Subtalar dislocations
Subtalar foot dislocations predominantly occur medially. Dislocations of the foot outward, posteriorly and anteriorly at the subtalar joint are extremely rare.
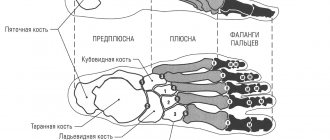
Subtalar dislocation of the foot medially occurs as a result of the simultaneous and even action of forces, during which strong inversion, adduction and plantar flexion of the foot occur. As a result of this, ligament rupture occurs, the foot is displaced in the talocalcaneal and talonavicular joints, and the calcaneus, together with the forefoot, is displaced medially (Fig. 205) in relation to the talus, which remains clamped in an equinus position in the ankle joint. Subtalar dislocations are combined with fractures of the head of the talus and fractures of the scaphoid. Internal subtalar dislocation of the foot is observed when falling on the outer edge of the foot.
Symptoms and recognition. Characterized by a rapidly growing hematoma, swelling, and movement in the foot is impossible. The foot is displaced inward and rotated outward in such a way that the sole faces the healthy limb and the outer surface of the foot faces downward. The outer ankle protrudes sharply outward, and there is a recess underneath it; the head of the talus is located in front of the outer malleolus; The inner edge of the calcaneus protrudes under the inner malleolus. Symptoms of impaired blood supply to the foot are observed. X-ray examination is crucial for diagnosing foot dislocations.
Treatment. Reduction of subtalar foot dislocations is often very difficult and must be performed under general or intraosseous anesthesia. Reduction must be started as soon as possible, since increasing swelling in the future makes it extremely difficult. In addition, bony protrusions can break through the skin stretched over them and cause bedsores. These complications significantly worsen the prognosis. The patient is placed on the operating table. The shin is bent at the knee to a right angle. Using a sheet, counter-traction is created on the thigh, and in addition to this, one assistant holds and pulls on the upper part of the lower leg. When realigning, movements are made that are opposite to those that led to this type of subtalar dislocation. To do this, the surgeon covers the heel with one hand and the forefoot with the other. The foot is strongly bent in the plantar direction, turned in the abduction position, trying to move it into place. After reduction, a plaster cast is applied from the middle of the thigh to the fingertips. The knee is fixed at an angle of 150°, and the foot at an angle of 90° with a slight inversion outward. The arch of the foot is carefully modeled. To control the position of the reduced foot, an x-ray is taken in two projections. The leg is placed on a splint or pillow. If signs of impaired blood supply and increasing swelling of the foot appear, the plaster cast is immediately cut along its entire length, and the edges are slightly moved apart. After 3 weeks, the plaster cast is changed. The knee remains free. The foot is given a normal position. The plaster cast is removed 8 weeks after reduction and physiotherapeutic procedures and therapeutic exercises are prescribed.
Rice. 205. Dislocation in the subtalar joint. a - before reduction; b - after reduction.
If reduction of the dislocation fails, urgent surgical intervention is indicated. In some cases, when there is a fracture with significant damage to the articular surface of the head of the talus or scaphoid, arthrodesis of the talonavicular joint is indicated.
Other types of subtalar dislocations - external, posterior and anterior - are determined by the corresponding position of the foot. Depending on the type of dislocation, reduction is carried out in the direction opposite to the displacement of the foot.
Complete isolated dislocation of the talus
Dislocation occurs at the moment of strong inversion of the foot, adduction and plantar flexion. The external and internal ankle ligaments, tibiofibular and subtalar ligaments are torn. The talus is everted: its body, turned in the frontal direction, faces the outer malleolus, and its head faces the inner; the lower articular surface faces backward, and the upper one faces forward.
The vessels supplying the talus are often ruptured, as a result of which, even after reduction, avascular necrosis of the talus can develop.
Symptoms and recognition. The ankle joint is deformed. The soft tissues and skin are tense and sometimes torn. In these cases, a rotated talus is presented.
Treatment. Reduction under anesthesia should be attempted immediately. The patient is placed on the operating table. The knee is bent at a right angle. A counter-thrust is created behind the thigh using a sheet. The assistant applies a strong pull on the heel with one hand, and with the other hand, which is placed on the forefoot, performs strong plantar flexions and rotates it inward for several minutes in order to expand the space in the ankle joint. Traction can also be performed using skeletal traction on a screw traction apparatus. At this point, the surgeon presses firmly with his thumb on the back of the talus, which has rotated and faces the outer malleolus. Pressure is applied inward and backward. At the same time, you should strive to rotate the talus around the longitudinal axis. Then a plaster cast is applied from the middle of the thigh to the fingertips. The knee is fixed at an angle of 150°. After a control x-ray, the leg is placed on a splint or pillow. After 3 weeks, the plaster cast is removed and another one is applied - up to the knee - for another 6 weeks. Wearing the leg should not be allowed for another 3 months, as there is a risk of developing aseptic necrosis of the talus. If such signs are detected radiographically, weight bearing on the leg is not allowed until complete revascularization. This may take several more months. Unfortunately, it is not always possible to prevent this complication in this way. When reduction of a closed dislocation of the talus in the described way has failed, and also if, as a result of dislocation of the talus, the skin has burst and there is a wound, urgent surgery is indicated.
Isolated dislocations of the cuboid, scaphoid and sphenoid bones, as well as dislocations at the Chopart joint, are rare.
The diagnosis is established radiologically. An attempt to realign these bones in most cases does not lead to the desired result, so surgical intervention is indicated. It comes down to realigning these bones and fixing them with knitting needles or staples.
