A violation of the statics of the cervical spine is quite rare. This deviation can seriously harm the patient’s body, causing not only obvious visual symptoms, but also discomfort and pain. It is necessary to diagnose the problem in time in order to completely cure and correct the deviation. If the disease is detected early, the likelihood of complete correction is high.
The section where the neck of any person is usually located consists of 7 main vertebrae that are capable of providing the necessary movement to the head. These vertebrae also connect the skull to the spinal column thanks to the occipital complex. Nature created intervertebral discs in humans so that the spinal column could perform static functions. The entire system has a certain integrity, which is ensured by the placement of these components in a certain order. If the condition of the discs is disturbed, a violation of the statics of the neck is also detected. Depending on the degree of disturbance, osteophytes are identified - growths of bone tissue.
Symptoms of dystrophic changes in the cervical spine
Degenerative changes in the cervical spine occur slowly in the body and, during their development, begin to manifest themselves with the following symptoms:
- You begin to suffer from headaches of unknown etymology.
- You are tormented by wandering pain in the shoulders and spinal joints.
- You feel a decrease in the range of motion in your neck. You cannot turn your head completely to the right or left.
- There is a constant feeling of “petrification” in the shoulders.
- Sometimes there is a feeling of numbness in the hands, and you need to constantly stretch your limbs.
- Regular lumbago occurs.
- There is a swelling on the back of the neck to the touch.
- You notice a curvature of the spine, stoop, and cervical lordosis.
Sometimes cervical osteochondrosis can cause dizziness and even fainting. It is known that there are arteries in the cervical spine. With osteochondrosis, the arteries can become pinched and cause headaches and dizziness. But this phenomenon is quite rare in the practice of doctors. Most often, dizziness in people is caused by vascular problems, diseases of the ENT organs, strokes, and vestibular anemia.
What are degenerative-dystrophic changes in the spine?
Both among ordinary patients and in the medical information space, it is customary to equate the concept of degenerative-dystrophic changes in the cervical spine with the term “osteochondrosis,” which is not entirely correct.
Osteochondrosis is only one of the forms of manifestation of the degeneration process in vertebral structures. But often many symptoms that are completely unrelated to this form of degenerative changes in the spine are attributed to this condition. For example, cervical osteochondrosis has nothing to do with the vestibular analyzer and does not affect the inner ear system. It is not always correct to attribute pain symptoms in the ear area to it. Initial appointment with a NEUROLOGIST
ONLY 1800 rubles!
(more about prices below)
Wearing a corset and giving a massage
What to do if your neck hurts? For people with this condition, it is best to use special corsets that will help avoid possible displacement of the vertebrae and maintain the correct position of the spine when walking. A good effect can also be achieved by using course massage and physical therapy, which helps strengthen muscles and strengthen ligaments. The patient must properly organize his workplace and choose a good orthopedic mattress for sleeping.
Problems with the position of the vertebrae are a serious pathology that requires professional treatment. Only timely assistance from the attending physician and proper treatment will help prevent surgery and avoid deterioration of the condition and severe pain.
Causes of the disease
Cervical, lumbar, thoracic, sacral areas of the spine can become targets of degenerative processes in the spine. Many scientists believe that this is a kind of payment a person pays for his upright posture. Due to the load that the spine receives daily, over time, the content of hyaluronic acid and bound water in the nucleus pulposus of the intervertebral discs decreases. The collagen network is also destroyed. As a result, the core loses its gel properties, and the disc begins to thin out and lose elasticity. There is a process of weakening the adhesion force between the collagen plates of the fibrous ring. All this becomes the cause of cracks and breaks in it. In addition, due to lack of nutrition, lime salts begin to be deposited near the vertebrae. Gas (nitrogen) is released from the disk substance, the so-called vacuum phenomenon. The marginal parts of the disc protrude beyond the vertebral bodies, forming protrusions.
Functional disorder of the spine
In order to understand what the functional disorder of the spine is, it is necessary to find out exactly what functions this part of the musculoskeletal system performs. They include:
- supporting function – the spine creates a reliable frame for the whole body;
- shock-absorbing – due to physiological bends and cartilaginous intervertebral discs, physical load is evenly distributed during movement of the human body;
- ensuring upright walking - between the last lumbar and first sacral disc there is a conditional center of gravity of the human body, which allows you to walk on two legs;
- protective - inside each vertebra there is an oval hole that forms the walls of the spinal canal, it contains the spinal cord, which is responsible for the innervation of the entire body;
- motor – due to flexibility and mobility, the spinal column allows you to make various movements of the body (bending, turning, twisting, etc.).
