15.01.2021
The human body begins its countdown at approximately 20 years of age. By this time, a person has managed to “tamper” with his health enough for chronic diseases to appear or some pathological processes to accelerate.
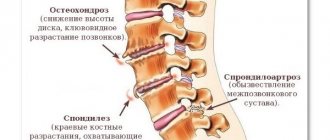
Degenerative changes in the intervertebral discs are changes that change the height of the intervertebral discs and the mechanics of the entire spinal column, resulting in back pain and dysfunction of the musculoskeletal system.
How and why does pathology develop?
Degenerative changes are considered widespread if clearly defined symptoms with constant pain appear. The process, unfortunately, is irreversible, the condition will worsen or the disease will become chronic .
The spinal column is constantly exposed to stress, most of which falls on the lumbar region. Due to the influence of external factors, deformation of the intervertebral discs begins.
Pathogenesis develops in stages:
- First of all, the nutrition of cartilage tissue deteriorates . You should know that the vertebra does not receive nutrients directly, since it does not have blood vessels. Due to the emerging deviations, the soft tissues of the spine lose their elasticity and begin to collapse.
- Then dystrophic processes appear . The cartilage tissue becomes thin and weakens. These changes reduce the height of the vertebrae.
- A continuation of dystrophy is the occurrence of protrusions or the formation of hernias . In places where the discs are displaced, the fibrous membrane begins to collapse, which causes rupture of the ring that holds the fibrous core. The leakage of gelatinous fluid forms a hernia. Naturally, pinched roots and disturbances in the proportions of the spine occur.
- The body responds to the pathogenic process with abnormal activity of the immune system . The synthesis of prostaglandins, which control inflammatory processes, is enhanced. They instantly increase blood circulation, which causes swelling around the spine. Then pain and stiffness occurs in the lumbar region.
Dystrophic changes in the spine occur due to malnutrition of cartilage tissue
Degenerative-dystrophic changes occur slowly, which contributes to the development of chronic diseases and the manifestation of complications. Damage to cartilage tissue often causes osteochondrosis, radiculitis and other pathologies of the spine.
Prevention
Degenerative changes in the lumbar region are easier to prevent than to treat, so doctors insist on early prevention of spinal pathologies.
Physical activity will help keep your spine healthy.
In order not to become hostage to dystrophic changes, you need to follow a few simple rules:
- monitor body weight and avoid excess weight;
- give the body a daily feasible load, and if it is impossible to do gymnastics, at least take walks for 20–30 minutes a day;
- swim more often, since during swimming all muscle groups are involved, and there is no load on the spine in the water;
- When working with heavy objects, follow safety precautions and use safety belts;
- avoid increased stress on the back, for example, in sports;
- If you have back pain, consult a doctor in a timely manner;
- patients with sedentary work once every six months (or more often - on the doctor’s recommendation) undergo courses of massage and manual therapy;
- avoid hypothermia;
- Eat a balanced diet and include enough foods containing calcium in your diet.
During the cold season, it is necessary to protect yourself from falls in many places on the road. Women are recommended to take hormonal medications during menopause, since when hormone levels change, the condition of bone tissue sharply worsens. And it is also necessary to promptly treat all inflammatory diseases.
The causes of these disorders in the lumbar region
Pathological changes in the lumbar region occur due to a number of negative factors.
The main reasons can be identified:
- Inactive lifestyle. If there is no load on the lower back, this leads to weakening of the muscles. As a result, the ability to withstand even small loads disappears.
- Mechanical and birth injuries.
- Professional sports with exorbitant loads. Destructive changes often begin due to lifting excessive weights and sudden movements without warming up the muscles.
- Hypothermia of the body.
- Inflammatory processes in the spine (arthritis, ankylosing spondylitis).
- Aging of the body. The necessary components are washed out from cartilage and bone tissues.
- Unhealthy diet. In this case, obesity is often observed, which negatively affects the spine.
There are many other factors that influence the appearance of dystrophic changes. In addition, the spinal column can be affected by several triggers. It follows from this that it is almost impossible to independently identify the cause.
Possible consequences
If you ignore the development of degenerative changes, then serious complications may arise in the lumbar area:
- Hernia formation.
- Osteochondropathy.
- Loss of motor ability and sensation in the legs.
- Paralysis of the lower extremities.
- Difficulty with bowel movements and urination.
- Sexual dysfunction disorder.
Consequences of degenerative-dystrophic changes in the spine
To prevent this from happening, timely and well-chosen treatment is necessary that can stop the destruction of intervertebral discs.
Stages, types of disc protrusion in the lower back
There is a classification of lumbar protrusions according to stages of development, which makes it possible to determine the severity of the clinical process.
- The first stage (mild) is characterized by the smallest, barely noticeable protrusion of the disc, which not every specialist can detect, even with MRI images. Dimensions – 0.1-1 mm.
