Introduction
In industrialized countries, there is a clear trend towards increased life expectancy and an increase in the number of older people in the population structure, which leads to certain socio-economic difficulties.
Age UK and the Office for National Statistics predict that by 2034, almost one in four people in this country will be over 65, with 58% of people over the age of 60 having a chronic condition and 25% having two or more conditions, which significantly reduces the working capacity of the population. Osteoarthritis and low back pain are the main causes of disability in the age group over 50 years [1]. In a comprehensive analysis, Hoy et al. (2010) on the epidemiology of back pain among the adult population [2] found that the frequency of lumbar pain ranges from 2% to 40% (on average 15%) and increases in older age groups. Back pain in older people has a number of features associated with such morphological changes in the spine as osteoporotic fractures, metastases, central or lateral spinal stenosis, degenerative spondylolisthesis and degenerative scoliosis [3]. According to the modern classification, lumbar pain is divided into:
nonspecific (musculoskeletal);
associated with diseases (tumors, injuries, infections, etc.);
caused by compression radiculopathy.
In 85% of cases in clinical practice, nonspecific (musculoskeletal, mechanical) pain occurs [3, 4].
The main task when examining a patient is to consistently exclude specific causes of spinal damage and diseases of the nervous system. The diagnosis is based on an analysis of the patient’s complaints, anamnesis data, and a standard neurological examination [5]. Red flags are signs, symptoms, or characteristics of a patient that indicate the need for additional testing to rule out potentially dangerous conditions. According to Henschke et al. (2009), the diagnostic value of “red flags” varies. The most dangerous are significant spinal trauma, severe or progressive neurological deficit, pelvic disorders, anesthesia in the anogenital area, and a history of cancer [6]. When observing a cohort of elderly people with back pain, a serious pathology was diagnosed in 6% of cases, mainly a spinal fracture. Multivariate regression analysis showed that 4 “red flags” were associated with the presence of this pathology: age ≥75 years, trauma, osteoporosis, high-intensity (≥7 points on the visual analogue scale [VAS]) pain in the lumbar or thoracic spine [7] .
The aging process is accompanied by changes in the structure and decrease in the functional activity of organs and tissues, including bone, with the development of osteoporosis [8, 9].
Diagnostic methods
The methods for identifying vertebral osteoporosis are the same as for establishing general skeletal pathology.
- Radiography. Usually it is informative only in advanced stages, when the bone mass “dries out” by 15–30%.
- Bone densitometry. Involves determining the density of bone tissue by the amount of absorbed x-rays.
- Radioisotope scanning. It is carried out using so-called radioactive markers, which settle only in skeletal tissues.
- Laboratory tests: biochemical tests of blood, urine, hormone test.
"Silent" disease
Osteoporosis is a condition in which bone mass decreases, causing loss of bone structure and strength, resulting in an increased risk of fractures. The most common method for diagnosing osteoporosis is densitometric assessment. To determine bone mineral density (BMD), the gold standard is dual-photon absorptiometry (DPA). To evaluate the T-score, a patient's BMD is compared to a reference BMD standard from a normative cohort aged 20 to 30 years. According to WHO recommendations (1994), osteoporosis is considered to be a decrease in BMD according to the T-criterion below -2.5; severe osteoporosis - a decrease in T-score below -2.5 in combination with one or more fractures [10].
The primary forms of osteoporosis include postmenopausal and senile, which make up 80% of all types, as well as juvenile and idiopathic. Postmenopausal osteoporosis, or type 1 osteoporosis, is characterized by predominant damage to trabecular bone tissue, a predominance of accelerated bone resorption, and develops in women from the onset of menopause to 65–70 years of age. Senile osteoporosis, as a rule, develops in people over 70 years of age, in bones with a cortical type of structure and in spongy bone; There is predominantly a decrease in bone formation, but variants with increased bone resorption are not uncommon. One in three menopausal women and more than half of the entire population aged 75–80 years suffer from osteoporosis. The prevalence of osteoporosis and the financial costs of treating associated fractures are steadily increasing, with 40% of the increase in prevalence due to the aging population [10, 11].
Secondary forms of osteoporosis occur against the background of somatic diseases or long-term use of drugs that cause calcium metabolism disorders.