Providing statistics, i.e. a certain limitation of movement and stability of the position of the vertebral bodies relative to each other - this is another important function, not of the spinal column, but of the muscular frame of the back, ligamentous and tendon apparatus located along it. If it is subjected to extreme physical stress, inflammation, stretching and other negative impacts, then the algorithm of its operation changes. The muscular frame of the back loses its ability to hold the spinal column in a certain position. When the ligaments of the spine are sprained and scar deformities occur in their structure, instability in the position of the vertebral bodies occurs. Most often, dysfunction of the spine is secondary in nature - it develops against the background of long-term diseases of a degenerative and deformative nature.
Treatment of static disorders without concomitant therapy for these diseases is impossible. Therefore, at the initial stage of diagnosis, it is important to establish all possible causes and conduct a full examination of the condition of not only the spinal column, but also the soft tissues surrounding it.
Types of degenerative changes in the spine
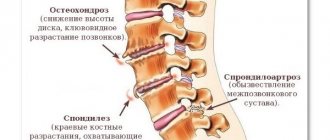
Degenerative changes in the cervical spine in medicine include:
- osteochondrosis, which can manifest itself as degeneration of the intervertebral disc, disc protrusions, their calcification and vacuum phenomenon, spondylolisthesis, Schmohl's hernia;
- spondylosis, Forestier disease;
- intervertebral disc herniation or extrusion;
- spondyloarthrosis - arthrosis of the intervertebral joints (facet syndrome), Bostrup syndrome;
- hypertrophy of the ligamentum flavum;
- spinal canal stenosis.
Most often, neurologists diagnose their patients with a degenerative pathological change such as osteochondrosis. The term "osteochondrosis" was proposed by two neurologists Brandon and Popelyansky in the mid-20th century and was subsequently widely popularized in Soviet medicine. Osteochondrosis itself means an inflammatory process and degenerative changes in the cartilage of the spine. This change is chronic and develops in all people with age, sooner or later. Most residents of St. Petersburg, if they do an MRI of the spine after 40 years, will find at least minor signs of osteochondrosis.
Previous Next
Regular displacement of the vertebrae
During physical activity, this provokes a minimal shift in the position of the vertebrae in the horizontal plane. This mobility is due to the structural features of the ligamentous apparatus. It is fastened on the front and back sides by strong longitudinal ligaments, which help maintain its position during tilting. On the lateral sides there are only intervertebral tendons, the strength of which is too low to maintain normal statics.
Often, regular displacement of the vertebrae leads to osteochondrosis, which develops over several years. The most dangerous thing is that throughout the entire time the patient does not feel any symptoms and feels normal.
Stages of the disease
Staging of degenerative diseases of the spine is very conditional, since this group includes various forms of degeneration. In the medical literature, it is most often customary to distinguish 3 stages of the progression process:
- dysfunction - the appearance of processes leading to rupture of the fibrous ring;
- instability - the disc loses its stability and changes its height and position;
- restabilization is the body’s response to disc instability in the form of the process of formation of bone growths (osteophytes) and narrowing of the spinal canal.
Diagnostics
A neurologist diagnoses back diseases. If degenerative-dystrophic diseases in the cervical spine are suspected, he will issue a referral for an MRI of the cervical spine. Since degeneration, as a rule, is not local in nature, but affects the entire spinal column, doctors often prescribe a comprehensive tomographic examination of the back - MRI of the entire spine. In case of cervical osteochondrosis with symptoms of dizziness, a neurologist may suspect cervical artery syndrome and prescribe the patient an MRI of the cervical spine and MRI of the neck vessels to assess the condition of the cervical arteries and veins.
What will an MRI show for degenerative changes in the spine?
The MRI picture of dystrophic changes in the cervical region of the back will be visible to doctors in the images based on a number of clear signs:
- by the dark color of the discs, since during degenerative processes water leaves the discs;
- reducing the height of the disc;
- the presence of osteophytic spurs in the area of the edges of the end plates;
- prolapse of the disc into the tubular substance of the vertebra;
- displacement of the overlying vertebra in relation to the underlying one;
- fatty degeneration within the vertebral bodies.