- The second stage (moderate) - the bulge increases, making it easier to diagnose using special imaging tools. The size of protrusion in stage 2 is 1-3 mm.
- The third stage (severe) - at this stage the displacement is already quite large, clearly visualized behind the contours of the vertebrae. Instrumental examination shows a formation of 3-6 mm, but still no signs of rupture of the outer part of the fibrous ring.
The last stage (3rd stage) is borderline with extrusion. And from this it follows that at any moment, against the background of strong sagging of the pulpous mass, the fragile fibrous ring may not be able to withstand it and finally burst. Then part of the nucleus will crawl out through the formed hole, which means a hernia will appear, in the true sense of the word from a medical point of view. However, we will not go beyond the scope of the article; let’s return to lumbar protrusion. Let us briefly consider its varieties depending on the direction and position of the resulting bulge.
| Variety | Characteristic |
| Dorsal | It protrudes from the vertebrae posteriorly, in the direction opposite to the spinal canal. This form is rare and clinically the calmest. |
| Lateral | Protrudes from the right or left side of the vertebra, in the projection of the foraminal opening. Common type. Often comes into contact with the nerve processes emerging from the intervertebral foramen. |
| Median | Prolapse “looks” strictly at the center of the spinal canal, where the nerve bundle of the spinal cord – the cauda equina – is concentrated. Worst location ever. |
| Circular | Uniform or uneven defect along the entire circumference of the disc. This is another dangerous form, and it is also the most common (80%). |
Symptoms and diagnostic methods
Unfortunately, a person is unaware of the disease until low back pain appears , which limits the ability to work. The degenerative process does not manifest itself; symptoms indicate its complications.
You should definitely visit a neurologist if the following sensations appear::
- Dull or stabbing pain in the lumbar region.
- Pain after being in an uncomfortable position for a long time.
- Painful sensations after physical activity.
- The appearance of weakness in the lower extremities.
- Difficulty bending and turning.
- Stiffness of the spine in the morning.
- Constipation and problems with urination.
- Cold skin in the lower back area.
- The symmetry of the body is broken.
- Swelling and redness of the skin in the lower spine.
Symptoms intensify depending on the stage of development of the pathology:
| Stage 1 | Symptoms appear extremely rarely. Sometimes a dull pain appears after exercise, but usually this is attributed to a feeling of fatigue. |
| Stage 2 | Symptoms are already occurring. It can be difficult to bend, sometimes your back gets shot. Compressed nerve endings cause tingling in the pelvic area. |
| Stage 3 | Considered spicy. Blood vessels are damaged, metabolism in the lumbar muscles is disrupted, and ischemia begins to develop. The pain intensifies, the legs become numb and cramps occur. |
| Stage 4 | Paralysis of the legs may occur because the spinal cord is already deformed. |
Symptoms appear most clearly during an exacerbation . When degenerative processes take a chronic form, the signs of the disease are characterized by muted discomfort.
Symptoms at the initial stages of development of degenerative disorders in the spine do not appear. It is very difficult to determine the degenerative process in the initial stage of development. It is usually only discovered during a routine medical examination. But if a visit to the clinic is caused by lower back pain, then the disease is already progressing.
It is important to detect the problem before the first complications appear. To do this, various diagnostic methods are used, covering a wide range of stimuli. But initially an examination is carried out by a neurologist. Then the doctor will prescribe additional tests to clarify the diagnosis.
The following procedures are usually performed : radiography, computed tomography, MRI.
X-ray is the most accessible method, but not very informative. It detects the disease at a late stage. and MRI are higher priority. They allow you to more accurately determine the location, as well as the degree of damage.
MRI most reliably indicates the presence of degenerative changes.
MRI results about the presence of dystrophic processes:
- The disk is destroyed more than 50%.
- Disc dehydration. It looks darker on MRI.
- Accurately determines the presence of protrusions and hernias.
- Detects erosion of the cartilage plate through which the cells inside the disc receive nutrition.
Sometimes it is necessary to conduct electroneuromyography to understand where and how the nerve is affected. Naturally, blood is given for analysis to detect endocrine disorders and possible infections.
Video: “Degenerative-dystrophic changes in the spine: lecture”
Recovery after surgery
After a minimally invasive simple session, the patient is activated after 2-3 hours. Most of those operated on notice noticeable improvements within the first hours after minimally invasive surgery. Perhaps, immediately after activation, he will be allowed to go home on his own. But in order to avoid postoperative complications, which are not excluded even after percutaneous (the most gentle) surgery, the following are prescribed:
- antibiotic therapy (against infections and suppurations);
- taking vascular medications (against limb thrombosis, thromboembolism);
- a calm physical regimen, especially gentle on the lower back during the recovery period;
- special physical therapy for good restoration of the operated area, muscle strengthening, and prevention of relapses;
- wearing a support corset during rehabilitation;
- ban on lifting weights, lifelong refusal from heavy sports.
