Healthy and strong joints of the lower extremities are the key to active longevity and the ability to engage in active sports. However, precautions should be taken. At least in order not to wonder why a lump appeared under the knee at the back, what it is and which doctor should be consulted for treatment.
For what reasons a lump may form at the back of the knee, we will examine it in detail in this material. You can learn about those diseases that manifest themselves with similar symptoms and the possibilities of treating them using manual therapy techniques.
It is important to understand that any neoplasms, regardless of their location, require close attention from medical personnel. A lump on the leg behind the knee may be the result of a deformed blood vessel (vein or artery), a blood clot, an inflamed lymph node, etc. Wen, hygroma and dermoid cysts are often localized here. These pathologies are surgical in nature and are benign neoplasms. You will not be able to determine on your own what kind of lump has formed. Therefore, we suggest that you seek medical help in a timely manner to make an accurate diagnosis.
If you have a lump on your leg under the back of your knee after a domestic or sports injury, knee sprain, twisted ankle or bruise, you can sign up for a free initial consultation at our manual therapy clinic. We provide rehabilitation after various injuries. We have developed special proprietary programs that allow us to restore the integrity of the ligamentous, tendon and muscle apparatus, internal synovial bursae and cartilaginous tissues of the joint.
Baker's cyst
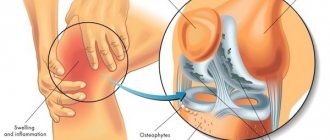
Baker's cyst is a hernial protrusion of the mucous bursa (bursa), which is located in the popliteal fossa, between the tendons (posteriorly) and connects to the joint capsule. The cause of the formation of Baker's cyst is trauma, post-traumatic changes and cystic degeneration of the menisci, rheumatoid arthritis and other diseases.
Baker's cyst. Click on photo to enlarge
A lump is the result of an inflammatory process, due to which the synovium of the joint begins to produce more fluid. Under pressure (during movement and load), it enters the popliteal intertendon bursa and fills it.
Main symptoms:
- the swelling can have different shapes (grape bunch, crescent, with a constriction in the middle, which makes it seem like there are 2 cysts under the knee, etc.);
- a small cyst does not affect the function of the joint, in this case the disease is asymptomatic;
- a large lump causes sharp, compressive, but more often aching pain in the knee, which intensifies with pressure, with extension, and can radiate to the lower leg and thigh.
Prognosis: with timely treatment, Baker's cyst is completely cured (in 90% of cases, half of them by conservative methods). Rarely (in 10% of cases) a large hernia:
- Causes compression of nerves, blood vessels, muscles and can lead to their necrosis (tissue death).
- It can rupture and cause swelling of the tissues of the lower leg.
- Causes thrombophlebitis (inflammation of vascular walls).
What kind of bumps appear under the knees?
We decided that we need to talk about the main pathology that causes such complaints in more detail.
Becker's cyst - this term refers to the accumulation of inflammatory fluid (not pus) in the mucous bursa located on the back of the lower leg, just below the popliteal fossa. In 50% of people, this bursa is located between the tendons of the muscles (gastrocnemius and semimembranosus), it communicates with the knee joint through small holes and is a variant of the normal development of the joint.
If a long-term inflammatory process occurs in the knee joint, the fluid that is formed as a result accumulates in this intertendinous bursa and acquires the name of this disease. Physically, a cyst is a swelling on the back of the knee. When inflammation occurs, fluid accumulates in the knee, which can seep into this “bag,” thereby increasing its size. Most often, the disease develops due to metabolic-dystrophic or inflammatory processes that occur in the knee joint. Becker's cyst is caused by pathologies such as osteoarthritis, arthrosis, rheumatoid arthritis, but other options are also possible. In addition, there are complex Baker cysts - fused (synechia), with septa inside (septa), with small daughter cysts inside the main one.
The main causes of the development of Becker cyst:
Excessive physical activity.
Pathological changes in the menisci.