| Service | Price according to Price | Discount Price at Night | Discount Price During the Day |
| from 23.00 to 8.00 | from 8.00 to 23.00 | ||
| MRI of the cervical spine | 3300 rub. | 2690 rub. | 2990 rub. |
| MRI of neck vessels (MR angiography of the neck) | 3300 rub. | 2690 rub. | 2990 rub. |
| MRI of the craniovertebral junction | 3300 rub. | 2690 rub. | 2990 rub. |
| MR arteriography of the neck | 3300 rub. | 2690 rub. | 2990 rub. |
| MRI of the cervical spine with contrast | from 6300 rub. | ||
| MRI of the brain and neck | 6600 rub. | 5380 rub. | 5980 rub. |
| Comprehensive MRI examination of the vessels of the brain and neck | 6600 rub. | 5380 rub. | 5980 rub. |
| Comprehensive neck examination (cervical MRI and MR angiography) | 6600 rub. | 5380 rub. | 5980 rub. |
| Neurologist appointment | 1800 rub. | free after MRI | free after MRI |
| Comprehensive neck diagnostics (MRI of the cervical spine, MRI of neck vessels, ultrasound of neck vessels, ultrasound of the thyroid gland and soft tissues of the neck, consultation with a neurologist) | 13200 rub. | 9500 rub. | 9500 rub. |
| Contrast administration (based on patient weight) | from 4000 to 6000 rub. |
Circulatory disorders with static dysfunction of the spine
Any static disorders of the spine invariably lead to changes in the functionality of a number of systems:
- the movement of blood through the main blood vessels, which are located inside and outside the spine, is disrupted;
- the process of diffuse nutrition of the cartilage tissue of the intervertebral discs changes, due to which they become dehydrated and lose their functionality, and a spinal hernia develops;
- physiological posture is disturbed;
- the chest is deformed;
- the position of the heart, lungs, and abdominal organs changes;
- dysfunction of the intestines and bladder occurs (urinary and fecal incontinence may occur);
- congestion forms in the lymphatic system.
When the static function of the spine is disrupted, all organs and systems of the human body suffer without exception, since the spinal cord, located in the spinal canal, is responsible for the innervation of all areas. Any deformation of the spinal canal causes serious neurological problems.
The process of circulatory disorders in the spine depends on the degree of deformation. If the displacement of the vertebrae is insignificant, then the arteries inside the spinal canal are not infringed and continue to fully supply the structures of the spinal cord and the radicular nerves extending from it with blood. If poor posture and vertebral displacement are significant, then areas of ischemia may occur. A spinal stroke develops with paralysis of certain parts of the body and changes in the functioning of internal organs.
Treatment
60% of people aged 35 years and older have serious forms of degenerative changes in the spine, which significantly impair their quality of life and require consultation with doctors. A neurologist treats degenerative-dystrophic diseases of the cervical spine. Basically, such changes in the cervical spine from the doctor will require either procedural therapy (droppers, acupuncture, plasma therapy) and pharmacological treatment, or physical therapy (massage, manual therapy, reflexology, unloading treatment based on spinal traction, vibration stimulation, exercise therapy). If a patient comes to see a neurologist with severe pain, the doctor will most likely suggest a therapeutic blockade or start taking painkillers or anti-inflammatory medications. You need to understand that medical blockade is not a method of therapy, it only helps relieve back pain in order to begin systemic treatment. Therapeutic measures for degenerative-dystrophic changes in the spine are aimed primarily at slowing down degeneration and improving the nutrition of intervertebral discs and vertebrae.
Osteophytes and dislocations
When problems arise, a disease is often diagnosed in which the vertebra becomes dislocated. The discs not only move away from the desired position, but also twist. Often the vertebrae do not extend beyond the disc, which makes the doctor’s work easier. The doctor easily adjusts everything the patient needs. But if the situation involves one vertebra going beyond the same, then the patient needs serious and quick help. Nerve fibers become pinched, and the circulatory system ceases to effectively perform its function. Spinal cord hemorrhage and even death may occur.
If the dislocation is not too serious, the patient experiences problems with breathing and swallowing, as well as sharp pain in the back of the head.
If the static condition worsens as a result of the appearance of specific growths in the bone tissue, then such a disease is called osteophyte. There may be several reasons for this. This is a serious strain on the neck. The patient experiences unpleasant sensations, namely a severe headache, and motor function is significantly impaired. This pathology can be diagnosed by contacting a medical institution, where the doctor will do an X-ray examination. These growths will definitely be visible on an x-ray. An experienced doctor can palpate them.
Prevention
As preventive measures to maintain the health of your neck and back, neurologists at medical centers in St. Petersburg recommend:
- avoid static poses;
- swim in the pool and support your back with physical exercises;
- Monitor the level of vitamin B12 in the blood and eat vitamin B-containing foods.