In osteoporosis, the density of bone and vertebral bodies is reduced to 70% and 50%, respectively. A decrease in bone mass, as a rule, is asymptomatic, even with the development of vertebral body deformity and a decrease in disc height. While extremity fractures are usually painful, some types of vertebral fractures, especially wedge fractures, may not cause pain. Osteoporotic fractures with pain in the lumbosacral spine are more common in women: 25% of postmenopausal women have compression fractures of the spine, and 40% of those over the age of 80 years. The risk of vertebral fractures in osteoporosis varies greatly depending on the presence or absence of pre-existing vertebral fractures [12, 13].
The WHO FRAX score is used to estimate the 10-year probability of fractures associated with changes in bone density and bone quality (clinically significant vertebral fracture, distal forearm fracture, proximal femoral fracture, or humeral fracture). The FRAX algorithm is used in postmenopausal women and men 50 years and older. The scoring model takes into account age, sex, presence of rheumatoid arthritis and secondary causes of osteoporosis: type 1 diabetes mellitus, osteogenesis imperfecta in adults, long-term untreated hyperthyroidism, hypogonadism or premature menopause (<40 years), chronic malnutrition or malabsorption, chronic liver disease, as well as previous osteoporotic fractures (including clinical and asymptomatic vertebral fractures), parental hip fractures, smoking, low body mass index, alcohol consumption (≥3 drinks per day), use of oral glucocorticoids ≥5 mg/day prednisolone for >3 months ., decrease in BMD (if it is possible to evaluate it).
BMD correlates with bone strength and is the best predictor of fracture risk. Measurements in the central (lumbar spine and Ward's area of the hip) and peripheral areas of the skeleton (forearm, heel, fingers) allow us to assess the risk of fractures. In postmenopausal women and men over the age of 50 years, the WHO diagnostic T-criterion (normal, osteopenia and osteoporosis) is determined by measuring BMD using the DPA method in the lumbar spine and femoral neck [14].
According to the recommendations of the American Association of Clinical Endocrinologists (AACE) and the American College of Endocrinology (ACE), BMD assessment is indicated:
All women ≥ 65 years old.
For postmenopausal women:
with fractures without serious injury;
with osteopenia detected by x-ray;
taking glucocorticoid therapy (≥3 months)
Peri- or postmenopausal women with risk factors for osteoporosis such as:
low body weight (<57 kg or body mass index <20 kg/m2);
long-term systemic glucocorticoid therapy (≥3 months);
family history of fractures due to AP;
early menopause (<40 years);
smoking;
excessive alcohol consumption.
For secondary osteoporosis [15].
The presence of osteopenia should not be considered as an independent disease; the indication of osteopenia is intended solely for epidemiological description. Additional risk factors for fractures include decreased height (>4 cm) and thoracic kyphosis. Bone markers - serum procollagen type I amino-terminal propeptide (s-PINP) and C-terminal telopeptide of type I collagen (s-CTX) as indicators of formation and Bone resorption accordingly has some prognostic value for fractures in situations where BMD measurements are not available [16].
Radiologically confirmed vertebral fractures (even asymptomatic ones) are a sign of impaired bone quality and strength and a strong predictor of new fractures, regardless of BMD, age and other clinical risk factors. Having one vertebral fracture increases the risk of subsequent fractures by 5 times, and the risk of hip and other fractures by 2-3 times. A vertebral fracture confirms the diagnosis of osteoporosis, even in the absence of a pronounced decrease in BMD, and is an indication for pharmacological treatment to reduce the risk of subsequent fracture. Most vertebral fractures are asymptomatic when they first occur and often go undiagnosed for many years. Vertebral imaging is the only way to diagnose these fractures:
All women aged 70 years or older and all men aged 80 years or older if spine, total hip, or femoral neck BMD T-score is ≤ -1.0.
Women aged 65 to 69 years and men aged 70 to 79 years if the spine, total hip, or femoral neck BMD T-score is ≤ -1.5.
Postmenopausal women and men aged 50 years and older with specific risk factors: in the form of a traumatic fracture in adulthood (50 years and older), with a decrease in height by 4 cm, treatment with glucocorticoids.
Repeat imaging is indicated only if there is ongoing height loss, pain, or spinal deformity [14].