In total, rehabilitation measures take 2 months. But this does not mean that during these 2 months a person will be limited from walking, going to work, doing household chores, etc. No, with a successful intervention, patients even go to work within 3-5 days. However, non-compliance with specific rehabilitation and lifelong regimens, which the doctor thoroughly informs about upon discharge, is associated with high risks of postoperative complications. The first among them is the rapid resumption and more progressive course of protrusion.
Treatment
Did you know that...
Next fact
First, conservative therapy is carried out: various medications for pain relief, warming ointments, therapeutic exercises, massage and physiotherapeutic procedures. If these methods do not help, then a decision is made on surgical intervention. .
Drugs
First of all, it is necessary to relieve the pain syndrome, which will allow the person to move normally. For this purpose, painkillers (Ketanov, Ketonal) and anti-inflammatory drugs (Movalis, Diclofenac) are prescribed. These medications are used topically, orally, and by injection.
To relax the lumbar muscles, muscle relaxants (Mydocalm, Sirdalud) are used. They are used intermittently due to weakening muscles.
Chondroprotectors are also used to help speed up the regeneration of cartilage and joints.
Treatment with drugs gives a positive effect, but one should not forget about adverse reactions, since drugs often disrupt the functioning of the gastrointestinal tract.
Surgical intervention
Typically, conservative treatment improves the patient's condition. Surgery is necessary if the pathology continues to progress and drug therapy is powerless . The surgeon installs special devices to support the lumbar spine. This relieves pressure and prevents further deformation of the intervertebral discs in the lumbar region.
Exercise therapy
Therapeutic exercises are necessary both during treatment and during the rehabilitation period . Physical exercises are indicated for any manifestations of degenerative-dystrophic changes in the lumbar region. Naturally, the causes, severity of the process and the main symptoms of the disease should be taken into account.
In the acute phase of the disease, exercise therapy, of course, is not performed . First, you need to achieve pain reduction using other methods: absolute rest, NSAIDs, blockades, local cooling and other procedures.
For intense manifestations, low-amplitude and static exercises are recommended, performed very carefully and slowly. During the rehabilitation period, dynamic complexes are preferable.
In the future, the complexes become more complicated, and exercises with weights are added.
Massage and physiotherapy
Massage and other physical procedures are allowed only during the period of remission of the disease. Carrying out this procedure for dystrophic changes in the lumbar region causes controversy in the medical community. Mechanical impact on the discs also harms the healthy spine. Massage can be allowed if the soft tissues are massaged by an experienced specialist and in the initial stage of the disease.
Massage is prohibited during the acute period , since manipulation causes blood flow, and this provokes increased inflammation and swelling.
During remission, when there is no inflammation and acute pain, physiotherapy is also used. Electrophoresis, acupuncture and magnetic therapy speed up recovery. Manual therapy will restore the normal position of the vertebrae.
Self-treatment at home is best avoided. Without knowing the cause and exact diagnosis of the disease that caused dystrophic changes in the lumbar region, you can only harm your health.
Prevention
To prevent degenerative-dystrophic changes, much effort is not required. But even simple preventive measures will help maintain mobility and health. The aging of cartilage and bones cannot be stopped, but everyone has the power to slow down the degeneration of any part of the spine.
What is needed for this:
- It is necessary to strengthen the back muscles. To develop a muscular corset, strength exercises are necessary, and swimming will also be beneficial.
- You always need to be active. Lack of movement leads to muscle atrophy and loss of ligament elasticity. To keep your back healthy, you just need to do daily exercises.
- It is advisable to avoid excessive physical activity.
- You should pay attention to your posture; your back should always be straight.
- It is better to sleep on an orthopedic mattress, which allows you to fully relax.
Compliance with these rules will prevent degenerative changes and prolong activity into old age.
Operation for protrusion
Let us recall that protrusion is the initial form of herniation, when the anatomical integrity of the outer sphere of the fibrous ring is preserved, due to which the nucleus pulposus is still located in the disc. Only such a picture of the disease allows the use of puncture methods of plastic disc surgery. It is advisable to recommend nucleoplasty to a person with a protrusion of the lumbar/lumbosacral location only under the following circumstances:
- ineffectiveness of non-surgical treatment for 3-6 weeks;
- frequent exacerbations of painful symptoms;
- dysfunction of the nerves of the equine ganglion;
- chronic reflex and radicular syndrome;
- rapidly progressing dynamics of protrusion development.
Puncture nucleoplasty is aimed at reducing the pressure inside the intervertebral disc, which facilitates the return of the latter to its normal shape. The effect of reducing intradiscal pressure and retracting deformation is ensured by direct impact on the core (with the goal of its partial destruction) by a certain physical factor:
- cold plasma (cold plasma plastic);
- laser (laser vaporization);
- electromagnetic waves (radiofrequency ablation);
- a pressure jet of isotonic liquid (outdated tactics, hydroplasty).
