16 June 2020
37798
0
3.5 out of 5
Metastases in the spine are second-order tumors found in 13% of cases. They are localized in the area of the vertebral bodies, spinal canal, inside the spinal cord, and are a serious complication of cancer of other organs. The disease often remains asymptomatic for a long time, so, unfortunately, secondary tumors in the spine are not always detected in a timely manner. Preventing their appearance is the main goal of treating the primary tumor, but due to the peculiarities of the course of cancer in the early stages and a number of other factors, neurosurgeons often have to deal with such a phenomenon as metastases in the spine and begin an active fight against such a formidable enemy.
Almost 96% of all malignant tumors of the spine are secondary.
What are metastases and the reasons for their formation
Metastases are neoplasms that form against the background of an aggressive course of cancer. They are formed from cells separated from the original malignant tumor, which, through the blood and lymph flow, can enter any organ of the human body. In 13% of cases, they “settle” in the spine and begin to actively divide, thus forming a new tumor.
The presence of metastases indicates III or terminal, i.e. IV, stage of cancer.
Therefore, the maternal and daughter formations will have the same histological structure. Only in isolated cases is the similarity between metastases and the primary focus difficult to trace. This is called heterogeneity.
The main way for malignant cells to enter the spinal region is through the bloodstream. Much less often they penetrate into the epidural space and bone tissue through the lymph. Most often, metastases in the spine are a consequence of cancer of the prostate, mammary glands, kidneys, as well as the respiratory and gastrointestinal tract. But this does not mean that malignant tumors of other organs cannot lead to the formation of secondary tumors in the spine.
Modern oncologists are of the opinion that spinal metastases can occur against the background of all forms of carcinomas and sarcomas.
Deterioration in the well-being of patients most often occurs precisely with the development of metastatic cancer. This is accompanied by serious disruptions in the functioning of most vital organs and the development of complications.
Causes
If you identify the problem at an early stage of the disease, you can prevent the destruction of bone and cartilage tissue in all segments of the spine.
It is degenerative changes that gradually contribute to such destruction. The main reasons leading to such pathological changes include:
- Leading an unhealthy lifestyle;
- Passivity;
- Having bad habits.
A number of factors can also contribute to the occurrence of degenerative changes in the lumbar spine:
- Walking and sitting in an incorrect position lead to deterioration of blood circulation in the spine, as a result, metabolic processes in tissues are disrupted. As a result, cartilage and bone tissue weakens; any movement can lead to microscopic injuries. Degenerative changes in the lumbar spine are observed precisely at this moment.
- The condition of the spinal segments in the lumbar region can be affected by regular excessive physical activity.
- Various injuries can also lead to such changes
- Weakening muscle tissue is another unfavorable factor.
- The result of damage to a segment of the lumbar spine can be infectious or endocrine diseases.
In fact, there are many more reasons than stated above. Whatever the reason, the most important thing is timely identification of the disease and immediate treatment.
To identify pathologies, it is important to undergo a medical examination with a doctor annually. Indeed, in the first stages of the disease, people do not perceive this condition as a disease; they mistakenly think that the discomfort arose due to overwork and will soon pass. Only a trip to the doctor can dispel all doubts.
Types of metastases in the spine and their features
Metastases that form in bone tissue can be:
- Osteolytic (osteoclastic daughter tumors) – characterized by high activity and a tendency to destroy bone structures. Therefore, when conducting X-ray studies in such cases, a pronounced decrease in the height of the vertebrae is observed.
- Osteoblastic (osteosclerotic) – cause pathological growth of bone and an increase in its density. In the presence of such metastases, not only the vertebral bodies are affected, but also their arches along with their processes. On x-rays, the pathological process appears as numerous spots in the bone structures, and an increase in the size of the vertebrae is also observed.
Secondary tumors of these types can form in any part of the spine, which determines the clinical picture of the disease. This is explained by the fact that each vertebra is in direct contact with specific spinal roots and vessels that are connected to specific internal organs and parts of the body.
Metastases in the cervical spine
Oncopathology is rapidly developing, causing severe pain in the neck and head even in the early stages of its occurrence. This is the result of mechanical compression of blood vessels and nerves, which in many cases allows the disease to be diagnosed early and appropriate measures taken. Pain tends to occur or intensify when trying to turn or tilt the head.