Features of lumbar pain in osteoporosis
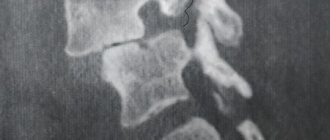
Osteoporosis of the vertebrae without fractures is not a source of pain. Changes in the configuration of the vertebrae are often an incidental finding during radiography. According to the literature, pain in the lumbar region with osteoporosis does not differ from pain in patients without osteoporosis, with the exception of cases of acute pain from fractures [3]. Compression fractures (a decrease in the height of the vertebral bodies by more than 20%) most often occur in the lower thoracic and upper lumbar regions. Fractures are typically characterized by the occurrence of acute local pain after a minor injury or even habitual movement; the pain intensifies with movement and coughing [8]. Provocation of pain during percussion of the spinous processes of the affected vertebra is typical. Difficult to diagnose are cases of sacral fractures, usually small ones. For such patients, pain in the lumbosacral region, deep pain in the gluteal region, sometimes radiating to the leg, without convincing radicular symptoms, which often occur after minor injuries or awkward movements, are typical. The pain intensifies with palpation and percussion in the projection of the fracture; small fractures are not visible with standard radiography; they are better visualized on CT or MRI.
A feature of radicular symptoms in osteoporosis is more frequent damage to the upper lumbar roots with irradiation of pain in the abdomen, groin, along the anterior and inner surface of the thighs. Relatively rarely, paresis of the lower extremities, pelvic disorders, and conduction disturbances of sensitivity are detected. There are indications of the possibility of chronic pain, predominantly of a muscular nature, against the background of severe spinal deformity, but the level of evidence for this data is very low [8, 10].
My own experience of studying the characteristics of low back pain in osteoporosis
On the basis of the Clinic of Nervous Diseases named after. AND I. Kozhevnikov, we conducted a pilot study, the purpose of which was to study the characteristics of pain syndrome in patients with chronic vertebrogenic lumbar sciatica and suffering from osteoporosis. 20 patients were examined, of which 10 patients (average age 65.2±5.27 years) were diagnosed with osteoporosis, and 10 patients (average age 63.9±5.67 years) without osteoporosis, who formed the control group. The objectives of the study included assessment of pain syndrome and neuroorthopedic status to identify the dominant source of pain, assessment of neuropsychological status and severity of spinal deformity. Diagnosis of osteoporosis was carried out using the method of quantitative ultrasound densitometry using the Omnisense 7000S device with a decrease in T-criteria -2.5SD
and below. Other methods of instrumental examination included: radiography of the lumbosacral spine in direct and lateral projections, CT and MRI of the lumbar spine. As part of the study, the disability index was assessed using the Oswestry Low Back Pain Disability Questionnaire and pain was assessed using the VAS. Taking into account the effect of osteoporosis on the biomechanics of the spine, the angle of kyphosis, lordosis and scoliosis was measured using a flexible rod according to the method proposed by M.A. Katbleen. To assess the severity of depression and anxiety, the Beck Depression Inventory, the Hospital Anxiety and Depression Scale, and the Hamilton test were used.
When studying the curvature of the spine, a statistically significant increase in the angles of thoracic kyphosis, lumbar lordosis and thoracolumbar scoliosis was found in patients suffering from osteoporosis (p<0.001). The level of pain according to VAS did not differ significantly between the groups and was 6.2±1.8 and 5.9±1.4 mm in patients with osteoporosis and patients without osteoporosis, respectively (p>0.5). Pain characteristic of dysfunction of the sacroiliac joint was detected in 8 patients with osteoporosis and 7 patients in the control group, pain in the facet joints at the lumbar level was detected in 6 and 4 patients, respectively. All 20 patients in both groups had muscular-tonic syndrome of varying severity, which manifested itself in tension and soreness of the paravertebral muscles, piriformis syndrome - in 3 and 2 patients of the corresponding groups. Radicular symptoms were detected in 1 patient with osteoporosis and 2 in the control group. When assessing anxiety and depression, the degree of disability in the 2 groups, no statistically significant differences were obtained, but there was a tendency for them to predominate in the group of patients with osteoporosis.
In summary, our pilot study demonstrated that osteoporosis per se is not a cause of chronic low back pain in elderly patients. There were no statistically significant differences in sources of pain, pain intensity, degree of anxiety-depressive disorders and degree of disability in patients with chronic lumbar pain syndrome, with and without osteoporosis.
Osteoporotic deformity of the vertebrae leads mainly to severe postural disorders, accompanied by an increase in thoracic kyphosis, flattening of the lumbar lordosis and S-shaped lumbar-thoracic scoliosis, which can also be the cause of secondary muscle spasm. Given the small size of the patient groups included in the study, this issue requires further study.
Kinds
Osteoporosis can be primary or secondary. The first develops due to age or hormonal imbalances in the body. The greatest risk of getting sick is observed in women over 55 years of age.
