First aid
The correctness and timeliness of the provision of pre-medical care often determines further treatment and recovery time for the patient.
Initially, you should carefully secure your hand - apply a support bandage or tape your hand to a splint. If the shoulder and elbow joints are immobilized at the same time, then the limb is fixed correctly.
If the wound is open, it must be thoroughly washed and disinfected.
If the arm does not bend at the elbow, it should be tied to the body. The main thing is to do everything carefully, without using force.
The victim's pulse should be periodically checked. If it disappears, you need to remove the bandages from your arm and carefully straighten it to restore blood flow. Afterwards, the arm should be secured again with a bandage.
Complications from shoulder fractures
Complications of humerus fractures : - occur quite often and in the long-term period in certain cases or with inadequate treatment are represented by non-united fractures, improperly fused fractures, as well as pseudarthrosis (false arthrosis).
At the time of injury, fractures of the humerus can be complicated by damage to the structures surrounding the humerus: damage to the neurovascular bundle, muscles and tendons manifested by bleeding, neurological disorders in the injured arm, and dysfunction of the upper limb.
Closed fracture of the surgical neck of the humerus before and after surgery. Osteosynthesis was performed with a plate.
Types of treatment:
- Conservative therapy is carried out using medications. After the limb is anesthetized, in case of a closed fracture, bone fragments are compared, and then the limb is fixed.
- Surgical intervention. The traumatologist returns the displaced fragments to their original state. There is an open and closed method.
- Skeletal traction. This type of treatment is used infrequently, if other methods fail, if the fragments diverge significantly and it is impossible to compare them. The technology consists of installing a pin that matches and sets the fragments. Next, a special type of plaster cast is applied for a month. The patient must remain in bed.
Diagnosis of shoulder fractures
Diagnosis of humerus fractures is a clinical examination of the patient (examination, comparative assessment, measurement, palpation, etc.), X-ray examination is standard radiography, special X-ray placement if necessary.
X-ray computed tomography to verify soft tissue damage is an MRI. To make an accurate and correct diagnosis, as well as to determine further treatment tactics, it is very important that the diagnosis is carried out by a qualified specialist doctor - an orthopedic traumatologist.
Anatomy of the elbow joint.
Your elbow joint is made up of 3 bones: the humerus, the radius, and the ulna. The elbow joint undergoes flexion and extension due to the movement of the ulna around the humerus. Also in the elbow joint, rotation or rotation of the head of the radial bone occurs, the radial bone itself seems to intersect with the ulna, and rotation of the forearm occurs.
The elbow joint itself is formed by the lower end of the humerus and the upper ends of the ulna and radius.
The elbow joint is held in its physiological position due to the architecture of the bones that form it, the articular capsule, which envelops their articular ends like a bag, and a large number of ligaments. Fractures of the lower end of the humerus, including the articular surface, are characterized by the presence of a large number of small fragments.
Such fractures are called comminuted or multifragmentary. In most cases, these fragments are displaced relative to each other.
Acute symptoms of a fracture of the humeral head
Acute symptoms include:
- Shoulder pain.
- Movement restrictions.
- Posture distortion
- Shoulder swelling.
- Hematoma.
As with all fractures, the main symptom of a humeral head fracture is pain. Most are unable to move their arm without pain and usually hold the injured arm close to the chest in a relaxed position.
The shoulder sometimes swells significantly. With a fracture, hematomas may be delayed and spread throughout the arm after a few days. Nerve injuries or open fractures (lacerations that break the skin) are rare.
Symptoms
The pathological phenomenon has a characteristic clinical picture, which is characterized by the following symptoms:
- pain syndrome due to rupture of soft tissues, ligaments, capsular damage or separation of fragments of the cartilaginous ridge,
- deformity in the shoulder joint,
- impaired sensitivity of the hand, forearm, shoulder due to compression of nerve fibers by displaced bone,
- swelling, tissue inflammation,
- stiffness because the displaced bone reduces the natural range of motion.
Such manifestations are serious and require immediate visit to a specialist.
Causes of fracture of the humeral head
Possible causes include osteoporosis, accidents and tumors. In the case of a proximal fracture of the humeral head, one or more fractions are displaced towards each other. In addition, the attending physician must determine exactly where the head of the humerus is broken.