Inflammatory processes in the knee joint.
Mechanical damage to the knee.
Problems with cartilage, their gradual destruction.
Regardless of what exactly caused the pathological process to start, this will cause increased production of synovial fluid, which fills the tendon bursa, which is why a cyst is formed. According to statistics, this disease most often occurs in older people, athletes, and loaders, but it can also occur in children.
A small cyst of the knee joint, as a rule, does not manifest itself; the disease proceeds without obvious signs. The skin over the neoplasm is not hyperemic, not hot, its structure does not change. This indicates the absence of inflammation above the cyst. Visually - a small cystic formation protruding under the knee; there is no pain when palpated. During physical activity, minor pain may occur. At the same time, the cyst is mobile and changeable, and may disappear without treatment.
At the beginning of the development of Baker's cyst, the patient begins to feel only some discomfort in the knee joint, but if it continues to increase, characteristic signs of the disease appear:
️Pronounced, mobile tumor with clear edges under the knee; ️
Painful sensations on palpation;
️Constant aching pain in the knee joint; ️
As the cyst enlarges, the pain spreads to the muscles of the lower leg, intensifies under the influence of loads, and can radiate to the thigh or lower leg.
️A feeling of fullness and discomfort from a foreign formation appears and increases, associated with its growth. ️ During movement and loads, stiffness appears in the joint;
️The mobility of the knee joint is significantly reduced, numbness of the limb develops; ️
Swelling of the entire organ of movement is noted; ️
It becomes problematic to bend the knee, difficult to climb stairs and squats, and the pain intensifies; ️The onset of complete immobility of the knee joint is possible.
Diagnosis of Becker's cyst
An examination by a specialist will reveal changes characteristic of this pathology.
X-ray examination, unfortunately, cannot detect a cyst, so...
The main, most accessible method is ultrasound diagnostics of the joint and/or soft tissues of the joint. It allows you to clarify the size and structure of the cyst.
The cyst can also be detected by MRI of the knee joints. ️
The course and treatment of the disease can be lengthy. In this case, swelling of the knee and lower leg, redness under the knee and in the calf muscles, acute pain in the joint, and increased body temperature are observed. The enlarging cyst puts pressure on the veins of the leg, in which stagnation develops and the walls of the vessels become inflamed.
With very large cysts, thrombophlebitis, varicose veins and thrombosis may occur (we will present you a separate article about the risk of complications of which). Compression of the lymphatic vessels leads to swelling of the limb. Pressure on the nerves causes numbness in the leg.
Metabolic processes may also be disrupted, which provoke the development of necrosis and trophic ulcers. Suppuration of the cyst can cause inflammation of the joint - arthritis.
The disease begins to be treated after diagnosis, taking into account the general health of the patient, the presence of chronic diseases, age, lifestyle, and profession. It is aimed, first of all, at eliminating the cause that caused the appearance of this pathology.
The patient is advised to rest and avoid putting stress on the affected leg. Pain and swelling are reduced by applying cold to the knee periodically for up to two days. But this is a temporary effect. Fixing the organ of movement with an elastic or simple bandage helps reduce swelling. The bandage should be tight, but not impair the blood supply, which can aggravate the disease. In this case, the leg should be in an elevated state, which helps improve blood flow and reduce swelling.
If there is no need for hospital treatment, the doctor may prescribe anti-inflammatory drugs with an analgesic effect - non-steroidal drugs (ibuprofen, nimesulide, paracetamol or others). You can use NSAIDs and local ones, in the form of ointments. But it must be remembered that the use of ointment is only an additional method of treatment. Their correct use and compliance with dosages is also important. An increase in temperature with a Baker's cyst usually causes suppuration, its rupture, or an exacerbation of the underlying disease. In this case, non-steroidal anti-inflammatory drugs are used and antibiotics may be added to treatment. Etiotropic treatment is also determined and prescribed, which is aimed at suppressing the causes that caused the pathological process.