The malignant process quickly spreads, covering an increasing number of healthy tissues. As a result, various types of sensory disturbances in the hands may occur, such as numbness and tingling sensations, as well as muscle weakness. Attacks of dizziness, impaired coordination, memory, decreased vision and hearing are often observed.
Metastases in the thoracic spine
The formation of secondary tumors in the thoracic spine later leads to symptoms. The first of these is pain in the area of the shoulder blades, which is a consequence of compression of the nerve endings and spinal cord stenosis. Additionally, there is a feeling of numbness, a feeling of goosebumps and tingling of the skin in the chest area. Pain during the formation of metastases in the thoracic region radiates to the ribs and pelvic area.
Metastases in the lumbar spine
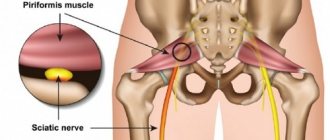
With metastatic lesions of the lumbar spine, the pain may resemble renal colic. Tumors progress rapidly and provoke an increase in static tension between most elements of the ridge. Since the lumbar region bears the greatest load, the formation of metastases in it significantly increases the risk of compression fractures.
An increase in size of the secondary tumor leads to pinching of the spinal cord and nerves of the cauda equina, which causes sensory disturbances in the legs, perineum and buttocks. There may also be a deterioration in supporting function, which can ultimately lead to complete paralysis of the legs.
Metastases in the spinal cord
Metastasis to the spinal cord (intramedullary metastases) is more typical for cancer of the stomach, lungs, mammary glands and prostate gland. This is observed in 4% of cases and may be accompanied by:
- muscle weakness, reaching paralysis;
- various types of paresthesia (sensitivity disturbances);
- violation of control up to its complete loss over urination and defecation.
All symptoms are observed on both sides of the body.
When metastases form in the spinal cord and spread to the brachial plexus, Horner's syndrome may be observed, accompanied by ptosis, dry face on the affected side, as well as miosis and enophthalmos.
The current level of development of medicine does not allow surgical removal of spinal cord metastases. Therefore, in such situations, unfortunately, we have to limit ourselves to palliative methods, i.e., those that improve the patient’s condition, but do not have a therapeutic effect. Patients are prescribed potent analgesics, radiation therapy and chemotherapy.
Pain arising from degenerative diseases of the spine in the vast majority of cases is chronic, as it tends to be long-lasting and recur [2].
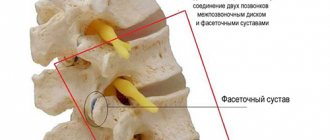
The main complaint of patients is pain in the lumbar spine. It can be caused by degenerative changes in the intervertebral discs, numerous ligaments, muscles or intervertebral joints [11, 17]. Pathological changes of a degenerative nature in the intervertebral joints, leading to their deformation and the development of persistent pain, are usually called spondyloarthrosis of a certain part of the spine. This pathology almost always accompanies degenerative changes in the lumbar intervertebral discs (osteochondrosis or discosis) due to a decrease in the height of the intervertebral space and disruption of the biomechanics of the spinal segment. During a clinical examination, the patient complains of pain in the lumbar spine, limitation of flexion and extension, as well as rotational movements in the lower back. Pain often radiates to the gluteal region, hip joint, groin area, thigh and lower leg [1, 9, 15]. When examining the patient, you can pay attention to the forced position of the body, tension of the paravertebral muscles on one or both sides. In addition to arthrogenic pain, these patients have discogenic or radicular pain caused by irritation of the posterior longitudinal ligament, on which the sinuvertebral nerve is located, and compression of the corresponding root by disc herniation [3, 16, 19].
According to our observations, in 70% of patients, lower lumbar pain syndrome can be caused by both discogenic and arthrosis pain syndrome, therefore, an isolated effect on one cause of pain will not give the desired result. For this group of patients, we developed and tested minimally invasive combined interventions in the clinic: percutaneous radiofrequency (RF) dereception of facet joints and percutaneous cold plasma (PC) nucleoplasty of the lumbosacral spine. The advantages of the methods are as follows: impact on two pathogenetic causes of pain syndrome (simultaneous), rapid postoperative recovery of the patient and return to work, as well as economic feasibility [7].