Humeral head fractures are common in children with low bone density. A typical accident is a fall on an outstretched arm. The fracture may occur indirectly due to compression of the outstretched arm or elbow. But fractures rarely occur as a result of direct impact.
For people with osteoporosis, a simple fall from a low height while standing is often enough - tripping over a curb or slipping on a smooth surface is enough to cause the head of the humerus to break. Bones with weak bone substance break even with low fall energy.
In rare cases, a malignant tumor in the bone causes a fracture of the head of the humerus due to weakening of the internal bone substance. These fractures often resolve spontaneously, without a pattern of trauma.
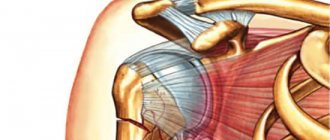
Shoulder instability
Shoulder instability (habitual dislocation of the humeral head).
The shoulder joint is the most mobile joint in the human body; the ligamentous apparatus and joint capsule are less durable compared to other large joints.
Figure: Ligamentous apparatus of the shoulder joint.
These factors predispose to humeral head dislocation, which is the most common dislocation in the human body, which in turn leads to the development of shoulder instability (habitual dislocation).
Figure: Position of the hand when the head of the humerus is dislocated.
Primary dislocation of the head of the humerus occurs due to injury: a fall on the arm, a pull on the arm, a blow to the shoulder joint. The injury is accompanied by damage to such structures as: the capsule, ligaments, fibrocartilaginous lip, and, sometimes, bone components (the head of the humerus and the articular process of the scapula).
A) B)
Figure: a) avulsion of the capsular-ligamentous complex, b) Hill-Sachs injury of the head of the humerus (impression fracture).
Elimination of a primary dislocation occurs, as a rule, in a medical facility under anesthesia, and then the shoulder joint is immobilized in a cast or orthosis for up to 4-6 weeks.
A) B)
Figure: a) Elimination of dislocation according to the Hippocratic method, b) Plaster immobilization of the shoulder joint.
Thus, treatment of primary dislocation of the humeral head is predominantly conservative (without surgery). However, very often after a primary dislocation of the humeral head, instability of the shoulder joint develops (habitual dislocation), and therefore many orthopedic specialists in Russia and abroad believe that any primary post-traumatic dislocation in the shoulder joint, especially in young patients, requires surgical treatment: arthroscopy shoulder joint and restoration of the capsular-ligamentous complex. Many patients, after a primary dislocation, experience relapses (repeated cases) of dislocations in the shoulder joint, then the so-called instability of the shoulder joint develops, which in the domestic literature is historically called “habitual dislocation of the head of the humerus” or “habitual dislocation of the shoulder.” The direction of instability of the shoulder joint is usually anterior (up to 90%), however, in some cases, posterior dislocation of the humeral head occurs, leading to posterior instability of the shoulder. Diagnosing instability requires a comprehensive approach. History taking and clinical examination were the main means of diagnostic search. At the stage of collecting an anamnesis, the mechanism of injury during primary dislocation, the presence and nature (if any) of injury during recurrent dislocation after surgery, the number of dislocations or subluxations are clarified.
The clinical examination of each patient includes: a thorough history taking by interview, palpation of the shoulder joint, determination of the volume of passive and active movements in the shoulder joint (flexion, abduction, external and internal rotation), the presence and severity of pain during active and passive movements, during sports and at home. Specific tests are performed to determine instability in the shoulder joint.
An instrumental examination of the shoulder joint is mandatory and includes magnetic resonance imaging and computed tomography of the shoulder joint. Magnetic resonance imaging can assess the extent of damage to the anterior labrum and other soft tissues of the shoulder joint, in particular damage to the rotator cuff.
Figure: Bankart lesion of the anterior labrum.
Figure: MRI section of the shoulder joint, allowing to assess the condition of the rotator cuff (a tear of the supraspinatus muscle was revealed).
Computed tomography (CT) can clearly identify hypoplasia of the articular process of the scapula and its abnormal position in space. CT scans assess the presence and extent of glenoid bone deficiency and the severity of Hill-Sachs damage to the humeral head. CT scan in 3D (three-dimensional reconstruction) mode clearly demonstrates damage to the bone structures of the glenoid of the scapula and the head of the humerus. Based on the CT scan data, the degree of glenoid deficiency and the degree of Hill-Sachs type damage are calculated.
