Spondylitis
is a disease of the spine of inflammatory etiology.
First of all, it affects the vertebral body, destroying it and reducing its height. In severe cases, a hump may form, ossification of the rib joints and displacement of internal organs. But this is not the only danger of spondylitis
.
In the long term, it leads to complications in the heart, liver, kidneys and nervous system. Both old and young are susceptible to the disease. The pathology is often observed in adolescents over the age of 15 years. Fortunately, spondylitis
is not very widespread - no more than 0.6% of people suffer from it.
But if the disease already exists, is it possible to avoid spinal deformation and worsening the condition? Let's understand the nature of spondylitis
.
Types of spondylitis
Depending on the causes of the disease, pathology is usually divided into:
- Specific spondylitis
. This category includes diseases caused by a specific infectious pathogen. As a rule, these are spondylitis secondary to tuberculosis, syphilis, gonorrhea, typhoid fever, actinomycosis, brucellosis and other diseases. - Nonspecific spondylitis
.
This group of spondylitis occurs as a result of nonspecific infections. They are caused by microorganisms that are already found in the human body or are considered only conditionally pathogenic. Therefore, spondylitis
begins only after a “trigger” has been triggered - for example, injury, stress, hypothermia, hormonal imbalance.
Based on the location of the inflammatory focus, the following are distinguished:
- cervical spondylitis;
- thoracic spondylitis;
- spondylitis of the lumbar spine
.
of spondylitis also varies
- it can progress slowly, with exacerbations, quickly and rapidly (within several hours - which is typical for septic spondylitis).
Tuberculous spondylitis
Tuberculous spondylitis
(Pott's disease) most often affects the thoracic region in children and adolescents because their musculoskeletal system is still developing. Bacteria (Koch's bacillus) penetrate the vertebral body and, releasing toxins, provoke a focal necrotic process in it. Over time, tuberculous spondylitis spreads to neighboring vertebrae, leading to the formation of edema and abscesses. Patients complain of increased fatigue, insomnia, and back pain.
Tuberculous spondylitis
may debut several months or even years after infection with tuberculosis - after stress, injury or decreased immunity.
The disease is characterized by a severe course, since it affects large areas at once. Also, the difficulty of treating tuberculous spondylitis
lies in the resistance of the pathogen to most antibiotics.
Aseptic spondylitis
Kümmel-Verneuil disease, also known as aseptic spondylitis
, begins with a back injury. Usually, several months or years pass between the injury and the onset of spondylitis - often patients even forget about the initial incident. However, after the appearance of necrotic lesions in the spine, their condition begins to worsen. Due to improperly distributed load, the risk of compression fractures of the spine and inflammatory processes in the nerve roots increases.
First of all, aseptic spondylitis affects the thoracic region, in rare cases it declares itself as lumbar spondylitis
. Young men under the age of 40-45 are most susceptible to it.
Ankylosing spondylitis
Ankylosing spondylitis
also known as ankylosing spondylitis. In this disease, the body's immune cells begin to attack its own bone and cartilage tissue, destroying the structure of the joint and the ligaments surrounding it. The body tries to compensate for the loss of tissue by replacing it with bone growths (osteophytes). Ultimately, this leads to ossification and complete immobility of the affected joint.
In addition to the loss of normal motor abilities of patients with ankylosing spondylitis
I am bothered by excruciating pains that do not subside even at night. When fusion of the vertebrae in the thoracic region occurs, difficulty breathing is observed, which can cause congestion in the lungs. Symptoms of the disease intensify after physical activity or prolonged rest.
90% of patients with ankylosing spondylitis
are made up of men.
The disease makes its debut between the ages of 15 and 40 years, and early onset often precedes its unfavorable course. Among patients with ankylosing spondylitis, lumbar spondylitis
.
Clinical observation
The course of the disease of a patient who was treated in the neurological department of the State Budgetary Healthcare Institution "SGB No. 4" (Samara) from August 28, 2019 to September 27, 2019 was analyzed.