At their core, all methods of influence “work” and are carried out according to the same principle. They are also approximately equal in effectiveness - the success rate of the procedures is approximately 80%. Access to the intervertebral disc is carried out from the back percutaneously (through a puncture puncture). Anesthesia is used mainly of a local type, but in some situations general anesthesia or epidural anesthesia is not excluded. The intervention is carried out on an empty stomach, before which the patient is given a cleansing enema. The procedure is carried out in the department of minimally invasive neurosurgery, equipped with an intraoperative X-ray machine. Session duration is 15-30 minutes. Let's consider all stages of nucleoplasty.
- The patient is placed on the operating table. The classic position is on your side, with your legs tucked towards your stomach.
- The skin of the lumbar region is widely treated with antiseptics. Anesthesia is performed.
- Under X-ray control, in a safe interval, the surgeon makes a puncture (2-5 mm) with a puncture needle inserted into the disc at the required distance. Usually to the center of the core.
- An electrode is installed into the working cannula of the needle, through which the “destruction agent” of the gelatinous substance will be supplied.
- By rotating and translational movements of the electrode, emitting, for example, pulses of laser radiation or a flow of low-temperature plasma, the jelly-like component in the disk is partially evaporated.
- The denucleation performed ensures inverse retraction of the pulpous mass that has shifted to the periphery of the ring during the course of the disease. The configuration of the lumbar disc is restored, and the pinched nerve root is eliminated.
- At the end of the operation, thin working instruments are removed, and an antiseptic patch is applied to the puncture. Usually such a tiny wound does not require stitches.
During the procedure.
If the protrusion is not confirmed by MRI, and a rupture of the fibrous part of the intervertebral lining is diagnosed, the significance of nucleoplasty is completely annulled. The operation of choice for already formed lumbar hernias is microdiscectomy or endoscopy.
Separately, it is worth highlighting the fact that elderly patients (after 50-55 years) do not undergo puncture surgery on lumbar discs. Experts explain this by the fact that, due to age-related aging, the lumbar intervertebral discs at this age are too severely dehydrated. This fact indicates the intractability of the unacceptably dehydrated fibrous ring to reverse retraction in the protrusion zone when using any type of nucleoplasty. And, consequently, the ineffectiveness of such procedures in elderly patients.
Department of Traumatology and Orthopedics
article in PDF format
QUOTE LINK:
Chernyaev A.V., Slinyakov L.Yu., Khurtsilava N.D., SURGICAL TREATMENT OF DEGENERATIVE LESIONS OF THE LUMBAR SPINE: HISTORY, TRADITIONAL APPROACHES (LECTURE) // Department of Traumatology and Orthopedics. 2014.№ 3(11). p.19-25 https://elibrary.ru/item.asp?id=24343037
A. V. CHERNYAEV1, L. Y. SLINYAKOV1,2, N. D. KHURTSILAVA2
1City Clinical Hospital named after. S.P. Botkina, Moscow
2First Moscow State Medical University named after I.M. Sechenov, Moscow
Review lecture. The evolution of views on surgical treatment of degenerative lesions of the lumbar spine is covered - from the first attempts to remove intervertebral discs to modern decompressive and stabilizing operations using high-tech techniques.
Key words: osteochondrosis, instability of the spinal motion segment, discectomy, transpedicular fixation.
The evolution of views on the surgical treatment of osteochondrosis of the lumbar spine is directly related to the development of ideas about the etiopathogenesis of clinical manifestations.
The first description of lumbar ischialgic syndrome was given in 1764 by D. cortugno, but he did not connect the clinic with spinal pathology. The first autopsy description of a disc herniation was by Middelton. The first graphic representation of a disc herniation was proposed by Goldthwait G., who first identified disc rupture as a cause of lumbar pain.
At the same time, the first attempts were made to remove the so-called “chondromas” by laminectomy. “Chondromas” were discovered during operations for various diseases of the spinal cord, some of the operations were performed with the aim of transecting the roots to relieve pain. In 1934 Mixter w. and Barr I. substantiated the need for decompression of the spinal canal by removing a disc herniation from a laminectomy approach in 12 patients with a clinical picture of lumbar ischialgia syndrome. The first report on the removal of a herniated disc from a posterior approach in Russia was made in 1935 by I.S. Babchin. (Fig. 1).
