Cervical spinal stenosis is a process of reducing the lumen of the spinal canal due to the development of various pathological structures. As a rule, the tendency to form stenosis most often occurs in people over 55 years of age. In a quarter of cases of the disease, cervical vertebral stenosis is diagnosed. In the absence of timely measures taken, spinal stenosis causes disability and disability.
Types of cervical stenosis
This pathology is represented by the following groups.
- Congenital (primary) stenosis, when the disease develops as a result of congenital abnormalities in the structure of the spine.
- Degenerative , acquired or secondary stenosis of neck vessels is a consequence of destructive-degenerative acquired changes.
- Combined or mixed stenosis is determined in the presence of various causative development factors.
Based on the area of the lesion, a distinction is made between relative and absolute stenosis (area less than 75 mm² or more than 75 mm², respectively).
Lateral stenosis is defined as a narrowing of the intervertebral foramen to 0.4 cm or less.
The term sagittal stenosis refers to a narrowing of the canal in the same plane.
Anatomically, the following types of cervical spinal canal stenosis are distinguished:
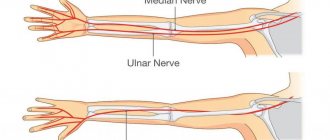
- lateral or lateral , when the exit site of the roots (radicular canal) of the spinal cord decreases in volume;
- central , when on the arch of the cervical vertebra (at the point where the roots exit) the distance from the posterior surface to the lateral surface decreases.
Complications of spinal canal stenosis
The main danger of primary stenosis is dysfunction of the respiratory system, which is observed against the background of compression of the spinal roots. Shallow breathing may be replaced by attacks of suffocation, which sometimes goes away on its own. But such situations are extremely dangerous for human life, so it is better not to take risks and immediately seek medical help.
Also, as a result of the narrowing of the canal, a change in the quality of nutrition of the spinal cord and brain is observed, since formations protruding into its lumen can compress the vertebral arteries, as well as other blood vessels. In such situations, surges in blood pressure may occur, which can lead to ischemic areas in the brain and stroke.
Other complications of such conditions include:
- brain hypoxia;
- massive swelling;
- poor circulation throughout the body;
- development of deviations in the functioning of internal organs;
- changes in the tissues surrounding the spinal canal.
Such complications do not pose such a threat to life as respiratory failure or ischemia of brain tissue, but they can significantly reduce a person’s quality of life and ultimately lead to extremely severe and sometimes fatal consequences. Therefore, it is important not to neglect the existing symptoms of the disease, but to immediately consult a doctor in order to diagnose the causes of their occurrence and prescribe treatment appropriate to the situation.
Why does cervical stenosis occur?
Cervical spinal stenosis develops for several reasons:
- Spinal fracture with compression of the vertebrae (compression);
- Congenital pathological changes in the structure of the vertebrae;
- Inflammatory diseases of the spine;
- Ankylosing spondylitis;
- Tumor processes;
- Intervertebral disc herniation;
- Chronic diseases of the articular surfaces of the spine;
- Adhesions after surgery;
- Overweight;
- Intervertebral disc displacement;
- Bone growths and osteophytes;
- Violation of the structure of the posterior yellow ligament;
- Osteochondrosis.
Stenosis of the neck vessels develops due to a decrease in the cavity where the spinal cord, nerves and vessels of the spine are located. First, complaints arise during certain turns and bends, then blood flow is disrupted and the situation worsens.
Over time, the pressure of the cerebrospinal fluid increases, provoking congestion and inflammatory processes.
Reasons for the development of pathology
Cervical stenosis can result from a huge number of diseases of the spine of this region, in particular:
- compression fracture of the spine;
- inflammatory diseases, including spondylitis;
- Bekhterev's disease;
- arthrosis of the facet joints with an increase in their size;
- formation of benign and malignant tumors, metastases;
- intervertebral hernia;
- deforming spondyloarthrosis;
- spondylolisthesis;
- spondylosis;
- pathologies of the posterior yellow ligament, accompanied by its thickening and compaction.
Sometimes cervical stenosis is a consequence of the formation of adhesions after surgery on the cervical spine.
Prerequisites for the development of the disease are created in the presence of:
- osteochondrosis;
- overweight;
- spinal curvatures.
In the vast majority of cases, cervical spinal stenosis occurs in people over 55 years of age.
Symptoms
The symptoms of absolute sagittal stenosis are determined by which structures are being compressed. The disease progresses slowly.