Secondary osteoporosis develops under the influence of developed degenerative processes. It can be:
- autoimmune diseases;
- genetic predisposition;
- rheumatism;
- long-term medication use.
The most common triggers are menopause and old age.
Features of management of patients with back pain in the presence of osteoporosis
Treatment of patients with back pain in the presence of osteoporosis is carried out in accordance with the general principles for the management of nonspecific back pain, developed in international clinical guidelines. In general, most guidelines for the treatment of nonspecific back pain recommend patient education programs, staying active, exercise, and the use of NSAIDs as first-line treatment [15–17]. Treatment of chronic low back pain should include exercise, NSAIDs, and multimodal rehabilitation (a combination of physical and psychological treatments) [11]. A meta-analysis of several randomized controlled trials (RCTs) showed that walking is one of the most effective, safe and accessible methods of therapeutic exercise [18].
The use of an integrated approach, including physical and psychological rehabilitation, with the use of cognitive behavioral therapy, is indicated if there are real psychosocial aspects that impede recovery, as well as if treatment is ineffective [15].
Patients with osteoporosis should receive treatment for the underlying disease, in accordance with international and domestic clinical guidelines for the management of osteoporosis; in addition, the treatment of patients with lumbar pain due to osteoporosis has a number of features. Two key elements in the treatment of osteoporosis are increasing bone mass with anabolic therapy and decreasing bone resorption with antiresorptive therapy.
According to ESCEO recommendations, postmenopausal patients are recommended to have a higher intake of protein and calcium-containing foods in combination with physical exercise due to the risk of developing osteoporosis [17].
Physical activity has been proposed as a non-pharmacological method to increase bone density in young people and prevent bone loss in older people [19]. Exercise programs have been shown to reduce the risk of fractures by increasing bone density, reducing inflammatory markers [20], and improving strength and coordination in aging women with osteoporosis, reducing the risk of falls [21]. At the same time, bone tissue remodeling requires fairly intense dynamic exercises, which are difficult for older women to perform [22].
The skeleton contains 99% of the body's calcium reserves. When exogenous calcium supply is insufficient, bone tissue is resorbed to maintain a constant serum calcium level. A balanced diet rich in low-fat dairy products, fruits and vegetables provides calcium. Calcium supplements may be prescribed up to the recommended daily dose. Adequate calcium intake throughout life is essential for the acquisition of peak bone mass and subsequent maintenance of bone health. According to the US Institute of Medicine (IOM), men aged 50–70 years should consume 1000 mg of calcium per day; women aged 51 years and older, men aged 71 years and older - 1200 mg of calcium per day. The National Osteoporosis Foundation recommends intake of at least 1200 mg of calcium per day and 800–1000 IU of vitamin D per day for postmenopausal women [23, 24]. There is no evidence that calcium intake above these amounts provides additional bone strength. Excessive calcium intake (more than 2000 mg per day) can be potentially harmful. An increased risk of cardiovascular events, urolithiasis, and even fractures has been found in association with excessive calcium intake, but this issue remains unresolved [25].
There is a high prevalence of vitamin D deficiency in patients with osteoporosis, especially those with hip fractures. The vitamin D intake recommended by the IOM is 600 IU/day for those aged under 70 years and 800 IU/day for those aged 71 years and over. According to a meta-analysis of RCTs (Weaver et al., 2016), the use of calcium and vitamin D supplements reduces the risk of fractures by 15% and hip fractures by 30% [22].
Osteogenon (active component: ossein-hydroxyapatite compound [OHS]) is a drug that affects bone mineralization (regulator of calcium-phosphorus metabolism), contains components necessary for the synthesis of bone tissue and has a dual effect on bone metabolism: stimulates osteoblasts and inhibits osteoclasts. Calcium is contained in the drug in the form of hydroxyapatite (in a 2:1 ratio with phosphorus), which promotes more complete absorption from the gastrointestinal tract. Inhibits the production of parathyroid hormone (PTH) and prevents hormonally caused bone resorption. The slow release of calcium from hydroxyapatite results in the absence of a hypercalcemia peak. Phosphorus, which participates in the crystallization of hydroxyapatite, promotes the fixation of calcium in the bone and inhibits its excretion by the kidneys.
