression of the root, if the disc herniation is not operated on, the following symptoms may appear:
- the occurrence of paresis, decreased severity of tendon reflexes, muscle weakness and malnutrition;
- numbness in the limbs, perineal skin;
- sharp shooting in the legs;
- frequent urinary urgency or urinary incontinence;
- persistent erectile dysfunction in men.
Posterior cervical laminectomy and fusion
Laminectomy means removal of the lamina. The lamina is a very thin plate of bone at the back of the neck that forms the roof of the spine and protects the spinal cord.
The purpose of this surgery is to remove the lamina to make room for the spinal cord.
The posterior cervical laminectomy procedure includes the following:
Surgical approach;
There will be a skin incision along the midline of the back of the neck and 3 to 4 inches long.
Removing the plate;
A high speed burr can be used to create a dimple in the plate on both sides just before it connects to the facet joint.
The plate, as with the spinous processes, is removed as a single unit.
Removing the lamina and spinous process allows the spinal cord to slide back and gives more space.
History of the development of minimally invasive surgical techniques
In 1934, W. J. Mixter and J. S. Barr described the correlation of disc prolapse and clinical syndromes associated with compression of the nerve roots and spinal cord. The authors advocated a surgical method of treating this pathology [11].
In 1939, LG Love presented a description of an approach in which the dural sac was displaced and the nerve root was released by removing the herniation with disc resection [12]. These basic methods are still used today, although the technique has been refined. At the moment, for standard discectomy they use a reduced unilateral 5-cm approach, going around m. multifidi
and the hernia is removed by passing through the intralaminar space.
In 1988, LL Wiltse and WC Spencer [13] described a paraspinal approach for the treatment of extraforaminal disc herniation - it passes between m. multifidi and m. longissimus.
Over the past 30 years, many different techniques have been developed aimed at reducing hernias and muscle injuries, but the general principle remains the same. The main changes concerned reduction of trauma, postoperative period, costs and reduction of rehabilitation time. This was achieved thanks to the improvement of optical magnification and lighting systems.
In 1977, W. Caspar [14] and RW Williams [15] introduced the method of surgical microdiscectomy. The access was reduced to 3 cm. During the operation, distractors for spreading the muscles and a microscope were used for better visualization.
In 1988, P. Kambin and S. Sampson [16] described a fully endoscopic technique based on an extraforaminal approach for non-sequestrated intracanal hernia.
Ten years later, with the aim of treating all types of hernia, K. Foley, M. Smith [17] and J. Destandau [18] introduced a video-assisted technique using a tubular working channel (microendoscopic discectomy) with a 2-cm approach.
In 2002, Yeung and Tsou [19] used an endoscopic technique, which made it possible to eliminate all forms of hernia using a transforaminal approach.
At the moment, debates between supporters of the effectiveness of microscopic and endoscopic techniques do not subside; the question remains open.
LLIF
The LLIF technique, or lateral fusion (Extreme Lateral Interbody Fusion, XLIF), described by BM Ozgur in 2006 [39], is an approach to the disc space through the lateral retroperitoneal, transposal canal. LLIF is applicable in situations that require access to the interbody disc space from T12–L1 to L4–L5. This method is not applicable for interventions at the L5–S1 levels due to the lateral access of the iliac crest. In addition, when the hernia is located at a more caudal level of the lumbar spine, the risk of intraoperative injury increases due to the anatomical location of the lumbar plexus and iliac vessels. The patient is in a lateral position during the operation. The choice of incision point is based on MRI data obtained preoperatively, as well as data from other radiological studies. Neuromonitoring should be performed continuously during access.
LLIF can be used for any degenerative disc changes. This is an excellent approach for correction of sagittal and coronal deformity, especially for lumbar degenerative scoliosis with laterolisthesis [40]. However, LLIF cannot be used in cases of severe central canal stenosis, osteolateral recess stenosis, and severe spondylolisthesis [41]. Pure LLIF, without the use of posterior approaches, should not be used in cases of high biomechanical instability, such as facet arthropathy, deformity and multilevel disease [42]. The lateral approach is also not suitable for patients with previous retroperitoneal surgery, retroperitoneal abscess, or patients with abnormal vascular anatomy. Disadvantages include the potential risk of injury to the lumbar plexus, blood vessels, psoas muscle, and intestine, especially at the L4–L5 level [29]. It is worth noting that bleeding that occurs during LLIF surgery is difficult to control [40, 43] (Fig. 5).
conclusions
Endoscopic techniques can compete with standard, more traditional methods by reducing operative time, shorter hospital stay, smaller incision and blood loss, less tissue trauma, lower need for opioid analgesics, and faster return of the patient to daily activities.
The recurrence rate observed with endoscopic discectomy in short-term follow-up remains within the range expected for microdiscectomy. This procedure is likely to achieve more favorable results in cases of new disc herniation and recurrent disc herniation.
By using a more posterolateral trajectory, endoscopic discectomy does not cause deformation of the extensor muscles, and if the intervention is unsuccessful (or the patient subsequently develops a hernia at another level), the surgeon can perform a standard microdiscectomy using a posterior midline incision and laminotomy, since This area remains intact.
Surgical procedures can be performed under local anesthesia, which eliminates the risks of general anesthesia, and, by definition, should reduce the associated risk of venous thromboembolism; however, shorter operative time has not been clearly documented and in reality is probably not clinically significant in itself. All these objective parameters are valid only during the early observation period - up to 3 months, while long-term results (as evidenced by more subjective clinical parameters - pain, dysfunction and disability) do not differ from these indicators with microdiscectomy.
The disadvantages of the endoscopic method are the long training period for a new procedure, the high costs of purchasing equipment (high-definition TV camera, high-resolution TFT monitor, dual-screen image intensifier, instruments, irrigation control system and radiofrequency probes for hemostasis) and consumables.