If the formation of Baker's cyst is associated with autoimmune connective tissue diseases - rheumatoid arthritis, lupus erythematosus, then treatment includes corticosteroid hormonal drugs (Dexamethasone, Prednisolone, Hydrocortisone). The medications stop the effects of the patient's immune system cells on the body's connective tissue cells.
In the presence of psoriatic arthritis, corticosteroids are prescribed, antihistamines are prescribed to relieve itching, and immunomodulatory drugs are prescribed to improve the functioning of the immune system. To reduce the amount of formation and accelerate the removal from the body of uric acid, which causes inflammation and promotes the production of joint fluid, allopurinol, etc. is prescribed for gouty arthritis.
If the cyst is diagnosed to be caused by osteoarthritis, the doctor may use a method of injecting corticosteroid drugs into the cavity of the cyst. This relieves inflammation and swelling in the area of the tumor well. Often, specialists decide to treat a cyst using drainage. Using a thick needle, they penetrate into its cavity, and use a large syringe to suck out the liquid contents. After this, hormonal anti-inflammatory drugs are administered. The procedure can be repeated. Its positive effect comes quickly. Pain goes away, swelling decreases, motor functions of the joint are restored.
Modern physiotherapeutic methods are also used in conservative treatment.
If medications and additional methods do not give a positive result, a relapse of the disease is observed, the cyst reaches a large size, the disease continues to develop, symptoms of complications appear, and surgical treatment is resorted to. During surgery, the pathological formation is dissected and removed. A modern method of surgical treatment of cysts using an arthroscope through two point incisions on the knee. This is an operation with minimal trauma and the possibility of wound infection. ️
Be healthy, but don't forget about disease prevention!
Prepatellar bursitis
Inflammation of the synovial bursa located on the front surface of the knee joint, in front of the patella. The reason is stress, mechanical injuries (impacts, bruises), chronic diseases (arthritis, arthrosis).
Prepatellar bursitis. Click on photo to enlarge
A bump with bursitis is the result of aseptic or septic (infectious) inflammation, which causes exudate (liquid) to accumulate in the bursa cavity.
Aseptic bursitis most often does not complicate the patient’s life - the bump in front under the knee is usually small, painless, can increase after physical activity, and occasionally causes discomfort and discomfort when bending the knee.
Purulent bursitis is characterized by:
- sharp, twitching pain in the bursa area;
- swelling, swelling and redness of the joint;
- pain when bending and straightening the knee;
- temperature increase;
- signs of intoxication (weakness, sweating, lack of appetite).
Prognosis: with timely treatment (the sooner the better), prepatellar bursitis is completely cured in 90–95% of cases. An infection can cause dangerous complications:
- breakthrough of pus into the joint cavity (purulent arthritis);
- into adjacent tissues (abscess, phlegmon);
- general infection (sepsis).
Inflammation of the tibial nerve
Inflammation of the tibial nerve (neuropathy) in the area of the popliteal fossa (runs from top to bottom, closer to the inner surface of the knee). The cause of inflammation is stress, injury, metabolic disorders, nerve compression, inflammatory processes in the joint and periarticular tissues.
Nerves and vessels of the popliteal fossa
A lump under the knee joint with damage to the tibial nerve is a strong swelling of the adjacent tissues; outwardly it resembles an elastic, dense and elastic bulge, painful when pressed.
In addition to the bump, the patient appears:
- Sharp, burning pain along the tibial nerve (from the popliteal fossa down to the foot).
- Loss of sensitivity in the back of the leg, sole of the foot, and fingers.
- The muscles of the leg and foot quickly atrophy (lose strength and volume), a person with tibial nerve neuropathy cannot stand on his toes and rests on his heel when walking.
Prognosis: success depends on how well the pathology that caused the neuropathy and lump under the knee can be treated - if it can be cured, the prognosis for recovery is good (in 70% of cases). If the development of neuropathy is based on genetic diseases, it is incurable, leading to dysfunction of the limb and loss of ability to work.