The purpose of the study is to develop differentiated indications and determine the effectiveness of PCP nucleoplasty in combination with CCP dereception of facet joints in vertebrogenic pain syndrome.
Material and methods
Since 1991, the Department of Neurosurgery of the Central Clinical Hospital of Civil Aviation has introduced and successfully used CCP dereception of facet joints, and since 2007, the CCP nucleoplasty method has been introduced using the Contrller 2000 device (“ArthroCare”). The uniqueness of the radiofrequency dereception apparatus lies in the fact that when used, it is possible to regulate the power of radiofrequency influence on the target, control temperature and exposure conditions at the target point. Consequently, by changing the temperature conditions at the source of exposure and near the target, the doctor can achieve the maximum therapeutic effect and at the same time be confident in the safety of the effect on surrounding tissues [1, 14]. PCP nucleoplasty is a new method developed by ArthroCare. The method is based on the disintegration of the nucleus pulposus of the disc under the influence of a focused plasma field, which is achieved by using low temperature (40-65 oC) [3, 5, 10, 18, 19]. In addition to the mechanical effect, nucleoplasty also revealed an effect at the biochemical level, in particular, a change in the composition of cytokines in the disc tissue. Research results have shown that changes in the content of cytokines in the disc after nucleoplasty are of great importance in the pathogenetic mechanism of treatment of pain syndrome and activation of reparative processes in disc tissue [10, 18].
CRF dereception of facet joints and CCP nucleoplasty were performed according to standard techniques widely covered in the literature.
The features of the combined operation of PCP-nucleoplasty and CCP-dereception of facet joints are as follows: the operation is performed under local anesthesia with intravenous sedation; with both interventions, the patient’s position on the operating table remains unchanged; PCP nucleoplasty is initially performed at one, two or three levels, depending on the clinical manifestations and data from neuroimaging studies; The second stage involves HRF destruction of the articular nerves with the selection of “target points” taking into account clinical manifestations [6].
139 patients aged from 21 to 70 years were examined and divided into three groups. Group 1 included 46 patients with arthrogenic lower lumbar pain syndrome who underwent HRF destruction of the facet nerves. Group 2 included 44 patients with discogenic pain syndrome; they underwent PCP nucleoplasty. Group 3 included 49 patients who had signs of both arthrogenic and discogenic pain syndromes, confirmed by MRI data. In this group, a combined method was used - CRF destruction of the facet nerves and CCP nucleoplasty.
The protocols for pre- and postoperative examination (clinical examination, radiographs and MRI scans), the composition of patients in groups by age, gender, concomitant diseases, localization of hernias and duration of the disease were identical, so we have the right to talk about correctly compared groups of patients and the results being assessed. Clinical and neurological manifestations are given in Table. 1.
In our study, examination methods included: X-ray examination of the lumbar spine in anteroposterior and lateral projections with mandatory functional tests [6]. On radiographs, in the case of degenerative lesions of the intervertebral discs and joints, subchondral sclerosis of the vertebral endplates, a decrease in the height of the intervertebral space, sclerosis and deformation of the articular surfaces, and a violation of their congruence are revealed (Fig. 1).
Figure 1. X-ray of the lumbar spine, lateral view. A - subchondral sclerosis; B - spondylosis; B — subchondral sclerosis of the facets.
The following magnetic resonance signs of arthrosis of the facet joints were taken into account: decreased signal intensity from the articular surfaces of the facet joints in T2 mode; narrowing and unevenness of the joint space; hypertrophy of the articular processes of the facet joints. Disc protrusion without rupture of the fibrous ring and protrusion of the hernia into the canal are visualized (Fig. 2).
Figure 2. MRI scan of the lumbar spine. A - disc protrusion; B - hypertrophy of the facet joints.
In the postoperative period, patients were recommended to rest in bed for 2-3 hours, followed by activation [4, 8]. During the first 24 hours, non-narcotic analgesics were prescribed.
Clinical case No. 1
Patient P., 47 years old, was admitted with complaints of pain in the lumbosacral region radiating to the right leg (along the outer surface of the foot), aggravated by movement, bending and turning, morning stiffness, as well as numbness along the outer surface of the right foot .