Patient R., 56 years old, pensioner, was admitted urgently to the neurological department due to severe pain in the lower thoracic and lumbar spine, weakness in the legs, and impaired mobility.
From the anamnesis
it is known that the patient suffers from urolithiasis; in 2021, he underwent surgical treatment for a malignant neoplasm of the bladder and polychemotherapy. In 2011, an electrical pacemaker (pacemaker) was implanted due to sick sinus syndrome. Due to pain in the projection of the right kidney, on June 1, 2019, he was urgently hospitalized in the urology department, where on June 3, 2019, contact lithotripsy was performed for a stone in the lower third of the right ureter. The condition was complicated by secondary obstructive pyelonephritis. A stent was installed in the right kidney on June 7, 2019. The postoperative period was complicated by urosepsis. From June 10, 2019, a rise in temperature to 40°C and chills were noted, the patient was transferred to the intensive care unit. Antibacterial therapy was carried out with ceftriaxone and ciprofloxacin. The stent was removed on June 17, 2019.
While being treated in the urology department, he began to notice pain in the lower thoracic and lumbar spine. He was examined by a neurologist, an X-ray was performed, then a computed tomography (CT) scan of the lumbar spine was performed. Conclusion
from 06/21/2019: CT signs of intervertebral osteochondrosis of the lumbar spine. L4 disc protrusion. Spondyloarthrosis. Spondylosis.
The nonsteroidal anti-inflammatory drug (NSAID) lornoxicam 8 mg twice a day for 7 days was recommended for treatment. With improvement in laboratory parameters of blood and urine tests, the patient was discharged on June 25, 2019 with recommendations: dynamic observation by a urologist, further intake of ciprofloxacin orally at a dose of 500 mg 2 times/day for 7 days, drinking plenty of fluids.
At home, he again noted episodes of chills, was bothered by general weakness, shortness of breath appeared with little physical exertion, and back pain persisted. Due to changes in the electrocardiogram, on June 27, 2019, the patient was sent to the regional cardiology clinic and hospitalized in the department for the treatment of complex arrhythmias and cardiac pacing for revision of the stimulating system. Transesophageal echocardiography revealed large vegetation on the pacemaker electrode and grade II–III tricuspid valve insufficiency. Blood cultures for sterility were performed three times (06/29, 06/30, 07/01) from both hands. Raoultella ornithinolytica isolated
, sensitive to antibiotics, namely to an antimicrobial drug from the fluoroquinolone group - levofloxacin.
07/11/2019 surgical treatment was performed - tricuspid valve repair
according to De Vega, removal of cardiac electrodes, implantation of the Effecta DR pacemaker with epicardial fascia electrodes.
During a bacteriological analysis of vegetation from an electrode (07/15/2019), the microorganism Klebsiella oxytoca
, and sensitivity to an antibiotic from the group of fluoroquinolones (levofloxacin) was determined. Antibacterial therapy was carried out: parenteral vancomycin 1.0 g 2 times/day for 10 days; daptomycin parenterally 500 mg 1 time/day for 2 weeks, levofloxacin parenterally 500 mg 2 times/day for 10 days.
After surgical treatment, along with antibiotic therapy, the patient noted an improvement in his condition in the form of a decrease in weakness, normalization of body temperature, but with persistence of pain in the back. He was re-examined by a neurologist, it was recommended: diclofenac sodium 25 mg/ml, 3.0 ml 1 time/day for 7–10 days, a lidocaine patch applied locally to the lumbar spine. Discharged on July 20, 2019.
Over the next month, intense back pain was noted that was not relieved by analgesics, and weakness in the legs began on August 20, 2019. Hospitalized in the neurological department
08/28/2019. Upon admission, there was severe pain in the lower thoracic and lumbar spine, assessed on a visual analogue scale (VAS) at 8–9 points out of 10, and was delivered on a gurney.