Pain under the kneecap
For orthopedists, the topic of pain in the anterior knee joint ends with heated debate around the treatment of certain problems that cause this pain .
What are the primary symptoms with which a patient comes for a consultation with an orthopedic traumatologist?
The patient's main complaint is PAIN , but depending on the disease causing this pain, it varies greatly. Typically, pain occurs:
- during physical activity (usually running, training in the gym, and especially squats and other sports)
- with a long flexion position of the knee joint (while driving a car or during constant sedentary work)
- under other factors (for example, when walking up the stairs)
The patient’s main complaint has been dealt with, but why does this pain in the knee joint occur in the first place? In fact, there are a lot of , and I tried to collect in a short list the most common diseases that I treat in my practice:
- Chondromalacia of the patellar cartilage is damage to the cartilage of the patella caused either by trauma or abnormal biomechanics of the movement of the patella.
- Osteoarthritis of the patellofemoral joint is a condition in which not only the cartilage of the patella is damaged, but also the area of cartilage on the thigh with which it comes into contact.
- Instability or damage to the ligaments - when the ligaments of the knee joint are torn or damaged, instability or excessive mobility occurs, which can cause pain.
- Pinching between the patella and femur of the synovial folds - normally we all have folds inside the knee joint. But due to individual development, in some people they can be greatly increased in size and fall between the patella and thigh, mechanically rubbing and damaging the cartilage.
- Various changes in the musculoskeletal system leading to dysfunction . Lack of tone and proper muscle function (for example, the rectus femoris muscle, which covers the entire patella with its tendon), incorrect biomechanical movement of bone structures occurs, which leads to overload of the cartilage.
- deformities that lead to changes in the axis of the lower limb. Any changes in the axis of the limb also lead to overload of certain parts of the joint, depending on the deformation (not all people have straight and beautiful legs).
What should you do if you experience such pain?
First of all, consultation with an orthopedic traumatologist is necessary. And then the treatment tactics depend on the diagnosis.
Most often this is conservative treatment in the form of injections of platelet-rich plasma or other types of modern cellular technologies; kinesiotherapy; various physical procedures (for example, shock wave therapy ), as well as exercises to strengthen the thigh muscles. You can read more about these treatment methods on my channel .
But of course, there are clinical situations where conservative treatment is impossible or has proven ineffective . In this case, minor surgery ( joint arthroscopy ) is required, for example to remove cartilage defects or folds from the joint.
Don’t forget, each patient needs an individual approach to treatment!
Popliteal artery aneurysm
A popliteal artery aneurysm is a protrusion of the wall of a blood vessel in the area of the popliteal fossa.
Different types of popliteal artery aneurysms. Click on photo to enlarge
Why does swelling appear with an aneurysm? An elastic, small lump in the popliteal fossa occurs due to the fact that the walls of the popliteal artery lose elasticity and strength, stratify and stretch, increasing the lumen of the vessel by 2 times. When you press on the lump under the knee from behind, you can clearly feel the pulsation (rhythmic beats of the heart and blood through the vessels, this distinguishes the formation from other lumps).
Reasons for appearance:
- congenital weakness of the vascular walls;
- loads;
- hypertension;
- atherosclerosis (plaques on the walls of blood vessels);
- infections of adjacent tissues;
- vasculitis (inflammation of blood vessels).
Another symptom of an aneurysm is acute, gradually subsiding pain in the popliteal fossa.
As the pain subsides, the following appear:
- pale or cyanotic (blue) skin;
- loss of sensitivity, numbness of the limb below the knee;
- weakness of the lower leg muscles.
In the popliteal fossa there may be not one, but 2 bumps (one above the other).