- Pain in the neck occurs - first in a certain position, gradually turning into permanent pain, which can radiate to the arms, shoulders, back of the head or shoulder blades.
- Feeling dizzy with sudden bends and turns, fainting is possible.
- Headaches in the temples and back of the head.
- The sensitivity of the scalp, arms and neck is impaired.
- You feel discomfort and weakness in your hands.
- The tone of the upper limbs and muscle frame increases.
- Changes in the functioning of the pelvic organs are observed: diarrhea alternates with constipation, fecal and urinary incontinence.
- Weakness in the legs.
- Breathing is labored, shallow, or rapid.
- Paralysis of limbs or complete immobility.
Diagnostic features
The doctor begins with a conversation with the patient, during which he finds out:
- complaints at the time of application;
- factors predisposing to the disease;
- previous diseases.
For the doctor, the body position that the patient is forced to take is important; he palpates the spine in order to determine the affected area.
The patient is prescribed additional examination:
- X-ray of the spine in two projections to determine bone growths, identify destroyed and fused vertebrae, disruption of the structure of joints, the presence of neoplasms, determine their size, location and structure;
- CT scan of the spine to find the cause of the disease, taking into account the smallest changes;
- MRI (if there are no contraindications) to detect changes in cartilage, nerves and blood vessels;
- myelogram to find changes in the structure of the spinal cord, the patency of the canal and the condition of the cerebrospinal fluid.
How is cervical artery stenosis treated?
Stenosis of the cervical arteries is treated using conservative methods (physiotherapeutic procedures and medications) and surgical intervention.
Conservative treatment
The course of treatment is selected for each patient, taking into account the characteristics of his condition:
- painkillers (NSAIDs) with analgesic and anti-inflammatory effects;
- injections of hormonal agents into the spine to reduce swelling, tissue compression and pain;
- diuretics to reduce cerebrospinal fluid pressure and relieve swelling;
- electrophoresis with novocaine to relieve pain in the affected area;
- magnetic therapy to reduce swelling and relieve pain;
- when the muscle frame is tense, massage is used;
- physical therapy – special exercises for stenosis help strengthen the cardiovascular system, arm and neck muscles;
- manual therapy;
- acupuncture;
- spinal traction.
Surgical treatment
Surgical methods are used if a conservative approach does not provide a lasting effect or the development of the disease calls into question the patient’s life and ability to work. Today there are many methods of surgical treatment, but three operations provide maximum effectiveness:
- decompressive laminectomy - an operation to remove a structure that causes a narrowing of the canal (hernial protrusions, tumors, intervertebral discs and arches, osteophytes;
- installation of stabilizing systems;
- installation of an implant after removal of the affected fragment.
Prevention of cervical stenosis
To prevent the development of the disease, preventive measures should be used:
- kneading the neck - eliminating physical inactivity;
- exercise therapy;
- correct posture, including while working at the computer;
- proper nutrition;
- if necessary, timely contact a specialist.
Feedback from patients suggests that when contacting a medical facility in the early stages, within 6-12 weeks, the pain syndrome disappears in most of them. In advanced cases, as a rule, cervical vertebral artery stenosis requires hospital treatment for a long time.
Cerebral circulation disorders in cervical osteochondrosis
Osteochondrosis is a degenerative-dystrophic disease of cartilage tissue that develops as a result of impaired metabolism of glycosaminoglycans. It can begin in almost any articular joint of the body, but most often it affects the intervertebral discs of the most mobile segments of the spinal column - the cervical and lumbar.
Since the intervertebral joints do not contain blood vessels, their nutrition and water supply occurs in a diffuse manner (by exchange with nearby soft tissues). With age, metabolic processes in the body slow down significantly or are disrupted, which leads to gradual dehydration and destruction of cartilage fibers, and, consequently, subsidence and thinning of the intervertebral discs.
Deformed joints are no longer able to fully perform their shock-absorbing functions, and with certain physical activities, pinching of nerve roots and blood vessels, pain, limited mobility and other complications occur. For the cervical spine these are headaches, dizziness, cerebrovascular accidents, hearing and vision disorders, etc.
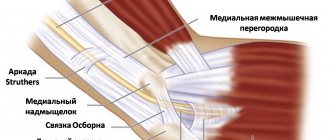
Pathogenesis of the disease
Chronic pain syndrome, inflammation, spasms and discomfort when moving the head cause a response from the body, as a result of which growths of bone marginal plates (osteophytes) are formed. With sudden physical exertion or awkward movements, intervertebral hernias or protrusions may occur, when the dense shell of the disc cracks, releasing a gelatinous substance (nucleus pulposus). Quite often, it is osteophytes or hernial protrusions that compress the spinal blood vessels or nerve endings.
