The well-known expression “if a disease cannot be cured, this does not mean that a person cannot be helped” is also relevant in relation to childhood scoliosis.
Ilya Yuryevich Kulguskin, a traumatologist-orthopedist, head of the consultative and diagnostic department of the St. Vladimir Children's City Clinical Hospital in Moscow, told us about the dangerous consequences of this disease in children, as well as about modern methods of its treatment under compulsory medical insurance.
Why is a diagnosis of scoliosis dangerous for a child?
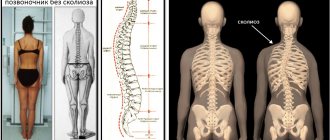
Scoliosis is not just a violation of posture in a child. This is a serious disease of the spine, characterized by both visible cosmetic defects in the form of hibuses (in other words, humps), and changes in the static functions and dynamics of the spinal column, which lead to disruption of the vital functions of the body as a whole.
Most often, such children, as they grow, suffer from early osteochondrosis, severe pain and impaired cardiopulmonary activity.
Preventive measures
Of course, scoliosis is easier to prevent than to cure. The main preventive measures that can help prevent the disease are the following :
- Taking medications with folic acid and vitamin B12 by the expectant mother during pregnancy.
- Constant monitoring of the child's posture.
- Enrichment of children's and adolescents' diets with foods rich in vitamins.
- Accustoming your child to do daily exercises and exercises.
- Providing the child with an orthopedic mattress.
- Accustoming a child to active sports, in particular volleyball.
- Regular visits to the pool by your child.
What is the classification of scoliosis?
Previously, scoliosis was divided into congenital and acquired. Modern orthopedics defines congenital scoliosis as a pathological form of vertebral formation during prenatal development. Such severe bone deformities are fortunately quite rare.
Acquired scoliosis is today called idiopathic. This is an intrauterine disorder of the formation of connective tissue, which leads to weakness of the ligamentous apparatus and muscle corset. With age, the vertebrae are not held in the correct position and they rotate (twist) relative to each other, which leads to curvature of the spinal arch. Thus, both types of scoliosis have a genetic predisposition.
4 degrees of idiopathic scoliosis
- 1. The first degree
is the most insignificant, in which the deviation of the spinal axis does not exceed 10⁰ and, as a rule, does not cause cosmetic defects or pain. - 2. The second degree
of scoliosis is characterized by a deviation of the spinal axis from 10⁰ to 25⁰. - 3. Third degree
- from 25⁰ to 50⁰. As a rule, after growth stops, the disease does not progress. Spinal deformities of more than 40⁰-45⁰ progress with age. - 4. The fourth degree
of scoliosis is characterized by an arc of curvature of more than 50⁰. Patients have severe bone deformity and severe pain. In this case, there are indications for surgical correction.
With the uncontrolled use of various gadgets, postural disorders and spinal deformities in children have become much more common.
Specific manifestations
The third form has specific signs of manifestation. If the first and the beginning of the second degree are mostly asymptomatic, but this cannot be said about the third. The symptoms are vivid and have the following description.
- Vertebral deformity, clearly visible visually, often in the form of the letter S.
- Severe distortion of the pelvic line in any direction.
- The slope of the shoulder line.
- Asymmetry of the scapular line.
- A pronounced stoop, a “drooping” appearance with drooping shoulders and head and an arched back.
- Concave chest or at least slightly sunken, changing shape.
- Severe pain that is felt in the area of the back where the curvature forms.
- Formation and growth of the costal hump.
- Tilt of the head to the shoulder in the direction of the curvature.
- Slight or severe decrease in sensitivity.
- The presence of shortness of breath regularly or during physical activities.
- Rapid and extreme fatigue even with the slightest physical effort.
Scoliosis of the third degree
With stooping, which always accompanies (even precedes) this form of scoliosis, the pectoral muscles become shorter, and the spinal muscles, on the contrary, lengthen due to stretching. Contractures (limitations in joint mobility) may appear.
An indispensable and obvious sign of tertiary scoliosis is pain syndrome, which may not be constant, but is felt immediately after static exercise or physical activity.
Physical activities and stress cause pain in patients with third degree scoliosis
A disease of a degree higher than the second often brings the body closer to displacement, displacement of internal organs or compression, which becomes the main cause of pathology of cardiac function or the occurrence of respiratory failure. In this situation, shortness of breath occurs, accompanied by reduced ability to work and constant fatigue.
What determines whether scoliosis will progress in a child?
From the combination of many factors: detection of the disease at an early stage, adequate therapeutic measures, the formation of the correct stereotype of posture and the absence of other somatic pathologies.
Scoliosis is also divided into stable and mobile deformities. This is diagnosed by x-ray. Scoliosis is mobile if the curvature of the spine changes depending on position. For example, in a standing position 25⁰, and in a lying position - 12-15⁰. When the difference in degrees between these two positions is more than 5-7, we talk about mobile deformation. It is considered a prerequisite for further progression of scoliosis.