Further development of posterior approach surgery is associated with the introduction of less invasive techniques (the term was introduced into the literature by hilderbrandt). The use of hemilaminectomy allowed for revision of two intervertebral discs. love j. proposed to remove disc herniation using interlaminar access. This method, with additions and modifications, has become widespread. In 1941 Dandy w. proposed to perform disc curettage in order to prevent relapses and create fibrous fusion between the vertebral bodies. Thus, posterior approach surgery in the first half of the 20th century consisted of the approach itself (laminectomy, hemilaminectomy) and discectomy. The undesirable consequences of such operations (primarily laminectomy), leading to a sharp decrease in the support ability of the spinal column, were not taken into account by surgeons. Rehabilitation after such surgical interventions was a complex and sometimes unsolvable problem. Many patients required repeated surgical interventions.
Attempts to stabilize the spinal column after decompression and discectomy from the posterior approach have been made since the late 20s by fixing the posterior structures with bone grafts (Meyerding, Kozlovsky, Moore, Sicard, etc. operations). Surgeons placed bone autografts of various shapes on the decorticated arches and spinous processes in the hope of developing bone fusion (Fig. 2). However, the number of unsatisfactory results associated with lysis and graft fractures, stress fractures of the vertebral arches remained at a high level.
Analyzing the long-term results of surgical treatment of hernias of the lumbar spine using a posterior approach, Yumashev G.S. (Fig. 3) and co-authors note unsatisfactory results in 29−57% of cases, and in 20% of cases patients required reoperation due to the development of recurrent hernias. The authors concluded that operations using a posterior approach (laminectomy, hemilaminectomy, facetectomy) are palliative and recommend their avoidance. According to Armstrong IR, out of 4,000 operations, excellent results were obtained in 62%, improvement in 17% and unsatisfactory results in 21% of cases. According to the observation of Romodanov A.D. and co-authors (1976), who analyzed the results of surgical treatment of 1200 patients, lumbar ischialgia syndrome remained in 50% of those operated on. Cloward R. notes failures of surgical treatment in 20−37% of cases.
Detailing the structure of the causes of unsatisfactory results of surgical treatment using a posterior approach, various authors cite the following factors: development of cicatricial adhesions (10.3−20%), unremoved hypertrophied ligamentum flavum (5−12.7%), recurrence of disc herniation (9 −57.9%), disc herniation of the adjacent segment (10−25.8%), instability of the operated segment (3−11.5%), errors during surgery (1−9.3%), persistent spinal canal stenosis ( 5−27.8%), infectious complications (1−5%).
A huge contribution to the development of surgery for degenerative lesions of the spine was made by domestic orthopedists and traumatologists - V.D. Chaklin, Ya.L. Tsivyan, G.S. Yumashev, A.A. Korzh. Their scientific research was devoted to the development of a new direction of osteochondrosis surgery for that time - discectomy from the anterior approach with anterior interbody fusion (Fig. 4). This method is pathogenetically substantiated and allows you to completely correct pathological relationships in the area of the disc-radicular conflict.
In 1882, Pirogov N.I. proposed extraperitoneal access to the abdominal aorta. This surgical approach became the basis for later approaches to the anterior spine. caperener (1932) carried out a theoretical substantiation of anterior spinal fusion, but the author noted that this type of operation is practically impossible. For the first time in the world, V.D. Chaklin developed and applied the technique of anterior spinal fusion. in 1931 (Fig. 5). Using the extraperitoneal approach according to Pirogov, he performed a wedge-shaped resection of the adjacent surfaces of the l5 and s1 vertebral bodies and wedging with an autologous bone graft. However, since the late 1930s, reports of anterior spinal fusion have been rare. The widespread introduction of the anterior spinal fusion method into domestic vertebral surgery is associated with the work of Tsivyan Ya.L., Osna A.I., Mitbreit I.M. Yumashev G.S. et al. introduced the technique of fenestrated spinal fusion from an anterior approach into clinical practice. The advantages of anterior spinal fusion include radical removal of the pathological focus (total discectomy), possible only through an anterior approach, reliable stabilization (arthrodesis) of the spinal column, prevention of osteochondrosis of healthy discs located above the stabilized segment, and unloading of the contents of the spinal canal from the effects of a degenerated disc. According to Yumashev G.S., anterior discectomy with spinal fusion was performed in 741 patients, with good results obtained in 80% of those operated on. Among the intra- and postoperative complications, the author notes injury to the great vessels, bleeding from the vertebral bodies, hematomas and wound suppuration, intestinal paresis, acute urinary retention, thromboembolic complications, pneumonia, as well as fractures and lysis of bone grafts. The data of foreign authors who developed anterior approaches do not differ fundamentally from those given above. Thus, despite the pathogenetic validity of anterior discectomy with spinal fusion, this technique is traumatic for the patient, technically difficult for the surgeon and requires long-term rehabilitation treatment (bed rest for 2.5-4 months, wearing a plaster corset for up to 8-10 months).