The cervical segment of the spine is designed in such a way that almost all the vital highways of the body that feed the brain lie in it, but it is supported and protected only by a very thin muscular corset.
As a rule, vascular pathologies are based on two main factors: compression of the vertebral or basilar arteries, as well as damage to the vasomotor (vasomotor) center located in the medulla oblongata. It is damage to the latter that causes dysfunction of the innervation of all smooth muscles of blood vessels (including the spinal cord and brain), which is fraught with sudden changes in blood pressure, hypoxia, ischemia, stroke, etc.
A decrease in the tone of the blood vessels of the brain, as well as the whole body, causes thickening of their walls or stenosis of the lumen of the canal, which can provoke disturbances in blood microcirculation, and, consequently, a slowdown in metabolic processes. In some cases, restoration or compensation of blood circulation occurs due to developed networks of collaterals, but they are not always durable.
Stages of disease development
The development of circulatory disorders in the system of vertebrobasilar arteries in osteochondrosis of the cervical spine can be conditionally divided into the following stages:
- Initial or stage of development of dyscirculatory encephalopathy (slowly progressive and/or diffuse damage to blood vessels, small arteries and arterioles of the brain). The patient is worried about dizziness, headaches, decreased attention and memory, difficulty maintaining balance, sleep disorders, fatigue, dysfunction of the organs of vision and hearing. There is a loss of cognitive, spastic, vestibular and autonomic functions.
- Subcompensation or the stage of pronounced neurological disorders, when the symptoms of the disease gradually increase and the patient’s well-being worsens. This is expressed in disorders of thinking and the ability to control subtle sequential movements, slower speech and chewing, deepening of the voice, constant changes in blood pressure, apathy, emotionally depressed state, etc.
- Late stage (decompensation) or stage of development of irreversible disorders in the central nervous system. At this stage, the patient practically becomes disabled, as he loses the ability to care for himself. He develops vascular dementia (dementia), affective disorders, parkinsonism, hypokinesia, involuntary laughter or crying, and quite often there is no ability to control urination and defecation.
Diagnosis and treatment of circulatory disorders in cervical osteochondrosis
A preliminary diagnosis is made during the initial examination of the patient by a neurologist and after collecting the clinical picture. The level of damage to the intervertebral discs is determined after an X-ray of the spinal column. Compression or damage to blood vessels, vascular beds, and nerve endings can be seen on an MRI or CT scan.
Pathologies of the spinal cord or brain are diagnosed using myelography with the introduction of a contrast agent. Dopplerography and ultrasound examination of cerebral vessels makes it possible to determine the patency of the channels and the speed of passage of blood fluid through them.
Treatment of cerebral circulatory disorders with cervical osteochondrosis depends on the location of the pathology, the severity of the lesion and the causes of the disease. First of all, conservative therapy is aimed at improving the patient’s condition (restoring and improving metabolic processes in the body and activating the regeneration processes of damaged cartilage tissue). For these purposes, the following are used: exercise therapy, massage sessions and physiotherapeutic procedures, adequate physical activity, and various water procedures.
Surgical methods of treatment are used quite rarely and only in cases where the patient’s condition sharply worsens or there is a threat to the normal functioning of internal organs.
Special drug therapy, in addition to drugs that relieve pain, muscle spasms, inflammation and swelling of soft tissues in the treatment of classic osteochondrosis, consists of:
- vasoactive drugs that activate cerebral circulation and dilate blood vessels;
- neuroleptics and antidepressants that have a sedative, calming effect, reducing the degree of cognitive (dizziness, vomiting, sweating, etc.) manifestations;
- nootropic agents that improve metabolic processes in the brain, memory, perception, thinking, speech abilities;
- diuretics and antioxidants, which help reduce swelling and activate the body's regeneration processes;
- B vitamins, calcium supplements or other vitamin complexes that improve the condition of the central nervous system and the patient’s entire body.
At home, the patient is advised to reconsider his lifestyle, give up bad habits, devote more time to active recreation and activities, and try to control his weight.
It is advisable to do morning exercises every day, water procedures, special physical exercises, attend sports clubs or take daily long walks at a fast pace.
Follow a daily routine, alternating appropriate periods of stress and relaxation, eat properly and rationally. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr