What is hygroma and what causes it?
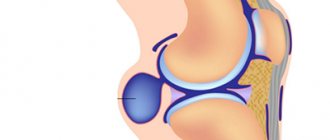
Any hygroma is a benign neoplasm that is not life-threatening. It does not degenerate into a cancerous tumor or other types of malignant formations; its only danger is the possibility of developing secondary inflammation, which, in turn, will cause pain and limited mobility. A hygroma is essentially a fluid-filled cyst that has a clear shell and is localized near the joint. The neoplasm is formed from the articular membranes and has a pedicle with which it is attached to the articular capsule, which explains its stable position.
Where is it located?
Hygroma of the foot occurs on the instep, in the area of the heel bone or ankle, depending on which joint it grew from. The most unpleasant location is the sole: such cysts especially interfere with walking and cause severe discomfort.
Why does it appear?
The reasons for the appearance of this neoplasm are still not fully understood. It is known that hygroma is more often formed in women than in men (sometimes several times), and also that this disease affects mainly young people, from 20 to 30 years old. It very rarely occurs in children and the elderly; after forty, its formation is considered rather an exception.
Provoking factors.
These reasons are considered:
- hereditary predisposition. In families where older relatives have had cases of synovial neoplasms, they are likely to appear in the younger generation. It is believed that this is due to the characteristics of tissues that are inherited;
- intensive work of joints. The risk of developing a cyst is higher if a person actively loads a particular joint. In the case of hygroma of the foot, those at risk include hikers, athletes whose activities involve footwork, or representatives of professions that involve walking or standing in one place for long periods of time. Hygroma can be caused by wearing heels, uncomfortable, too tight shoes;
- injuries and illnesses. Suffered joint injuries can lead to the appearance of a synovial cyst; tendonitis, synovitis, bursitis and other inflammatory diseases of the joint and surrounding tissues are also considered risk factors.
Characteristics of the pathology
A tumor of dense consistency from the connective epithelium of a round shape may form on the leg in the ankle area. The capsule contains inside a viscous liquid of a transparent or yellowish tint. When pressed with your fingers, a jelly-like compaction is felt. Hygroma is attached to the outer sheath of the tendon or directly affects the joint. Hygroma of the ankle joint ranks second in the frequency of diagnosed cases after tumors of the hand.
The cyst is usually located on the back of the foot or sole, and can be diagnosed in the instep area, on the toe of the left or right foot. The tendon process of degeneration into dystrophic-degenerative disorders leads to the formation of a neoplasm on the articular membrane.
Two types of cells are involved in the formation of a cyst:
- fusiform form the outer capsule of the hygroma;
- spherical ones produce a viscous liquid that fills the capsule.
If the capsule is not completely removed, the pathology is prone to relapse, so doctors try to remove the capsule along with its contents.
Hygroma can present as a single formation on the right or left foot, as well as in the form of multiple lumps on both legs at once.
The ICD-10 code for the disease is M71.3 “Other cyst of the bursa.” The nature of the disease is benign, but it needs to be treated at any stage of development. Large sizes put pressure on neighboring tissues: they are subject to mechanical injury when putting on shoes or walking.
How to detect hygroma
First signs
Secondary symptoms usually do not appear immediately. In the early stages, hygroma looks like a nodule or ball under the skin, soft, but nevertheless dense, with clearly defined boundaries. The shape of the neoplasm is usually regular, close to spherical, there is no sensation of germination into other tissues, or blurring of the boundaries. The seal can move freely, but with a very small amplitude. Inside the hygroma is synovial fluid, a substance that is usually found in the joint, sometimes interspersed with mucus or fibrin.
Development of the disease
If at first a hygroma is just a lump that is not painful in itself and does not cause discomfort, then over time secondary symptoms appear. It is associated with the growth of the tumor, which can be quite rapid: synovial cysts can reach impressive sizes. Secondary symptoms are associated with the fact that the hygroma begins to compress the surrounding tissues, pinching them and thereby interfering with their normal functioning.