Dislocations in the Chopart joint
This joint, also called the middle tarsal joint, includes the talonavicular and calcaneocuboid joints. The articular spaces of the Shopard joint are similar in outline to the horizontal letter S. Strong and sharp abduction, less often adduction, rotational pressure on the forefoot can cause partial or
complete dislocation of this joint. Displacement in the chopard joint of the distal part of the foot in relation to the talus and calcaneus usually occurs internally and towards the rear. Dislocation is often combined with a fracture of the cuboid or scaphoid bone. Displacements of fragments are rarely significant.
Symptoms and recognition. The foot is significantly deformed. The skin is stretched. Swelling and severe pain quickly increase, making it impossible to step on the foot. The edge of the navicular bone can be felt on the inner and dorsal surfaces of the foot. There is a significant circulatory disorder in the foot.
An x-ray makes it possible to accurately depict the nature of the damage.
Treatment. Reduction under general anesthesia should be attempted immediately. In this case, fractures of the cuboid and scaphoid bones can be neglected and all attention can be focused on reducing the dislocation. One assistant supports the shin in its lower third, the second one stretches the heel with one hand, and the other covers the front of the foot and produces strong traction. The surgeon, using the elevations of the first finger, strongly presses on the forefoot in the inward direction, and with the other hand, placed on the inner surface of the heel, presses in the opposite direction - outward. He then places one hand on the back of the foot and the other on the sole and applies firm downward pressure towards the sole. After reduction, a plaster cast is applied to the knee. The foot is fixed at a right angle and the arch is well modeled. The leg is placed on a splint and the state of the blood supply to the foot is monitored. Walking is allowed after 2-3 days with the help of crutches without putting weight on the leg. The plaster cast is removed after 2 months. In the future, therapeutic exercises, massage, warm baths, and wearing an instep support are prescribed. At first, the patient walks with the help of crutches, lightly loading the leg, then the load is increased.
If reduction fails, urgent surgery is indicated. An incision on the dorsum of the foot, depending on the nature of the displacement, is made closer to the inner or outer edge. After exposing the Shopard joint, reduction is performed using the techniques described above. To prevent re-dislocation, one or two wires are inserted through the scaphoid into the head of the talus, the free ends of which remain above the surface of the skin. The wound is sutured and a plaster cast is applied. The needles are removed after 4 weeks. Further treatment is the same as described above. If there is significant destruction of the articular surfaces in the chopard joint, primary arthrodesis is indicated. Arthrodesis is also necessary when deforming arthrosis develops and pain continues for a long time (a year or more).
Rice. 206. Types of complete (a, b, c) and incomplete (d, e, f) fracture-dislocations in the Lisfranc joint.
a - dislocation of all metatarsal bones outward; b, c — divergent (divergent) dislocation; d — dislocation of the II-V metatarsal bones outward; e — isolated fracture-dislocation of the first metatarsal bone medially and plantarly; e - isolated dislocation of the fifth metatarsal bone outward and posteriorly.
Rice. 207. Divergent (divergent) dislocation in the Lisfranc joint. a - before surgery; b —
reduction and osteosynthesis with wires; c — after removing the spokes.
Diagnostic procedures
Although there are no clinically validated tests for diagnosing SBS, two clinical techniques have been described: the midtarsal adduction (midplane rotation) test and the midtarsal supination test. During the adduction test, the tarsal joint passively moves in the transverse plane (above/below the axis) while stabilizing the calcaneus. During this technique, the medial part of the calcaneocuboid joint is compressed and its lateral part is relaxed. Supination is a similar technique with the addition of inversion (frontal plane) and plantar flexion (sagittal plane). Pain can also be caused by passive dorsal or plantar movement of the cuboid. This movement is reduced when the cuboid is in a locked position. The diagnostic accuracy of these techniques has not been determined.
Dislocations in the Lisfranc joint
Dislocations of the metatarsal bones occur when you fall on your foot under the influence of a force acting on the front part of it, or if there is a forceful rotation of the foot. There are complete (all metatarsal bones) dislocations in the Lisfranc joint, which, as a rule, are combined with a fracture of one second metatarsal bone, and dislocations of individual metatarsal bones, which are also combined with fractures. Isolated dislocation is observed mainly of the first metatarsal bone. Dislocations of the metatarsal bones can occur upward, downward, outward, inward, and in different directions (divergent dislocation) (Fig. 206).
Symptoms and recognition. Patients feel severe pain and significant swelling is noted. The foot is deformed. There are often signs of a circulatory disorder in the foot. The diagnosis is confirmed by x-ray.
Treatment. Reduction should be undertaken immediately under general, less often under local anesthesia. Forced simultaneous traction is used on the distal part of the foot, and in case of isolated dislocation - on the finger of the same name; simultaneously exert pressure on the protruding bases of the metatarsal bones. Then, for 6-8 weeks, a bedding-free plaster cast is applied to the foot and lower leg. After removing the plaster cast, the patient must wear an instep support for 6-12 months. If reduction fails, surgery is indicated. After reduction, re-dislocations often occur. To prevent them, they should be fixed using 2-4 knitting needles, which are passed through the metatarsal bones into the cuboid and triangular bones (Fig. 207).
Differential diagnosis
- Fracture or dislocation of the cuboid bone, calcaneus, or 4th or 5th metatarsal bones.
- Calcaneonavicular fusion.
- Tendonitis of the fibula or extensor digitorum brevis.
- Plantar fasciitis.
- Sinus tarsus syndrome.
- Formation of the menisciform body in the ankle.
- Gout.
- Inflammation of the tarsal bones.
- Lisfranc joint injuries.
- Compressive neuropathy of the sural nerve.
- Entrapment of the lateral plantar nerve.
- Impingement syndrome of the ankle joint.