Prognosis: with an aneurysm of the popliteal artery, there is a high probability of thrombosis (blockage of the vessel, from 25 to 50%), which quickly leads to necrosis (death of soft tissue). The larger the size of the lump under the knee, the higher the risk of adverse complications (rupture of an aneurysm or blockage of a vessel). Early diagnosis and surgical treatment gives a chance of getting rid of the aneurysm (in 80% of cases).
Why did a lump form on the back of my knee?
A lump under the knee at the back may be a consequence of pathologies of the musculoskeletal system. Without timely assistance, serious complications may develop. Let's look at some common reasons why a lump may form on the back of the knee:
- bursitis (inflammation of the synovial bursa);
- pathology of the meniscus in the posterior part (may be associated with chondropathy and chondromalacia of a traumatic nature);
- cicatricial changes in ligaments and tendons at muscle attachment points;
- Baker's cyst;
- Hoff's disease.
If a lump has formed at the back of the knee, then it is necessary to conduct an examination and exclude all possible causes. A preliminary diagnosis can be made during the initial examination. Thus, with Hoffa's disease, during palpation you can hear the sound of distinct crepitus at the attachment points of the lateral ligaments. Pain syndrome occurs when trying to forcefully extend the leg at the knee joint. The area where the lump has formed at the back of the knee is usually swollen. Fluid may gradually accumulate inside the joint. Without timely and correct treatment of Hoffa's disease, the patient inevitably receives persistent contracture of the knee joint. Any movements in it will be limited.
Baker's cyst, like Hoff's disease, limits the mobility of the leg and occurs mainly due to traumatic exposure. The initial accumulation of fluid, forming a lump, occurs due to slight bleeding, which occurs, for example, with a small rupture of the ligaments. Then the accumulated blood undergoes decay and destruction. An inflammatory reaction occurs, during which fibrin is formed in large quantities in the resulting cavity. This substance is the basis of connective tissue, which in the form of scars replaces normal structures after injuries to ligaments, tendons, muscles and epidermis.
In order to prevent scar tissue degeneration, it is necessary to carry out proper and effective rehabilitation after any serious injury. If you have suffered a knee sprain, then immediately after the pain has been eliminated, you should begin rehabilitation measures under the guidance of an experienced specialist. The program includes osteopathy and reflexology, massage and gymnastics.
Other causes of lumps
A lump on the knee may appear due to other pathologies.
Osgood–Schlatter osteochondropathy
This is the death of the tibial tuberosity at the site of attachment of the patellar ligament. A lump with Schlatter's disease forms under the knee in front; it is quite dense and painful to the touch.
Osgood–Schlatter osteochondropathy
The reason for its appearance is excessive stress on the knees during the period of growth and formation of bone tissue in a child (this type of osteochondropathy is diagnosed only in children, adolescents and young adults from 10 to 18 years).
Abscess
This is an infectious inflammation of soft tissues (muscles or subcutaneous fat in the knee joint), as a result of which a cavity filled with pus is formed in them. The reason is the penetration of infectious pathogens (streptococci, staphylococci and others) through a wound or through blood vessels. An abscess lump can be located above or below the knee; it is painful, red, hot to the touch, quickly increases in size, and when pressed, you can feel the fluid inside oscillating. Local symptoms are accompanied by an increase in general temperature, weakness, sweating and other signs of intoxication.
Abscess
Synovioma
Synovioma is a malignant tumor that affects the synovial membranes, tendon and mucous membranes of the joints. The cause of cell degeneration is unknown. The lump is dense and lobed to the touch (heterogeneous, consists of several parts, fragments), without obvious boundaries, painful when pressed, of different sizes (from 2 to 20 cm), can be located under the knee or on the lateral surface of the joint. Over time it increases, capturing and destroying bones.
Tomogram shows synovial sarcoma (malignant synovioma) of the knee joint. Click on photo to enlarge
Diagnostics
The main ways to diagnose diseases that may cause a lump to appear:
- Inspection, questioning, palpation.