In parallel with the development of anterior approach surgery, the development of pathogenetically based posterior lumbar interbody fusion (PlIF - posterior lumbar interbody fusion) took place. The first report on this technique belongs to Briggs H. and hillaman jw Surgeons used fragments of the spinous process, which were inserted dorsoventrally into the interbody space. Thus, the principle of restoring the height of the interbody gap was put into practice. However, the interbody bone block rarely developed, and the analgesic effect of the operation differed little from that after hemilaminectomy, which was common at that time, with discectomy from the posterior approach. Similar operations were performed by cloward Rb (1952), using an autograft from the iliac crest. The results were also unsatisfactory. The technique has not received widespread practical application.
In the 70s, reports appeared about the use of ceramic, hydrocarbon and other implants instead of bone grafts to achieve a block between the bodies of adjacent vertebrae. implants were installed from an anterior or posterolateral approach. These operations were not widely used at that time due to the complexity of the installation and the long rehabilitation period.
the desire to minimize the trauma of surgery led to the emergence of microsurgical techniques. In 1963, Smith s. tested the method of chemonucleolysis using chymopapain, which has become widespread both abroad and in our country. However, a high percentage of complications (spondylitis, toxic effects of papain on the myocardium, allergic reactions) forced a change in view on the feasibility of this procedure. An analysis of the treatment of 94 patients with lumbar osteochondrosis showed that chemonucleolysis is not able to replace surgical treatment, and the use of this technique requires too complex selection of patients. Vetrile S.T., Kazmin A.I. and their students state that this procedure does not help achieve the spinal stabilization necessary for a good result, also increasing treatment time.
In 1976, Caspar W. introduced into the clinic the microsurgical discectomy he improved (based on the love j. technique). The effectiveness of this technique reaches 94%. The high percentage of positive results of microdiscectomy is due to the possibility of performing an adequate discectomy without destroying the posterior supporting complex of the spinal column.
Modern methods of surgical treatment of degenerative-dystrophic lesions of the lumbar spine are the result of the development and implementation of high-tech techniques. The classical principles of spinal canal decompression, laid down at the beginning of the 20th century, are being implemented in full, and the use of modern metal structures for various purposes is both a preventive and pathogenetic component of surgical techniques.
At the moment, several main directions of surgical treatment of osteochondrosis of the lumbar spine can be distinguished.
Decompressive and stabilizing surgeries, arthroplasty surgeries from the anterior approach
These techniques are used in patients with degenerative lesions of the lumbar spine, complicated by the development of a disc herniation with neurological symptoms, instability of the spinal motion segment, and narrowing of the spinal canal mainly due to the anterior structures. Indications also include grade 1 degenerative spondylolisthesis, when compression of neural structures is caused not only by protrusion of the intervertebral disc, but also by the superoposterior part of the overlying vertebra. All methods of performing anterior spinal fusion from the ventral approach (AlIF-anterior lumbar interbody fusion) are based on the method proposed by V.D. Chaklin. Currently, instead of bone grafts, various versions of cages are used (English: cage), hollow metal structures of various shapes (Fig. 6), filled with bone autograft during installation, which is aimed at creating a full-fledged bone block. Along with hollow cages filled with autologous bone before installation, implants made of various materials (carbon, tantalum) are used to increase the efficiency of installation, that is, to increase the likelihood of bone block formation.
Considering the high traumatic nature of the anterior approach and the high risk of intra- and postoperative complications, two new types of approaches using minimally invasive techniques have been introduced into practice since the early 90s. on the one hand, laparoscopic techniques have been developed. The use of laparoscopic techniques is limited due to the high cost of laparoscopic equipment and the need for skills to work with it. It should also be noted that intraoperative complications are often serious and irreparable from this approach and require a transition to the open classical approach.
On the other hand, the classic ventral approach was minimized in size and complemented by microsurgical techniques, the use of various retractor systems (mini-AlIF in foreign literature). The advantages of these methods include minimal tissue trauma, low blood loss, reduced operation time, and a reduced number of intra- and postoperative complications.
Since the beginning of the 80s, arthroplastic methods of surgical treatment have been introduced into practice - endoprosthetics of intervertebral discs (Fig. 7). The purpose of the operation is not only to relieve pain, restore the height of the interbody space, but also to preserve function. The main problem of this area of vertebral surgery is maintaining the stability of the endoprosthesis at the implant-bone interface.
Despite a large selection of implants (ProDisk, bristol and others) and their constant improvement, the problem of endoprosthesis instability has not been resolved.
Contraindications to operations performed through the ventral approach include spinal canal stenosis caused by posterior structures and sequestered disc herniations.
Puncture, endoscopic and laser techniques
This group of surgical methods includes puncture endoscopic decompression, laser puncture endoscopic decompression, and “automatic” percutaneous discectomy.
Indications for these methods are detected only in 10−15% of patients with clinical symptoms of lumbargia or radicular syndrome. The indication is verified disc protrusion without rupture of the annulus fibrosus according to computed tomography and magnetic resonance imaging and the absence of effect from conservative treatment within 6 weeks. In the presence of damage to the posterior longitudinal ligament, the effect of the operation is questionable; in the presence of a sequestered disc herniation, the techniques are contraindicated.