For older patients, depending on the stage of degenerative changes in the cervical spine, the following will be indicated:
- do an MRI of the spine once a year to monitor the rate of degenerative changes;
- undergo a course of plasma therapy for the spine 1-2 times a year;
- do a course of therapeutic massage of the collar zone, exercise therapy, manual therapy;
- do a seasonal (spring - autumn) procedure for drip vitaminization of the body.
Author: Shogenov Ramish Kurbanovich
Neurologist with 10 years of experience
Currently, spinal instability (M 53.2) is one of the most common spinal problems with which patients seek help in outpatient medical institutions.
Instability of the cervical spine (CS) is the appearance of additional degrees of freedom during flexion or extension, when the muscular-ligamentous apparatus of the cervical-collar zone is not able to provide movement of the seven cervical vertebrae as a whole [9]. The history of studying the phenomenon of instability began in the 30-40s of the 20th century, when researchers began to pay great attention to the issues of osteochondrosis and especially to the violation of the fixation ability of the dystrophically changed spine. The term “instability” was first introduced by A. Ferguson in 1934, but over the years, many authors have defined the essence of this concept differently [20]. The first opinions on the causes of spinal instability were expressed by foreign authors. For example, R. Hirsch in 1948 associated the occurrence of such a pathology with partial or complete rupture of the fibers of the posterior sections of the fibrous ring of the intervertebral disc [27]. A. Farfan considered instability of the intervertebral segments as a result of damage to at least one of the following supporting components: the disc, one or both facet joints.
The second wave of studying this phenomenon, associated with the names of domestic researchers, arose in the 70s of the last century. So, according to L.Ya. Tsivyan, “segmental instability is one of the earliest functional features of disc degeneration, characterized by the appearance of unusual movements forward and backward, and manifested radiographically by displacement of the overlying vertebra anteriorly during flexion and posteriorly during extension” [22].
G.S. Yumashev defined instability as excessive sliding of the vertebrae in the sagittal plane by more than 2 mm relative to each other, accompanied by pain due to the tension of the abundantly innervated joint capsules [26]. The history of the issue of spinal instability is also associated with such names as A.I. Osna, N.I. Khvisyuk, G.V. Pavelescu, I.Yu. Popelyansky et al. [20]. But the subject of interest, as a rule, was the lumbar spine. Only later did researchers pay attention to the instability of the SHOP and its consequences.
Along with studying the pathology of the statokinetic function of the cervical spine, doctors also paid attention to the features of hemodynamics in the vertebral arteries (VA) located in the bone canal of the transverse processes of the cervical vertebrae. And the first to assess the significance of the pathological mobility of the cervical vertebrae, raising the issue of intrapartum damage to the cervical spine, the clinical features of the pathology, and the age range of the most pronounced manifestation of vascular disorders, was A.Yu. Ratner [10, 14].
It is currently known that acute and chronic dislocations of the upper cervical vertebrae lead to acute and chronic trauma to the VA with corresponding disturbances of blood and lymph circulation in the vertebrobasilar system (VBS). Disruption of the statics of the cervical intervertebral segments is accompanied by damage to the caudal parts of the brain stem, the myelobulbar junction and the four upper segments of the spinal cord, which is manifested by autonomic disorders, dysfunction of the circulatory and respiratory systems [8]. Back in the 60s of the last century N.V. Vereshchagin noted that damage to the distal parts of the VA leads to insufficient blood supply to the cerebellum, diencephalic region and brain stem, and its occipital lobes [1]. Many authors assumed that even in the development of Wellenberg-Zakharchenko syndrome, a significant role could be played not only by the pathology of the intracranial part of the VA, but also by the pathology of its extracranial part against the background of degenerative-dystrophic changes in the cervical spine [4]. Symptoms such as transient alternating paralysis, visual and vestibular disorders have been associated with dynamic circulatory disorders in the PA system [11, 25].