- Ultrasound, CT or MRI (studies that allow you to diagnose changes in the soft tissues of the joint).
- X-ray (a method used to detect changes in the bones of the joint, tissue calcification).
- Electromyography (a diagnostic method that allows you to study the functions of muscles and nervous tissue).
- Angiography (a method of examining blood vessels with the introduction of a contrast agent into them).
- Therapeutic and diagnostic puncture (extraction of fluid from formed cavities, synovial bursae, which allows you to quickly alleviate the patient’s condition and examine the contents).
- Laboratory tests, including histological examination of tissue fragments (for malignant cells).
1 – ultrasound examination; 2 – electroneuromyography; 3 – catheterization of the artery during angiography; 4 - puncture
Some studies are prescribed to exclude diseases that are similar in symptoms.
How to treat a lump under the knee at the back?
Before treating a lump under the knee at the back, you need to clarify the etiology of the origin of this clinical sign. Only the disease that provoked the appearance of the tumor can be treated. It is impossible to treat a lump at the back of the knee in isolation.
Therefore, first you need to make an appointment with an orthopedist. You can do this right now by exercising your right to a free initial consultation at our chiropractic clinic. We employ experienced doctors. During your first appointment, you will be given a preliminary diagnosis. As necessary, various types of examinations will be recommended to clarify the diagnosis. Information is also provided about the methods and methods, possibilities and prospects of the treatment.
In particular, if there was a sports (domestic) injury and after it a lump appeared under the knee at the back, but there was no discomfort in movement, then perhaps help would be in the use of massage and osteopathy techniques. The specialist, using special techniques, will ensure the drainage of lymphatic fluid from the posterior projection of the knee joint. The lump will go away on its own within a few weeks of treatment.
If bursitis or inflammation of the meniscus is diagnosed, then in such a situation treatment will begin with first aid to the patient. The doctor will relieve the pain and then a course of rehabilitation therapy will be developed.
Any treatment is developed strictly individually. The doctor takes into account all the individual characteristics of the patient. Therefore, you can find out detailed information regarding your case during an initial free consultation.
Treatment
With timely treatment, some of the pathologies that caused bumps on the knee are completely cured (bursitis, Baker's cyst, abscess). Some are incurable (tibial nerve neuropathy, if its cause is genetic diseases).
General principles of therapy for all diseases
Common in the treatment of 90% of joint pathologies is the following:
- non-steroidal anti-inflammatory drugs (NSAIDs);
- glucocorticosteroids (if NSAIDs are ineffective);
- hardware physiotherapy, massage, physical therapy exercises (at the recovery stage, in order to speed it up and quickly restore joint function).
General methods of treating knee joint diseases: 1 – non-steroidal anti-inflammatory drugs (for example, ibuprofen); 2 – corticosteroids (for example, prednisolone); 3 – magnetic therapy; 4 – medical massage
During treatment and during the recovery period, the load on the knee is limited.
Features of therapy for specific pathologies
| Pathology | Features of treatment |
| Baker's cyst | The fluid is removed from the bag, glucocorticosteroids are injected inside, a tight pressure bandage is applied Infectious and chronic bursitis is treated by excising the bursa |
| Prepatellar bursitis | |
| Inflammation of the tibial nerve | Treat the underlying disease (for example, diabetes mellitus), prescribe antidepressants, anticonvulsants and strong painkillers (Tramadol) When a nerve is compressed, surgical treatment is used |
| Popliteal artery aneurysm | Surgical bypass surgery (formation of a bypass artery) or artery stenting (installation of a reinforcing frame) is performed. |
| Schlatter's osteochondropathy | Treated by limiting the load and standard means (NSAIDs, physiotherapy), occasionally with surgical methods (restoration of the tibial tuberosity) |
| Abscess | The abscess is opened, the cavity is washed with antiseptics, and the patient is prescribed a course of antibiotics |
| Synovioma | The synovioma is surgically removed, chemotherapy and radiation therapy are used |