Secondary signs
These include:
- pain that manifests itself when pressing on the hygroma or when trying to move the affected joint;
- discomfort when moving (especially pronounced in the case of hygroma on the foot in places that experience stress while walking);
- redness, swelling, other symptoms of inflammation resulting from tissue compression;
- blood stagnation, which is accompanied by numbness, a tingling sensation, and a change in the temperature of the foot.
The color of the skin over the hygroma is no different from normal; in some cases, the skin becomes rougher and rougher than before the cyst appeared. The tumor can grow for several years, remaining unnoticed until it begins to cause discomfort, or it can rapidly develop in a short time - up to several days.
Important
A swelling found on the foot is not always a hygroma. The lump can be a symptom of other diseases, so you should not diagnose yourself. It is best to consult a competent doctor and find out for sure what kind of disease manifests itself this way.
Why the disease is unpleasant
Hygroma has no risk of malignancy and, as a rule, is not capable of causing death. Often a person does not notice it at all until it grows to a state in which it becomes visible to the naked eye. The cyst begins to cause discomfort when it grows to a certain size: as a rule, doctors talk about a diameter of over 10 mm. Much depends on its location: the most unpleasant are hygromas on the sole of the foot; neoplasms on the instep, heel or ankle are not so uncomfortable, but can cause problems when choosing shoes, walking, or changing shoes. If the cyst begins to compress the surrounding surfaces, secondary aseptic inflammation may occur, which is characterized by pain and limited mobility.
What will happen if left untreated?
Depending on the specific case, hygroma on the foot can behave very differently without treatment. Sometimes growth stops at a certain point; in some situations, the tumor continues to grow until it reaches a substantial size. The rate of growth also varies from person to person, with the development of a synovial cyst taking anywhere from a matter of days to several years. You can predict something only after reading a specific case, but there are certain observations that apply to all patients:
- Overloading the joint increases the likelihood of hygroma growth, so it is recommended to reduce physical activity during treatment;
- physiotherapeutic and drug treatment affects concomitant inflammation and other secondary symptoms, but does not in any way reduce the size of the tumor and is not able to influence its development;
- It is extremely rare for hygroma to resolve on its own, but this happens infrequently, and you should not count on such a possibility.
Classification
Hygroma of the foot is classified according to structural features. There are two forms in total:
- Single-chamber. Usually located on the thumb joint;
- Multi-chamber. Most often localized on the soles or in the ankle area.
In addition, foot hygroma can be:
- isolated, not connected to the synovial bursa;
- with anastomosis;
- with valve.
In the latter case, the synovium penetrates into the hygroma cavity only during physical activity.
Accidental hygroma injuries
If a synovial cyst is damaged, it can burst and quickly disappear, but it is highly not recommended to injure it yourself in the hope of such a possibility. In this way, the surrounding healthy tissue can be damaged, in addition, the contents of the cyst will remain around the joint and in the future will lead to the formation of new hygromas. Crushing the tumor often causes relapses, including multiple ones, in which several hygromas form at once near one joint. External damage that disrupts the integrity of the skin (for example, puncture) can lead to infection and the development of a secondary infectious process with the formation of pus. In the case of a synovial cyst of the foot, the risk of injury is much higher than in other cases, so it is not recommended to delay contacting a doctor.
We fight hygroma with folk remedies
Conservative medicine offers hope for a chance to avoid unwanted surgical interventions when treating a tumor. There is no guarantee that folk remedies for combating hygroma will be more effective than traditional medicine. If the disease is already advanced, home recipes will not help and you cannot do without a doctor. Folk remedies are based on plants and natural products. Here are the most common ones.
"Copper" miracle
A copper coin is applied to the tumor and tied tightly with bandages. You need to wear the “copper” bandage for two to three days. Patients who have experienced this method on themselves confirm its effectiveness.
Compresses
Lotions are made from raw eggs and wine vinegar.
A compress of 60% alcohol is also used at night. Gauze cloth soaked in the solution is applied to the tumor, and a layer of cotton wool and polyethylene is placed on top. The compress is fixed with a bandage.
Physalis (cranberry) will help
Crushed cranberry fruits are applied to the neoplasm in the form of a compress.