Scoliosis is considered stable when there is a slight difference, up to 5⁰. In this case, the course of the disease will be calm and, in most cases, scoliosis does not progress.
Diagnostics
Diagnosis of scoliosis includes medical history, examination and neurological status. The medical history may include questions about the parents' genealogy. Has anyone in your family had scoliosis? If so, was any treatment given? In addition, the patient’s age and the onset of puberty are important to determine how many years are left before the completion of skeletal formation. As a rule, the progression of scoliosis less than 40-45 degrees stops after skeletal formation is completed. If the degree of curvature is more than 40-45, then progression can continue after maturation. Examination and neurological status allows us to establish a starting point for monitoring the development of the disease. A typical examination looks like this:
| Study | Description |
| Physical examination | The attending physician examines for the presence of asymmetries of the torso, such as uneven shoulders and pelvis. |
| The cardiovascular system | Heart and lung functions are checked |
| Adam's test | The patient leans forward with his arms extended forward. The doctor looks for the presence of a protruding shoulder blade or curvature of the pelvis. |
| Leg length | The length of the legs is measured (to check for differences). |
| Vertical line | The vertical line is measured using a plumb line from the 7th cervical vertebra, and it should pass between the buttocks. With scoliosis, this line deviates. |
| Range of motion | The doctor studies the patient's ability to flex, extend, bend and turn. |
| Palpation | The doctor checks for abnormalities by touch. Most often, problems can be detected from the ribs. |
| Neurological status | By conducting a neurological examination, the doctor receives information about reflex function, sensitivity disorders, and muscle strength. |
Is adult scoliosis different from childhood scoliosis?
No different, this is just one of the deep-rooted myths among the population. Scoliosis in children and scoliosis in adults are the same disease. Yes, there are secondary scoliosis after removal of spinal tumors, which can develop in adulthood, but this is a fairly rare case. Scoliosis always begins in childhood and, only as it progresses, leads to pain, decreased performance and irreversible changes in the bone structure of the vertebrae and the functioning of internal organs.
Scoliosis cannot be completely cured, but it is possible to stop its development and correct cosmetic defects that reduce the child’s quality of life.
Causes
In the vast majority of cases, the cause remains unknown, and scoliosis is considered idiopathic. Increased risk factors are:
- asthenia;
- sedentary lifestyle;
- serious loads on the spine, exceeding its capabilities;
- bad posture.
The curvature is congenital, when a child is born with various anomalies of the vertebrae, spinous processes and ribs. They can be underdeveloped (hemivertebrae) and fuse together, which is more often observed in the lumbar region and is detected in the form of lumbarization or sacralization.
Acquired scoliosis often occurs due to traumatic injuries, including congenital hip dislocations, different leg lengths, and problems with flexion and extension of large joints of the lower extremities.
Curvature of the spine can be of neurogenic, metabolic, rheumatic origin and develop against the background of diseases such as:
- poliomyelitis, Friedreich's ataxia, cerebral palsy, syringomyelia;
- myopathy, muscle dystrophy;
- rickets, cystinosis, bone formation disorders, Hunter syndrome;
- rheumatoid arthritis;
- osteochondrosis, neurofibromatosis.
Can parents themselves determine whether their child has scoliosis?
Yes, this is real on a visual level. It is worth paying attention to the child while swimming, relaxing on the beach, or simply when he walks around the house with a naked torso. If one shoulder is slightly higher, if the shoulder blades are at different levels, if one hip seems to be protruding forward, this is a reason to immediately consult an orthopedic doctor. Especially if you notice that your child often slouches.
After the examination, the doctor will decide whether the child needs additional diagnostic methods: x-ray or computer-optical topography. If everything is clear with the first method - it is an X-ray image in a normal projection, then the second method is more interesting for a small patient. Let me make a reservation right away: it does not replace radiography.
Computed optical topography is a simple photograph of a child by projecting dark and light stripes of light onto the dorsal surface of the torso (i.e., the back) and then evaluating the resulting three-dimensional image. It is used as a screening technique because it does not require “heavy” equipment (X-ray machine) and is absolutely safe - there is no radiation dose to the body. After such screening, a group of patients is identified that needs an X-ray examination. Based on x-rays, the degree of curvature and further treatment tactics are already determined.
Treatment methods
Conservative treatment methods
Some patients can be treated conservatively, while others require only surgical treatment. If the deviation is less than 15-20 degrees, it is enough to carry out exercise therapy and massage; there is no need for corsetry. If the deviation is more than 20 to 40 degrees, it becomes necessary to wear a corset in order to avoid progression of the curvature. Teenagers are not always comfortable wearing a corset for a long time, but given that in many cases this can be avoided by surgery, wearing corsets is justified. In addition, gentle physical activity (individually selected) is recommended. Unfortunately, physical activity and corseting do not always give the expected effect, especially when the curvature is in the cervicothoracic region or more than 40 degrees.