There is a history of low back pain for 2 years, especially after heavy physical activity. She was treated on an outpatient basis for 5 weeks, without any changes. Subsequently, the pain intensified and numbness appeared along the outer surface of the right foot. Neurological status: sensory disturbances in the form of hypoesthesia in the dermatome of the LV root on the right, the Achilles tendon reflex on the right is reduced. Locally: lumbar lordosis is smoothed, pain over the spinous processes of the LIV-SI segments and at paravertebral points, Lasegue’s symptom at an angle of 45° on the right, 60° on the left. The intensity of the pain syndrome on the visual analogue scale (VAS) was 7.5 points. After conducting instrumental research methods (MRI, lumbar spondylography with functional tests), the patient was diagnosed with spinal osteochondrosis. Spondyloarthrosis, spondylosis. LIV-LV disc protrusion (Fig. 3, A).
Figure 3. MRI data of patient P. before (A) and after (B) the operation of CCP-nucleoplasty and CCP-dereception of the facet joints.
The patient underwent CRF dereception of the facet joint at the LV-SI level on both sides in combination with CCP nucleoplasty at the LIV-LV level. The postoperative period proceeded smoothly, and there was almost complete regression of the pain syndrome (VAS score 2). After 12 months, the condition is satisfactory, no complaints. Pain intensity according to VAS 1 point. On the MR tomogram of the lumbar spine, the size of the protrusion at the LIV-LV level decreased from 6 to 2 mm (Fig. 3, B).
Clinical case No. 2
Patient S., 62 years old, was admitted with complaints of pain in the lumbosacral region radiating to the left buttock, along the posterior surface of the left thigh and along the posterolateral surface of the left leg, paresthesia in the form of “tingling” in this area, increased pain during extension in the lumbar region, in an upright position and when walking.
He has a history of suffering from spinal osteochondrosis for a long time. There has been a real deterioration in the last 6 months, when pain in the lumbar spine increased significantly, followed by pain in the left leg, conservative therapy without significant effect. On admission, pain intensity according to VAS was 7 points. During examination, paresis of the long extensor of the first toe on the left was noted up to 3.5 points. Tendon reflexes are lively, the knees are flaccid, the left Achilles is not evoked. Lasègue's symptom is negative on both sides. Local pain on palpation in the paravertebral region at the level of LIV, LV, SI, pain on palpation of the left piriformis muscle. MRI scan, spondylography of the lumbar spine with functional tests: manifestations of osteochondrosis, spondyloarthrosis of the lumbar spine, stable antelisthesis LIII by 2 mm. LIV-LV disc herniation (7.8 mm).
CRF destruction of the facet nerves at the LIV-LV and LV-SI levels on the left was performed in combination with CCP nucleoplasty of the LIV-LV intervertebral disc. In the early postoperative period, regression of pain syndrome was noted. However, 2 weeks after discharge, the patient was readmitted to the hospital due to relapse of pain. The patient underwent microdiscectomy and foraminotomy. The pain syndrome was relieved, the patient was discharged in satisfactory condition.
Results and discussion
The main criteria for assessing postoperative results (consultations, questionnaires, MRI, e-mail) were the dynamics of pain, which was determined by VAS. The results were assessed on days 2–3 (at discharge) and 6–12 months after surgery (Table 2).
With good results, there was a regression of pain to 2 points and below, with satisfactory results - from 2 to 4 points, with unsatisfactory results - 5 points and above.
Good results at discharge were observed in 33 (71.7%) patients of the 1st group, 34 (77.3%) patients of the 2nd group and 37 (75.7%) patients of the 3rd group. Good results after 6-12 months were observed in 17 (50.1%) patients of the 1st group, 20 (52.6%) of the 2nd group and 15 (48.4%) of the 3rd group, respectively.
Satisfactory results at discharge were observed in 8 (17.4%) patients of group 1, 6 (13.6%) of group 2, and 8 (16.3%) of group 3; 6-12 months after surgery - in 7 (26.4%) of the 1st group, in 10 (26.4%) of the 2nd group and in 10 (32.2%) of the 3rd group.