Neurological status:
the patient is conscious, meningeal signs are negative, cranial nerves are without focal pathology. Superficial and deep sensitivity is preserved. Lower paraparesis up to 3.0–3.5 points. Tendon reflexes of the lower extremities are animated, positive pathological Babinski reflex on both sides. Palpation of the spinous processes of the vertebrae reveals sharp pain at the level from Th10 to L5, tension in the paravertebral muscles in the thoracic and lumbar regions, and the range of motion in the lumbar spine is significantly limited. The functions of the pelvic organs are not impaired.
In the general blood test: unexpressed leukocytosis up to 10.6 × 109/l with a band shift up to 6%, increased ESR up to 28 mm/h. In a general urine test: an increased content of leukocytes up to 15–20 per field of view in the absence of protein and other changes. Biochemical blood test without deviations from the norm. On admission, C-reactive protein (CRP) was not detected.
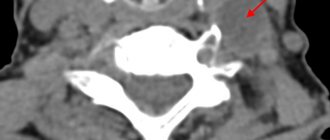
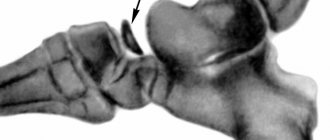
Figure 1 shows a radiograph of the thoracic spine (lateral view) obtained upon admission. To clarify the diagnosis, a CT scan of the thoracic spine was performed (Fig. 2).
To exclude tuberculous etiology of the disease, Diaskintest was performed with a negative result. Examination by a phthisio-osteologist: there is no evidence of extrapulmonary tuberculosis.
Blood samples were taken from both hands three times to ensure sterility: no growth of microorganisms was detected.
Thus, the patient was given a clinical diagnosis
: Subacute nonspecific spondylitis Th12/L1, lower paraparesis with moderate limitations of motor functions. Pain syndrome.
Taking into account previous antibiotic therapy, in agreement with the neurosurgeon and clinical pharmacologist, the patient was prescribed: parenteral lincomycin 600 mg twice a day for 4 weeks, rifampicin 450 mg/day for a month, angioprotector diosmin 600 mg/day, thioctic acid 600 mg /day, opioid analgesic - tramadol hydrochloride 50 mg up to 2 times / day, it is recommended to wear a rigid thoracolumbar corset.
Clinically, positive dynamics were noted in the form of a decrease in pain, VAS score - 2 points, strength in the lower extremities increased to 4 points, the patient moves independently around the department. Laboratory parameters returned to normal. The patient was discharged on the 31st day with recommendations to continue antibiotic therapy: lincomycin 500 mg twice a day for 4 weeks, rifampicin 450 mg/day for a month, dynamic observation by a neurologist and neurosurgeon for 6 months. Conclusion according to CT data (09.19.2019): signs of spondylodiscitis Th12/L1, pathological compression fracture of the Th12 body.
According to the literature, CT/MRI monitoring of treatment effectiveness is impractical due to the discrepancy between clinical improvement and neuroimaging picture, which is what we observed. CT/MRI monitoring is indicated if therapy is ineffective, there is no clinical improvement, or there are continuing negative dynamics in laboratory parameters [3, 6].
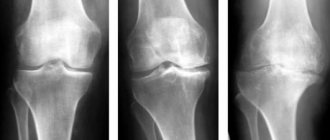
Dynamic monitoring was also carried out after a course of outpatient treatment. In October 2021, surgical treatment was performed - percutaneous vertebroplasty of the Th12 vertebra under radiation control
. The X-ray dated October 28, 2019 is shown in Figure 3. There was an improvement in well-being, a decrease in pain, and the patient could move independently. Neurological status: no paresis.
Causes of spondylitis
Spondylitis of the spine
can be called a “disease of neglected infections” - most often it occurs as a complication due to late access to a doctor for the treatment of infectious diseases.