Ossein is an organic component of the drug that contains local regulators of bone tissue remodeling (β-transforming growth factor, insulin-like growth factors I and II, osteocalcin, collagen type I), which activate the process of bone formation and inhibit bone resorption. β-transforming growth factor stimulates the activity of osteoblasts, increases their number, promotes collagen production, and also inhibits the formation of osteoclast precursors. Insulin-like growth factors I and II stimulate the synthesis of collagen and osteocalcin. Osteocalcin promotes the crystallization of bone tissue by binding calcium. Type I collagen ensures the formation of the bone matrix. In the study conducted by S.S. Rodionova et al. (2006) study, when OGS was prescribed to patients with postmenopausal and senile osteoporosis, whose bone loss before treatment exceeded 30–40% of the age norm, vertebral body fractures were observed less frequently than in women from the control group who did not take this drug (6, 7% versus 40%). In addition, patients in the control group continued to lose BMD in the vertebral bodies [26].
A randomized, open-label, parallel-group, prospective controlled trial compared the effects of OGS (treatment group) and calcium carbonate (control group) on bone metabolism in a group of women over 65 years of age with densitometrically confirmed osteoporosis. Serum osteocalcin levels increased to a greater extent in patients in the OGS group compared with those in patients receiving calcium carbonate. In patients in the OGS group, osteocalcin levels increased by 0.84±3.13 ng/ml in the 2nd year and by 1.86±2.22 ng/ml in the 3rd year of the study, whereas in patients receiving calcium carbonate , this indicator decreased by 0.39±1.39 ng/ml in the 2nd year and increased by 0.31±2.51 ng/ml in the 3rd year of the study (data presented as mean ± standard deviation); differences between treatment groups were statistically significant (p<0.05 in all cases). Changes over time in serum osteocalcin levels were also statistically significant (p < 0.05) in the OGS group but not in the calcium carbonate group. Changes in mean BMD at the lumbar spine and femoral neck between baseline and year 3 were 1.1% and 2.5% for OGS; 2.3% and 1.2% for calcium carbonate, respectively. It was concluded that OGS has a greater anabolic effect [27]. In addition, a pronounced analgesic effect was revealed in the OGS group for back and knee pain, as well as an improvement in quality of life indicators [28].
According to the clinical recommendations of the Ministry of Health of the Russian Federation for the treatment of pathological fractures complicating osteoporosis, in the first year after a fracture, it is recommended to take OGS complex as a calcium supplement (level of confidence of recommendation B, level of certainty of evidence 3) [29], the advantages of which over the use of calcium carbonate are described higher [27, 28]. The use of OGS normalizes the time for fracture healing against the background of osteoporosis or osteopenia and shortens the time for bone healing in pseudarthrosis [30, 31].
Specific treatment is recommended for postmenopausal women who have a BMD of T=-2.5 or less, a history of vertebral or hip fracture, or an increased risk of fracture according to the FRAX score. FDA-approved pharmacologic options for the prevention and/or treatment of postmenopausal osteoporosis include: bisphosphonates (alendronic acid, ibandronic acid, zoledronic acid), calcitonin, estrogens, estrogen receptor agonist/antagonist (raloxifene), tissue-selective estrogen complex (conjugated estrogens/bazedoxifene) , PTH and denosumab is a fully human monoclonal antibody (IgG2) that has high affinity and specificity for RANKL (RANK receptor ligand), thereby preventing the activation of RANK receptors on the surface of osteoclasts and their precursors. The benefits of FDA-approved medications for preventing fractures have been shown primarily in women with postmenopausal osteoporosis. There are limited data on fractures in glucocorticoid-induced osteoporosis and in men. FDA-approved osteoporosis treatments have been shown to reduce the risk of fractures in patients with fractures and/or DPA-confirmed osteoporosis. Pharmacotherapy may also reduce the risk of vertebral fractures in patients with low bone mass (osteopenia) without fractures; the level of evidence is low [14, 32].
In 2021, experts from the American College of Physicians released updated Clinical Guidelines for Fracture Prevention in Osteoporosis and Osteopenia, which include:
Alendronic acid, risedronic acid, zoledronic acid, or denosumab are indicated to reduce the risk of hip and vertebral fractures in women with proven osteoporosis (strong recommendation, high level of evidence).
Duration of therapy should be 5 years (weak recommendation; low-quality evidence).
For men with clinically proven osteoporosis, bisphosphonates are recommended (weak recommendation; low-quality evidence).
During the period of pharmacotherapy, patients do not need densitometry monitoring (weak recommendation; low quality of evidence).
The use of hormone replacement therapy or raloxifene for the treatment of osteoporosis in women is not recommended (strong recommendation; moderate quality of evidence).