Unsatisfactory results at discharge were observed in 5 (10.9%), 4 (9.1%) and 4 (8.0%) respectively; 6-12 months after surgery - in 8 (23.5%), 8 (21.0%), and 6 (19.4%).
A control MRI was performed in 26 patients of groups 2 and 3 within a period of 1 to 12 months, according to which 10 (38.5%) patients showed a decrease in the size of the protrusion from 5 to 2 mm. In 11 (42.3%), the size of the protrusion did not change, but its shape changed to drop-shaped, which indicates a decrease in intradiscal pressure [3, 13]. In 5 (19.2%) patients after nucleoplasty and combined treatment, MRI scans showed an increase in the size of the disc herniation, which was explained by rupture of the fibrous ring. These patients underwent LV-SI microdiscectomy at different times due to pronounced increasing radicular symptoms with good results.
One of the indications for PCP nucleoplasty is the absence of rupture of the fibrous ring and the size of the protrusion is no more than 1/3 of the spinal canal [4, 5, 12]. Unsatisfactory results are a consequence of improper selection of patients in whom the size of the protrusion exceeded 1/3 of the spinal canal; the elderly age of the patients (over 60 years) is also an unfavorable factor.
Thus, the indications for performing CRF dereception of facet joints together with CCP nucleoplasty are:
- a combination of discogenic pain syndrome (with or without a radicular component) with painful manifestations of arthrosis of the facet joints, the size of the protrusion is no more than 1/3 of the spinal canal, according to MRI, the absence of ruptures of the fibrous ring, a decrease in the height of the disc by no more than 50% and the presence of arthrosis of the facet joints joints based on radiological data [5, 12];
— ineffectiveness of previously performed isolated CCP nucleoplasty or CCP dereception of facet joints;
- resistance to conservative therapy for 4-6 weeks.
conclusions
1. PCP nucleoplasty is an effective method in the treatment of discogenic pain syndrome, the effectiveness of which reaches 91.9%, and after 12 months - 79.0%.
2. In patients with mixed discogenic and arthrogenic pain syndrome, the most adequate method is the combined use of PCP-nucleoplasty and PFC-destruction of the facet nerves, the effectiveness of which at discharge is 92.0%, and after 12 months - 80.6%.
3. Indications for performing PCP nucleoplasty of intervertebral discs in combination with PCP destruction of facet nerves in vertebrogenic pain syndrome have been developed.
Factors that negatively affect the results of treatment are: inadequate selection of patients (undiagnosed rupture of the annulus fibrosus, patient refusal from open surgery), anatomical features of the surgical area (hypertrophy and widening of the facet joints, features of the passage of the recurrent nerves), soft tissue stenosis of the spinal canal or foraminal holes (often not diagnosed on low-tension MRI), the age of patients over 60 years old, the presence of disc protrusion of more than 1/3 of the spinal canal and ignoring the recommendations of postoperative rehabilitation.
Thus, with proper selection of patients, the isolated or combined use of CCP-nucleoplasty and CRF dereception of the facet nerves is an effective method of treating patients with vertebrogenic pain syndrome.
A comment
Methods of radiofrequency dereception of facet joints and percutaneous nucleoplasty using cold plasma have been increasingly used in our country in recent years to treat patients with degenerative diseases of the lumbar spine. In most clinics, their separate use is known. Each method has its own strict indications and is aimed at treating certain structures of the spinal segment. Thus, percutaneous nucleoplasty is relevant only for small disc herniations without rupture of the fibrous ring and without a pronounced decrease in its height. These changes obtained from MRI must strictly correspond to the clinical manifestations: radicular pain as a result of root compression and low back pain due to overstretching of the fibrous ring. Moreover, the pain caused by the pathology of the intervertebral disc differs from the nature of the pain caused by the pathology of the intervertebral joints. In the latter case (facet syndrome), the pain in the lower back is diffuse and intensifies when bending back. With intervertebral disc pathology, pain is localized in the midline and intensifies when bending forward. For facet syndrome, percutaneous radiofrequency deception is traditional.