It can be caused by both a chronic infection circulating in the body (for example, streptococcus, Staphylococcus aureus, actinomycosis) and an acute infectious disease (for example, typhus, gonorrhea and even tonsillitis or pyoderma). The following factors can provoke the development of spondylitis against the background of an underlying infection:
- general suppression of the immune system due to an unhealthy lifestyle or bad habits;
- hormonal changes in the body or endocrine disorders;
- psycho-emotional or physical stress;
- spinal injuries;
- the presence of a focus of chronic infection;
- severe hypothermia or overheating;
- long-term use of medications (especially glucocorticoids and cytostatics);
- genetic predisposition (indicative if there have already been cases of spondylitis in the family).
Diagnostics
Detection of the disease at an early stage is possible only through X-ray examinations. Sometimes this is not enough and a comprehensive examination may be required: in some cases, this is the only way to make a correct diagnosis.
When performing radiography, it is very important that the pictures are taken in lateral and standard projections. Osteophytes, if any, can definitely be seen in such images. In addition, it is necessary to visualize which parts of the spine are susceptible to pathology.
If the picture is not too clear, then a computed tomography scan is prescribed in addition. Timely and correct diagnosis allows you to identify the disease at an early stage and begin adequate treatment.
Symptoms of spondylitis
Symptoms of spondylitis begin and intensify as bone density in the spine decreases. Therefore, at the initial stage (when only one vertebra is affected), the clinical picture of the disease may be blurry. The first signs of the disease include:
- moderate pain in the thoracic or sacral spine, which bothers the patient only periodically;
- general decrease in endurance;
- characteristic poses designed to reduce the load on the affected area.
Later, depending on the location and type of spondylitis, other alarming symptoms appear:
- feeling of suffocation and shortness of breath, difficulty taking deep breaths, pain in the sternum;
- spread of pain to other parts of the spine and its intensification;
- pain persists during rest;
- characteristic lumbago;
- instability of blood pressure, its sharp jumps;
- redness and increased temperature of the skin over the site of inflammation;
- swelling of the affected areas;
- abdominal pain (in particular, with lumbar spondylitis);
- deterioration in sleep quality;
- “gentle” gait;
- mood problems - depression, irritability, emotional “reactivity”.
At the last stage, irreversible changes appear:
- kyphosis caused by spinal deformation (as a rule, the natural curves of the back are disrupted, and the stomach protrudes forward);
- characteristic hump and shortening of the spinal column;
- immobility, stiffness of the back, which is especially noticeable when turning the body;
- numbness of the limbs and loss of ability to self-care;
- paralysis;
- disruption of the pelvic organs (including problems with the toilet);
- fistula formation is possible.
With the rapid progression of purulent spondylitis, symptoms develop within several hours and begin with acute pain and an increase in temperature to 40 degrees or more. There are also symptoms of acute intoxication - dizziness, severe weakness.
Mechanism of disease development
The leading role in the development of this disease is played by a complex of inflammatory changes leading to necrosis (necrosis) of the bone tissue of the vertebral body. This condition entails disruption of the joints and ligaments. As a result, mobility is significantly reduced and deformation of the spinal column develops.
As the pathological process develops, the affected vertebrae begin to acquire a wedge-shaped shape. Ultimately, this leads to compression (displacement and deformation) of the spinal cord substance and the development of compression fractures.
Treatment of spondylitis
Treatment of spondylitis
consists in the complex use of medications, physiotherapy, diet therapy and therapeutic exercises. Surgical interventions to relieve symptoms are performed quite rarely - mainly for tuberculous and ankylosing spondylitis.
It is necessary to begin treatment for spondylitis when the first, still mildly expressed, pain in the sternum, neck or sacrum appears. The treatment strategy is selected taking into account the nature of the disease, the patient’s age, and the presence of neurological problems associated with compression of the spinal roots.
With proper and timely treatment, it is possible to avoid a reduction in life expectancy in patients with spondylitis.