Contraindications also include: cauda equina syndrome, spinal stenosis, previous operations in this area, mental disability of the patient, deafness and blindness, intolerance to local anesthetics.
Complications (periradicular hematoma, bleeding, local aseptic epiduritis, etc.), according to materials from various authors, range from 2 to 15%. Positive results, according to Kotilainen e., were obtained in 64% of cases, only 57% of patients returned to work.
Thus, the technical complexity of this group of operations, narrow indications and a wide range of contraindications, the high risk of complications due to limited diagnostic and manipulation capabilities determine the limitations in the use of techniques.
Decompression and stabilization operations from the posterior approach
Surgical intervention from the posterior approach is currently the main and most common method of surgical treatment of lumbar intervertebral disc herniations.
modern vertebrology and surgery of degenerative diseases in particular received a fundamentally new direction of development with the advent of the transpedicular fixation method. In the development of the method, the most important place is given to Roycamille R. (1970), who developed and introduced pedicle fixation with plates into clinical practice. Subsequent developments and improvements by various companies led to the emergence of highly efficient designs.
Currently, all transpedicular fixators can be divided into rigid and dynamic (Fig. 8). The indication for the use of transpedicular fixation is instability of the spinal motion segment.
According to Yumashev G.S. and Furman M.E., instability of the spine should be understood as clinical and radiological syndrome of osteochondrosis, manifested in the functional failure of the spine under conditions of static-dynamic load and caused by pathological displacement of the vertebrae relative to each other in the horizontal plane.
Khvisyuk N.I., Korzh A.A. and Makovoz E.M. The term “spinal instability” includes the biomechanical inability of the spinal column to support itself, a violation of the physiological movements of the vertebrae relative to each other, and a symptom complex corresponding to these disturbances, the main manifestation of which is the dependence of the intensity of the pain syndrome on the magnitude of the load on the spinal column.
Bradford Ds (1985) in the concept of instability includes manifestations of traumatic lesions, congenital and acquired lesions of the axial skeleton, distinguishing acute and chronic forms.
It should be noted that there is currently no generally accepted definition of instability. Each author has his own concept of instability and classification, taking into account the etiology (abnormal, degenerative, post-traumatic, destructive), degree of compensation (compensated, subcompensated, decompensated).
Thus, it is most appropriate to understand instability of the lumbar spine in degenerative-dystrophic diseases as chronic degenerative instability - a condition in which it is impossible to maintain stable spatial relationships between the elements of the biomechanical chain of the spine under the influence of external loads.
from a practical point of view, the classification of degenerative instability of the lumbar spine proposed by Makirov S.K. is of greatest interest. and Kavalersky G.M. based on the results of mathematical modeling. The authors identify 3 types of instability in the spinal motion segment:
type 1 dislocation syndrome – characterized by a decrease in the height of the interbody space (i.e., intervertebral disc) from 10 to 30%; in this case, a slight “subluxation” (“functional block”) is observed in the facet joints;
dislocation syndrome type 2 (true instability) – there is a decrease in the height of the interbody space from 31 to 50%; the development of dynamic stenosis of the spinal canal is possible even in the absence of stenotic factors (disc herniation, hypertrophy of the ligamentous apparatus, osteophytes); Type 2A - stenotic factors are located in the anterior part of the spinal canal, type 2b - stenosis comes from the lateral and posterior parts of the canal.
dislocation syndrome type 3 – reduction in the height of the interbody space by more than 50%; this degree of degeneration of the intervertebral disc leads to the development of spondyloarthrosis, impaired mobility in the facet joints and creates conditions for the development of a fibrous block in the intervertebral space with further degeneration of bone tissue (progression of spondylosis).
The use of various transpedicular systems should be justified by the type of instability that has developed, that is, the stage of the pathological process in the spinal motion segment.
For type 1 dislocation syndrome, it is possible to use dynamic transpedicular systems (nonfusion technologies). The first such system was Dynesis (Fig. 9). The longitudinal metal rods were replaced with a stabilizing cord. the system made it possible to stabilize the affected segment while maintaining the physiological range of motion (neutralization of dyskinesia in combination with a controlled range of motion).
Another direction in the development of dynamic implants was the use of interspinous fixators (co ex, Diam). The advantage of these implants is ease of installation, unloading of the posterior parts of the intervertebral discs and facet joints (Fig. 10). the installation of these fixators is positioned not only as a way to eliminate instability, but also as a means of active prevention after removal of hernias using an interlaminar approach.
For dislocation syndrome types 2 and 3, the use of rigid transpedicular systems is indicated.