Analyzing our results, we came to the conclusion that the effectiveness of these treatment methods is approximately 80%. It should be noted that after radiofrequency dereception of the intervertebral joints, as a result of regeneration of the nerve endings innervating the intervertebral joints, pain in the lumbar region may occur again after 1-2 years. Repeated dereception has good clinical results.
Considering clinical case No. 1 presented in this article, it should be noted that dereception was carried out only at one level - LV-SI. Considering the cross innervation of the intervertebral joints at the lumbar level, we recommend performing it simultaneously at three levels: LIII-LIV, LIV-LV, LV-SI, even if there is only local pain from the LV-SI level. This should lead to a more durable clinical effect.
In general, the article is devoted to a current topic in the surgery of degenerative diseases of the spine. The described experience of simultaneous use of radiofrequency dereception and nucleoplasty using cold plasma is necessary information for neurosurgeons, orthopedists and neurologists dealing with this problem.
ON THE. Konovalov
(Moscow)
Signs of metastases in the spine
It is already obvious that the nature of the symptoms depends on the location of the metastases in the spine. Also, the number and area of lesions have a significant impact on the well-being of patients. In general, the clinical picture of tumor metastasis to the spine is accompanied by several syndromes:
- radicular - damage to the spinal roots, which are responsible for transmitting nerve impulses from the spinal cord to all internal organs, is accompanied by severe pain and neurological disorders;
- myelopathic – compression of the spinal cord by a growing tumor, which causes severe pain in the affected area and paralysis;
- polyneuropathic – changes in the autonomic nervous system, leading to increased sweating and impaired sensitivity of the hands and feet, as well as deterioration of reflexes.
Myelopathic syndrome is most often observed with metastasis to the thoracic spine.
Radicular disorders deserve the most attention. They consist in the appearance of pain, which becomes a consequence of damage and destruction of the spinal roots. More often they are observed with the formation of metastases in the cervical and thoracic region, since the spinal cord in an adult ends at the level of 1 or 2 lumbar vertebrae. But in this section there is a huge plexus of nerves (“cauda equina”), which can also be pinched by the tumor, which will lead to neurological disorders of the legs and pelvic organs.
Patients may experience typical signs of radiculopathy, girdle pain, decreased expression of the knee and Achilles reflexes, as well as sharp pain when trying to palpate the spine in the area where the tumor is located. In certain cases, the pain syndrome goes away on its own, but this sign cannot be regarded as an indicator of recovery. In fact, the disappearance of pain is explained by the destruction of the nerves passing in close proximity to the malignant tumor. Subsequently, as it increases, new nerves will be involved in the pathological process, which will provoke a resumption of pain.
The formation of metastases in the spine causes severe metabolic disorders. They gradually destroy the structural elements of the spine and paravertebral (surrounding the spine) tissues. In the later stages, they are so critical that there is a significant deterioration in general well-being and an increase in local symptoms. In addition to pain, paresis, paralysis, patients suffer from anemia, nausea and vomiting. In particularly difficult situations:
- breathing disorders occur, manifested by shortness of breath, followed by attacks of respiratory arrest;
- changes in body temperature, both upward and downward;
- There is apathy, weakness, lack of interest in food and the surrounding world.
Such signs indicate not only an extremely serious condition of the patient, but also an imminent death outcome. Therefore, it is worth making every effort to prevent this from happening. Today, most cancers are curable, but only if they are diagnosed at the earliest stages. But since cancer symptoms usually appear when the tumor has already reached stage 2 or 3 of development, it is important to undergo regular preventive examinations. In such cases, small tumors are an “accidental” discovery, which makes it possible to effectively treat them and achieve stable remission.
MRI diagnostics for pain syndrome due to damage to the lumbar spine
Low back pain is familiar to almost every person and often leads to temporary disability. The most common is low back pain caused by changes in the lumbosacral spine. The classic manifestations of diseases of the lumbar spine are well known: with pain in the lower back, radiating to the buttocks and along the back of the legs, a diagnosis is made quickly. Difficulties arise when pain radiates to the perineum, scrotum or along the front of the legs. In this case, an inguinal hernia or a hernia of the obturator foramen with compression of the nerves is mistakenly suspected. Difficulties also arise in the diagnosis of spondyloarthropathies, the prevalence of which is currently much wider than is commonly believed. To avoid mistakes in such cases, it is always necessary to exclude spinal disease.