Ointment "folk"
Powder from 30 analgin tablets is mixed well with 200 g of iodine. The ointment is used until the tumor disappears. When using this method, you need to follow safety precautions. The mixture may cause allergies or “corrode” the skin. Be careful with folk remedies.
Diagnostics
The importance of visiting a doctor
Diagnosis and treatment of hygroma of the instep and other areas of the foot begin with a visit to a specialist. A traumatologist and rheumatologist deal with cysts near the joints: these doctors are the first ones to start examining if you suspect a hygroma. Despite the fact that the neoplasm is diagnosed quite easily and is usually visible to the naked eye or manifested by palpation, the doctor’s goal is to exclude other diseases. Such symptoms are caused not only by hygroma: the cause may be an epithelial cyst, lipoma, vascular formation and other types of benign tumors. Also, swelling and growths near the joints are a common symptom of arthritis and other inflammatory diseases of the musculoskeletal system.
Diagnostic methods
To make an accurate diagnosis, the doctor usually prescribes:
- general and biochemical blood test, urine test (they are needed to accurately exclude diseases that one way or another cause changes in the composition of urine and blood);
- Ultrasound or radiography (allows you to see what is happening under the skin and inside the joint).
Often these measures are enough to make an accurate diagnosis, but if doubts remain, a specialist may recommend a puncture or MRI. Conversely, in cases where the diagnosis is clear without additional measures, the doctor can report hygroma immediately after visual examination, palpation and history taking.
Treatment
For foot hygroma, conservative or surgical treatment is used. It is important to understand that the tumor will not disappear or decrease by taking medications and undergoing physiotherapeutic procedures: they are needed to relieve inflammation and increase joint mobility, but none of these measures will get rid of the cyst itself. There is no evidence that any medications or procedures can shrink or eliminate a hygroma - only surgery is used for this.
Medication measures
Nonsteroidal anti-inflammatory drugs and, in rare cases, glucocorticosteroids are used as medications. They are designed to reduce swelling around the cyst, relieve secondary inflammation that occurs due to compression or concomitant diseases of the musculoskeletal system. Antihistamines are sometimes added to anti-inflammatory drugs. If an infection has been introduced into the hygroma (this happens if you try to puncture the cyst yourself), the doctor prescribes antibiotics that should overcome the infectious process.
Physiotherapeutic measures
They are selected based on the specific case and may include mud therapy, ultrasound or shock resonance therapy, paraffin therapy and other methods. Some evidence suggests that these treatments may shrink a hygroma, but this does not always happen, and even when this happens, the risk of the tumor growing again is extremely high.
Surgical treatment
This is the only method that today allows you to completely get rid of a synovial cyst. In the past, crushing was used as a therapeutic measure, but today it is not used due to the very high likelihood of relapse and the possibility of damaging surrounding tissue. Surgery for hygroma is easy and does not require general anesthesia or a long hospital stay. It is usually prescribed if the cyst is growing rapidly, causing discomfort or pain in the patient, or interfering with his normal life activities - in other cases, the operation is performed only at the request of the person himself.
How it goes
Under local anesthesia, a skin incision is made, after which the surgeon performs resection of the cyst. Usually it is removed directly in the capsule; damage to the walls of the hygroma is not allowed. The wound is sutured, it is treated with antiseptic drugs, after which the patient can go home. For a certain period of time, you must follow the recommendations (do not disturb the limb, treat the incision site), and then come back to remove the sutures.
Modern method
This is an operation using a laser that burns out the cyst. Its use is justified if the hygroma is located near blood vessels or nerve endings that can be damaged during standard surgery. After laser surgery, tissue recovers faster.
Recovery after surgery
After surgery, a special rubber band is inserted into the wound and a suture is applied. The elastic band is removed and the stitch is removed seven days after surgery. To avoid the formation of adhesions, special exercises are prescribed. Recovery is important, as is surgery. Proper return to form minimizes the risk of disease recurrence. This process takes up to three weeks. Bandages or plaster splints are used for healing. This period is accompanied by aching pain, the leg swells, and the skin peels.
Without indications for removal, it is permissible not to get rid of the hygroma and live with it all your life. The patient decides to leave the lump or remove it for aesthetic purposes.