Access to the spinal canal is carried out through laminectomy, hemilaminectomy, interlaminar love or transligamentous, extended interlaminar access with arcotomy. After spinal canal decompression and discectomy, if necessary, stabilization is carried out using one of the following methods:
1. spinal fusion with autologous bone or cage in combination with bilateral transpedicular fixation (PlIF, spinal fusion 3600).
2. spinal fusion with a cage in combination with unilateral transpedicular fixation (spinal fusion 2700).
3. bilateral transpedicular fixation - in cases where discectomy is not required (spinal fusion 1800).
4. spinal fusion with a cage through a transforaminal approach in combination with transpedicular fixation (tlIF - transforaminal lumbar interbody fusion).
Modern transpedicular fixators create absolute stability in the operated segment, which allows for early activation of patients and the abandonment of external immobilization. Despite these positive aspects of using these fixators, there remains one important aspect that negatively affects the biomechanics of the spinal column. When using transpedicular clamps, the spinal motion segment is switched off from the single functional chain of the spinal column. As a result, compensatory hypermobility develops in the superior and inferior segments, which can ultimately lead to accelerated degeneration of the corresponding intervertebral discs and the development of instability in the segments adjacent to the operated segments, which in total may be an indication for repeated surgical intervention. Therefore, recently there have been reports of the installation of dynamic fixators above the rigid fixation system.
When assessing the results of surgical treatment using transpedicular fixators, the number of unsatisfactory results remains quite high, reaching 25%. One of the reasons for persistent pain in the lumbar region after surgery is the traumatic nature of the posterior approaches, caused by massive skeletonization of the arches and articular processes and prolonged traction of the musculofascial complex. The development of this idea led to the emergence of a minimally invasive technique for stabilizing the lumbar spine (Fig. 11).
Thus, the methodology for surgical treatment of degenerative lesions of the lumbar spine has evolved from a symptomatic approach to pathogenetic treatment with the introduction of high-tech surgical techniques.
Bibliography
1. Korzh A.A., Talyshinsky R.R., Khvisyuk N.I. Surgical approaches to the thoracic and lumbar vertebrae. M., Medicine, 1968. 204 p.
2. Mitbreit I.M. spondylolisthesis. M.: Medgiz, 1978. 271 p. 3. Mikhailovsky M.V. Stages of development of vertebral surgery: historical excursus // Spinal surgery. 2004. No1. With. 10−24.
4. Musalatov Kh.A., Aganesov A.G. Surgical rehabilitation of radicular syndrome in osteochondrosis of the lumbar spine. (Microsurgical and puncture discectomy). M.: Medicine, 1998. 88 p.
5. Osna A.I. Surgical treatment of lumbar osteochondrosis. M.: Medicine, 1965. 192 p.
6. Khvisyuk N.I. Instability of the lumbar spine: Dis. ...Dr. med. Sci. Kharkov, 1977. 472 p.
7. Tsivyan Ya.L. Spine surgery. Novosibirsk: Novosibirsk University Publishing House, 1993. 364 p.
8. Chaklin V.D. Evolution of ideas in spine surgery and orthopedics // Orthopedist. traumatol. 1971. No3. With. 48−54.
9. Yumashev G.S., Furman M.E. Osteochondrosis of the spine. 2nd ed., revised. and additional M.: Medicine, 1984. 382 p.
10. Andersson G. Epidemiology if spinal disorders. /In: Frymoyer jw, editor. e adult spine: principles and practice. New York: Ravel Press, 1991. pp. 107–146.
11. Slinyakov L.Yu., Chernyaev A.V., Bobrov D.S. Classification of structural and functional disorders of the thoracolumbar spine in osteoporotic deformities // Moscow Surgical Journal. 2013. No. 3. p. 54−60.
12.Caspar W. A new surgical procedure for lumbar disc herniation causing less damage through a microsurgical approach // Advances in neurosurg. 1977. Vol. 4. P. 74−77.
13. Khoo LT, Palmer S, Laich DT et al. Minimally invasive percutaneous posterior lumbar interbody fusion // neurosurgery. 2002. Vol. 51. P. 166–171.
14.Magerl F. translaminare verschraubung der intervertebralgelenke. / In: weber b., Magerl F. eds. Fixateur externe. Berlin: Springer-Verlag, 1985. P. 315−317.
SURGICAL TREATMENT OF DEGENERATIVE LUMBAR SPINE: HISTORY, THE TRADITIONAL APPROACH (LECTURE)
A. V. CHERNYAEV1, L. YU. SLINYAKOV1,2, ND KHURTSILАVA2
1Botkin City Clinical Hospital, Moscow
2Sechenov First Moscow State Medical University, Moscow
Review lecture. Present the evolution of views on the surgical treatment of degenerative lumbar spine – from the rst attempts to remove the intervertebral disc to modern decompressive-stabilizing operations with the use of high-tech methods.
keywords: low back pain, instability of the vertebral-motor segment, discectomy, transpedicular xation.