Exercise therapy for spondylitis
Therapeutic exercises for spinal spondylitis are performed only in a state of remission, in the absence of the slightest symptoms of inflammation. With regular exercise, exercise therapy helps eliminate stiffness and spasms in the back, and increases the overall endurance of the muscles and ligaments that form the supporting corset for the spine. Also, therapeutic exercises help to unblock compressed nerve roots and improve blood circulation in the tissues of the spine. A set of exercise therapy exercises for spondylitis is compiled individually, after a complete examination of the patient. The fact is that even minor injuries with this disease can cause a compression fracture of the spine.
Diet for spondylitis
For patients with spinal spondylitis
It is recommended to avoid foods rich in starch and other simple carbohydrates, such as:
- potato;
- fast food;
- confectionery and baked goods, especially factory-made ones;
- White bread;
- sugar and carbonated drinks;
- coffee “3 in 1”;
- alcohol.
Sausages and refined fats (mayonnaise, margarine) are also extremely undesirable.
To combat anemia and inflammation, patients are advised to eat foods high in:
- iron (buckwheat, greens, pomegranate, liver);
- antioxidants - vitamins E, C, flavonoids (fruits, primarily red, berries);
- polyunsaturated fatty acids (sea fish, nuts, unrefined olive and flaxseed oil);
- calcium and boron (dairy products, beets, green peas, apricots).
To relieve intoxication and normal metabolism, you should drink at least 2 liters of water per day.
Physiotherapy
Physiotherapy plays a supporting role in the treatment of spondylitis
.
First of all, it is aimed at relieving the inflammatory process and cold swelling in the spine, healing necrotic lesions and fistulas. For spinal spondylitis,
the following methods are recommended:
- electrophoresis;
- laser therapy;
- ultrasound therapy;
- shock wave therapy;
- phonophoresis;
- balneotherapy (especially medicinal baths);
- massage (including hydromassage) and manual therapy;
- passive and active kinesiotherapy;
- high-tone bioresonance therapy;
- physiotherapy.
Medicinal phono- or electrophoresis with glucocorticosteroids, as well as magnetic therapy are used during exacerbation of spondylitis. Other methods are priority during the period of remission.
Drugs for spondylitis
Drug therapy is the main treatment for spondylitis. In addition to antibiotics to eliminate the underlying disease, nonsteroidal anti-inflammatory drugs (NSAIDs) are considered the leading drugs. They allow you to relieve the symptoms of inflammation, remove swelling and completely or partially eliminate pain. NSAIDs cannot be taken constantly - they are prescribed only during exacerbations, since they negatively affect the gastrointestinal mucosa.
For severe inflammation and extensive necrosis of spinal tissue, glucocorticoid steroids are prescribed. This group of drugs is also intended for short-term symptomatic use, since long-term use can only worsen spondylitis.
In case of infectious intoxication of the body, drip intravenous administration of solutions to remove toxins is indicated. To protect healthy tissues and improve metabolic processes, B vitamins, blood microcirculation correctors, and vasoprotectors are used.
Due to the fact that the affected spine cannot perform its supporting function in full, the back muscles take on part of the load. Constant overexertion causes severe spasms; to relieve them, patients are prescribed antispasmodics and muscle relaxants.
The only group of medications that really helps restore damaged tissues are chondroprotectors.
Chondroprotective agents for the treatment of spondylitis help accelerate regeneration processes in the spine, protect healthy cells from the adverse effects of toxins and enzymes, and also significantly slow down the progression of the disease. They are most effective in cases of slow or worsening disease, as well as in the recovery period after treatment of septic spondylitis. For spondylitis of various etiologies, doctors recommend a course of Artracam. It is enough to take this chondroprotector in a sachet for 2-4 months a year to prevent or slow down the transition of spondylitis to new joints. Artracam reduces pain, helps prolong remission, and most importantly, allows you to less frequently resort to taking anti-inflammatory drugs that are unsafe for health. Being a natural product based on glucosamine, Artracam has no contraindications for use at any age. And may spondylitis spare your joints!