The main causes of pain identified by MRI examination are the following:
Due to the heavy load and lack of rib protection, the lumbar region is most often affected. Pain and accompanying symptoms are most often caused by damage to the intervertebral discs, with the L4/5, L5/S1 discs most often affected.
The main symptom of osteoarthritis is severe limitation of movement. In most cases, patients cope with this inconvenience for some time, but as osteoarthritis progresses, subluxation of the articular processes of the vertebrae occurs, which leads to narrowing of the intervertebral foramina, and concomitant osteochondrosis leads to stenosis of the spinal canal. These changes lead to compression of the spinal nerves and deformation of the dural sac, causing radiculo- and myelopathies.
Herniated discs and osteophytes can cause inflammation in the epidural space and on the outer surface of the dura mater of the spinal cord (epiduritis).
| Osteochondrosis, deforming spondylosis. Spinal stenosis; compression of the dural sac. Extradural space-occupying lesion at the L3-L4 level (susp. epiduritis) |
| L5/S1 disc herniation |
| L4/5 disc herniation with caudal migration |
| Osteochondrosis. Hernias L4-S1; hernial sequestration L5/S1 with cranial migration to the pedicular level |
Pain occurs due to tension in the spinal ligaments or irritation of the spinal roots.
| Antelisthesis of the L5 vertebra, “vacuum” phenomenon of the L5-S1 disc |
Neurological symptoms appear when the tumor compresses or grows into the spinal roots or spinal cord. The symptoms are very varied and are characterized by their steady progression.
The most common malignant neoplasms are myeloma and spinal metastases.
| Pathological infiltration (metastases or multiple primary tumors) of the sacrum |
| Intradural space-occupying lesion at the L5 vertebral level |
| Space-occupying formation of the sacrum (pathological infiltration, destruction, paravertebral component) differential diagnosis with metastasis |
| Focal changes in the L3 vertebral body (hemangioma). Chondrosis |
| Volumetric formation of the sacrum (pathological infiltration); verified myeloma disease |
| Metastases |
There are both traumatic and pathological compression fractures caused by destruction of the vertebrae due to multiple myeloma, metastatic disease or osteoporosis.
| Pathological fracture of the L4 vertebra; osteoporotic fracture of the L2 vertebra; L2 retrolisthesis. | Osteoporosis. Osteoporotic fractures of L2-L5 vertebrae | Osteoporosis. Osteoporotic fractures of Th11, Th12 vertebrae, osteoporotic deformities of L1-L3, L5 vertebrae |
| Compression fracture of the L1 vertebra (chronic period) |
| Fracture of L4 vertebra (horizontal) |
| Compression-comminuted fracture of the L1 vertebra (chronic period) |
| Osteomyelitis L4-L5 |
| Epidural abscess |
| Spondylitis L4-S1; epiduritis; abscess formation in the anterior parts of the spinal canal |
| Spondylitis; contact destruction. Spinal stenosis (congenitally narrow spinal canal) |
| Spondylitis Th12-L1, L5-S1 subacute period |
This group of diseases is characterized by damage to the sacroiliac joints and spine, oligoarthritis and enthesopathies. The symptoms listed above occur at rest (especially in the morning, after sleep) and decrease after physical activity.
| Bilateral sacroiliitis stage 4 (partial synostosis), beyond the acute stage; deforming spondylosis at the level of Th12-S1 segments (Bechterev's disease) |
| Left-sided sacroiliitis; chondrosis, L4/5 protrusion |
| Ankylosing spondylitis (Bechterew's disease). |
| Vascular malformation of the spinal canal; myelopathy |
| Post-contrast |
| Malformations – synostosis L4-L5 |
| Concrescence of bodies L3-L4; osteoporotic body deformity Th12 |
According to some experts, pain in the lower back is a kind of retribution of humanity for upright walking, when the greatest load falls on the lumbar spine, which bears the main burden of the weight of the human body. Physical inactivity, poor nutrition, obesity, and stress also have a detrimental effect. Lower back pain can occur only once and disappear without a trace, or it can return again and again, causing considerable suffering. Low back pain is a nonspecific symptom that can be caused by many reasons. Many different examination methods help the clinician to reliably make a topical diagnosis and start treatment in a timely manner, among which the leading role is currently occupied by the modern method - MRI of the lower back.