Decisions about treatment for women with osteopenia over 65 years of age at high risk of fracture should be based on an analysis of patient preferences, fracture patterns, potential hazards and cost of treatment (weak recommendation; low-quality evidence) [33].
Bisphosphonates and denosumab reduce the risk of hip and vertebral fractures. Bisphosphonates are usually used as first line of treatment in women who have no contraindications. In women intolerant of oral bisphosphonates (or in whom they are contraindicated), intravenous bisphosphonates or denosumab are the most appropriate alternatives, with raloxifene or menopausal hormone therapy as additional options. PTH reduces the risk of developing nonvertebral and vertebral fractures. Osteonecrosis of the jaw and atypical femoral fractures have been reported during treatment but are rare. The benefit-risk ratio for treating osteoporosis is positive for most women with osteoporosis. Because benefits persist after discontinuation of alendronic acid or zoledronic acid, use after 5 years of alendronic acid therapy or 3 years of zoledronic acid therapy may be considered in patients at lower risk of fracture. Treatment should be reconsidered after 3–5 years of bisphosphonate treatment. The risk of fracture should be reassessed after a new fracture, regardless of when it occurred. The risk of new clinical and vertebral fractures increases in patients who discontinue treatment. Discontinuation of denosumab therapy is associated with a recovery in the incidence of vertebral fractures. Bisphosphonate therapy may be considered after discontinuation of denosumab. There is little evidence to guide decision making after 10 years of treatment, and treatment options in these patients must be considered on an individual basis [14–16].
The Global Spine Care Initiative Expert Panel (2017) published recommendations for the use of noninvasive treatments for acute vertebral compression fractures due to osteoporosis. In addition to bed rest and pain relief, these patients are recommended to wear corsets and use calcitonin due to its analgesic effect. Early mobilization is indicated, and when a sufficient level of pain relief is achieved, gymnastics is effective to improve functional status and improve quality of life [34].
In a systematic review, Parreira et al. (2017) of various recommendations for the management of patients with compression fractures of the vertebral bodies emphasize the lack of a unified proven position. Most guidelines recommend the use of radiography and DPA for diagnosis and vertebroplasty and kyphoplasty for treatment. Various recommendations contain conflicting data regarding the prescription of bed rest, corsets, electrical stimulation, and gymnastics [35].
Patients with osteoporosis and a high risk of fracture should not perform trunk flexion exercises due to the fact that such loads increase the risk of vertebral fracture (Class IIA recommendation); Intensive twisting movements of the torso and exercises for maximum stretching of the spine should be avoided (III C). Extension and stabilization exercises for the abdominal muscles (IIA), various aerobic physical activities or resistance training are considered safe. It is recommended to start with light loads (15–30 min each), with a gradual increase in intensity, taking into account individual tolerance (IIA) [36, 37].
If conventional treatment is insufficiently effective, blockades of local anesthetics and glucocorticoids may be used, depending on the main source of pain, and for acute fractures, intraosseous administration is possible; with a short-term effect of blockades, radiofrequency denervation can be performed [3]. The use of a short course of glucocorticoid blockade is safe in postmenopausal women with osteoporosis and does not affect the risk of osteoporotic fractures [38].
How does osteoporosis occur?
Human bone tissue is constantly renewed.
Two types of cells are involved in this process: osteoclasts and osteoblasts. Osteoclasts destroy bone mass, and osteoblasts recreate it. In osteoporosis, osteoclasts are activated, and bone tissue is destroyed faster than it is formed. Bones become porous and brittle, and fractures occur easily. The disease most often affects the vertebrae, pelvic bones, wrists and forearms. Most bone tissue is formed at the age of 16, when bone formation prevails over destruction. At the age of 30-50, the destruction and restoration of bone tissue occurs at the same pace. After 50 years, the processes of bone tissue destruction accelerate. Every year, older adults lose 2–5% of their bone mass. Thus, osteoporosis of bones occurs due to the aging of the body. The disease develops gradually over several years.
Complications
According to statistics, osteoporosis is one of the leading causes of disability and mortality. The main complications of the pathology are fractures:
- femoral neck;
- radius bones;
- vertebrae
Bone fractures force patients to remain in bed for a long time.
As a result, the risk of bedsores and pneumonia increases. Severe stages of osteoporosis lead to external physical defects that contribute to impaired self-care. Therefore, it is important to diagnose the pathology in time and carry out correct treatment. If osteoporosis is detected, you must strictly follow your doctor's recommendations. Make an appointment