Figure: Comparative characteristics of the articular surfaces of the scapula of the right and left shoulder in three-dimensional reconstruction mode, clearly demonstrating the presence of bone deficiency of the scapula.
Figure: 3D CT scan showing a Hill-Sachs defect of the humeral head.
Based on a comprehensive examination of the patient, we use one or another surgical technique to treat instability of the shoulder joint (habitual dislocation). At the moment, 2 types of operations are most widely used: arthroscopy of the shoulder joint and arthroscopic restoration of the capsular-ligamentous apparatus (Bankart injury) using anchor fixators and Latarget osteoplastic surgery. In the absence of a significant bone defect of the articular process of the scapula, arthroscopy of the shoulder joint and stabilization - restoration of the Bankart lesion - is performed.
Figure: Schematic illustration of Bankart damage repair using anchors.
Figure: Intraoperative photographs of arthroscopic repair of a Bankart lesion using anchors.
The operation is practically free of complications. It is performed minimally invasively through 2-3 skin punctures. The stabilizing effect of the operation can be supplemented by treating the anterior capsule with a holmium laser, which leads to an increase in the strength of the capsular-ligamentous structures. The patient may already be discharged 2-3 days after surgery for outpatient follow-up care. The rehabilitation period after arthroscopic repair of a Bankart injury takes 6-8 months.
If there is a concomitant Hill-Sachs injury, we perform a “reimplissage” manipulation, when the infraspinatus tendon is fixed into the defect area.
Figure: Arthroscopy of the shoulder joint: Stages of the remplissage procedure.
In case of severe deficiency of the bone structure of the articular process of the scapula, we perform Latarget osteoplastic surgery for transposition of the coracoid process. The operation is performed both openly - through a small skin incision of 6-8 cm along the anterior surface of the shoulder joint, and arthroscopically (arthroscopic Latarget operation).
Figure: Schematic representation of the graft position.
Figure: CT scan after 6 months. after surgery and graft engraftment.
The rehabilitation period after Latarget osteoplastic surgery ranges from 6 to 12 months and requires control computed tomograms to confirm graft growth.
Both after arthroscopic surgery to repair a Bankart lesion using anchors, and after Latarget osteoplastic surgery, patients return to a full-fledged everyday and sports life.
Thus, we have and master the entire arsenal of diagnostic and therapeutic procedures to treat the complex problem of shoulder instability. Contact our clinic and you will be in reliable and capable hands!
Conservative therapy
Adequate pain-relieving therapy using active herbal ingredients (eg, nettle leaves) and non-steroidal pain relievers (ibuprofen, ketoprofen) helps the child control the inflammatory reactions of shoulder osteoarthritis.
Special physiotherapy exercises support and improve shoulder function, relieve pain and ensure good mobility of the shoulder joint. The child must follow all the doctor’s recommendations, undergo additional training, learn new sequences of movements and rules of behavior in order to adapt his lifestyle to the injured shoulder.
Conservative treatment includes painkillers, such as: metamizole sodium - 2.0 ml, trimeperidine - 1.0 ml, tramadol - 1.0 ml, diphenhydramine - 1.0 ml. Based on 0.1 ml per 1 year of a child’s life. In addition, ketorolac 30 mg/ml – 1.0 ml is prescribed.
During surgical treatment of a fracture, the following is prescribed:
– Cefazolin. 1 g IV – 1 time 30-60 minutes before the skin incision; for surgical operations lasting 2 hours or more - an additional 0.5-1 g during surgery and 0.5-1 g every 6-8 hours during the day after surgery.
– Cefuroxime. 750 mg IV – 1 time 30-60 minutes before the skin incision.
- Ceftriaxone. 50-70 mg per kg body weight IV – 1 time 30-60 minutes before the skin incision. No more than 10 mg/min is administered; the duration of infusion should be at least 60 minutes.
Other types of treatment:
exercise therapy;
Physiotherapy:
- magnetic therapy (5-10 procedures).
- UHF therapy (5-10 procedures).
- UV-therapy (5-10 procedures).
- laser therapy (5-10 procedures).
The body's natural responses to heat, cold, light, water and electrical stimuli support the healing process and relieve pain associated with osteoarthritis. Physical therapy works with these stimulating triggers and thus stimulates the body to heal itself.
Treatments such as shock wave therapy, biomechanical stimulation and deep heat are aimed at accelerating the healing and regeneration process.