Diagnostics
Spinal metastases are detected by X-ray, CT and MRI. When metastatic cancer is detected, efforts are directed toward detecting the primary tumor, as well as accurately determining the location of secondary lesions and their extent. For these purposes, an examination is initially carried out by a neurologist, vertebrologist and oncologist. Doctors collect anamnesis, conduct a visual examination, and palpate the spine. Reflexes, muscle tone, sensitivity and neurological tests must be assessed to determine the level of spinal cord damage.
Patients are prescribed laboratory and instrumental diagnostic methods:
- CBC - shows specific changes typical of late stages of oncology, including a decrease in red blood cell titer and severe anemia;
- tests for tumor markers SCC, NCE, CA 242, CEA, CA 19-9 - indicators exceeding the norm in any of them are a sign of a high probability of cancer of the corresponding organ;
- spinal puncture followed by histological examination of the cerebrospinal fluid - used to diagnose the oncological process in the spinal cord;
- X-ray of the spine - shows the extent of metastases and the involvement of nearby anatomical structures in the pathological process;
- chest x-ray – used to search for a primary tumor in the tissues of the lungs and bronchi;
- Ultrasound of the abdominal cavity and pelvis - used to detect primary malignant neoplasms in the gastrointestinal tract, kidneys, prostate gland, uterus and appendages;
- MRI of the spine - helps to accurately assess the condition of the spinal cord, its roots and the degree of damage to bone tissue;
- Spinal scintigraphy - involves the use of radioactive substances that accumulate in metastases, which makes it possible to detect the slightest secondary oncological foci with high accuracy.
- PET-CT allows you to accurately diagnose and identify metastatic foci throughout the body
It is important to differentiate metastatic cancer from a primary tumor of the spinal cord and spine, as well as Guillain-Barré syndrome and inflammatory processes affecting the membranes of the spinal cord.
Treatment of metastases in the spine
Yes, the presence of metastases in the spine is a sign of advanced cancer. But this is not a reason to fold your arms and prepare for an imminent death. The modern level of development of medicine can significantly improve the quality and life expectancy of such patients.
In each case, the forecast is compiled individually. It depends on many factors, including the age of the patient, the location and extent of the metastatic process. Of course, each person must decide for himself whether it is worth fighting further, given that the upcoming path of palliative treatment cannot be called simple.
Treatment of spinal metastases includes:
- drug therapy;
- radiation therapy;
- surgery.
The nature of the recommended therapy in each case is selected individually and directly depends on the characteristics of the maternal tumor, as well as the stage of the disease.
Drug therapy
Medicines for metastatic cancer are used to alleviate the patient's condition and increase the effectiveness of other components of therapy. Most often, the use of drugs from the following groups is recommended:
- antitumor – prevent the division of malignant cells and help stop further tumor growth;
- detoxification – help cleanse the body of the products of drug metabolism and tissue breakdown;
- painkillers – used to relieve pain of varying intensity;
- antiemetics – help maintain normal condition after courses of chemotherapy and radiation therapy;
- sedatives – improve the psycho-emotional state, help normalize sleep;
- bisphosphonates – prevent the destruction of bone tissue and have an analgesic effect;
- mineral supplements of iron and calcium - are used to compensate for the deficiency of these minerals in order to prevent the development of osteoporosis and anemia.
Hormonal drugs are also often prescribed for metastatic cancer. They are necessary to reduce the production of estrogens and androgens in cases of diagnosing hormone-dependent tumors.
Radiation therapy
Radiation therapy involves precisely dosed radiation exposure. It is most effective in the presence of tumors smaller than 2 cm, but is also used to treat large tumors. In such situations, radiation therapy helps to reduce their size.
For each patient, the radiation dose is selected strictly individually based on the severity of the disease and the sensitivity of the malignant cells of the maternal tumor and metastases in the spine to radioactive radiation.
Today, radiation therapy can be carried out in a targeted manner without affecting healthy tissue, and can also affect tumors in hard-to-reach places, which was previously impossible.