In the first decades of the 21st century, the problem of SHOP instability has not lost its relevance. The issue of vascular disorders in the VBS that occurs in patients of working age has again become acute. Not taking into account whiplash and birth injuries to the neck, the prevalence of instability of the spinal cord in the population at the present stage is quite high. Its occurrence in people of working age is associated with the characteristics of modern work activity. Physical inactivity, stereotypical postures when working at a computer or driving a car, poor organization of the workplace, lack of technical breaks - all this leads to abnormal loads on the cervical-collar area. Chronic mechanical impact on the spine with hyperextension puts the greatest load on the CI-CII joint, and with hyperflexion - on the CIV-CV segment. With static loads accompanied by stretching or hyperextension of the spinal cord, hemorrhages into the adventitia of the VA are possible with the development of persistent vasospasm (AS) [1, 11] and the clinical picture of bulbomyeloischemia. Loads with hyperflexion usually lead to damage to the disc ligament apparatus, and subsequently signs of intervertebral instability, compression of the radiculomedullary artery and regional myeloradiculoischemia appear [10]. As a rule, the first clinical harbingers of already developing instability of the spine are headaches. According to A.Yu. Ratner, these headaches are more often localized on one side, they can change their side from attack to attack, their intensity depends on the movement of the head, its prolonged tense-forced position, and intensifies when walking [9]. An example of a clear extravasal influence is MRI and angiography-confirmed attacks of sudden falls due to switching off muscle tone when turning the head sharply - the so-called transient spinal attacks (dropp attaks). In these cases, clinical and instrumental comparison clearly indicates short-term vertebrogenic compression of the vertebral artery with the development of ischemia. In our observations, in some patients with instability of the spine, MRI revealed multiple small foci of vascular origin in the medulla. These patients complained of episodes of loss of consciousness during sudden turns or throwing back the head. Thus, the position or even the degree of duration of stereotypical poses is of key importance. In particular, research by T.A. Khorevoy [21] confirm the important role of head position during sleep in patients with vertebrobasilar insufficiency (VBI), emphasizing the difficulty of venous circulation according to ultrasound data in fast sleeping patients as one of the leading factors. Such headaches often occur at night and persist or worsen in the morning. Often, these cephalgic attacks intensify or provoke autonomic dysfunction of the body in the form of lability of blood pressure (BP), palpitations, hyperhidrosis, chills or, on the contrary, sensations of heat, nausea and vomiting. Before the onset of headache attacks, one of the clinical manifestations of instability of the cervical spine may be “fogginess” of consciousness that occurs when turning the head. Often, patients themselves noted the appearance of asthenia, adynamia, and disturbances in the rhythm of sleep and wakefulness. All this, both domestic and foreign authors, was regarded as dysfunction of the reticular formation of the brainstem, caused by circulatory deficiency in the VLS [4, 11, 15]. If in the 60-70s. In the 20th century, it was possible to assume the vascular genesis of the above-mentioned disorders in patients with cervical spine pathology, based on clinical and radiological research methods, but in the era of ultrasound technology it became possible to clarify their pathogenesis using duplex scanning of the brachiocephalic vessels (BCV) and registration of blood flow velocity indicators in Doppler mode [6]. Further improvement of ultrasound diagnostic methods made it possible to evaluate not only arterial inflow, but also venous outflow, the disruption of which is no less important for the formation of circulatory failure in the VVS [24].
Material and methods
We examined 256 patients who had an outpatient appointment with a neurologist. Of these, 197 (76.9%) were women and 59 (23.1%) were men. The average age of the subjects was 36.8±11.6 years.
The leading complaint was persistent headaches, accompanied by symptoms of vertebrobasilar insufficiency (VBI) (dizziness, tinnitus, hearing loss, incoordination, staggering, etc.) and signs of autonomic dysfunction (nausea, retching, palpitations, instability of arterial blood). pressure, increased sweating, etc.). Often, when questioning patients, attention was drawn to information about morning swelling of the face or eyelids, not associated with taking fluids at night, morning weakness and reduced ability to work. According to the patients, performance increased in the afternoon and was accompanied by a decrease or complete disappearance of the pastiness of the face and eyelids.
The clinical examination included an assessment of the neurological status of the patients (stating the symptoms of the VBN syndrome complex: the presence and nature of nystagmus, accuracy of coordination tests, maintaining balance in the Romberg test, we also assessed the patient’s gait) and the condition of the fundus of the eye (features of the course of arteries and veins, changes in the optic nerve head ).
The main method for diagnosing cervical spine instability was survey spondylography, supplemented by functional tests. In our work, the study was carried out using a digital X-ray machine Axiom Iconos R 200 (Germany). The method did not require special training or additional recommendations. The radiation exposure when performing an X-ray of the spine with functional tests corresponded to 0.384 mSv and did not exceed the permissible radiation exposure for medical research per year (1 mSv) in addition to natural radiation (2 mSv/year).
The method of functional x-ray examination (FRI) is given particular importance in identifying unstable vertebral displacement [13, 17-19, 28]. The technique consists of taking lateral radiographs in the position of maximum flexion and extension. This diagnostic method makes it possible to identify instability of the spine in the form of anterior, posterior or combined listhesis, determine the amplitude of vertebral displacement and establish the position (flexion and/or extension) in which additional degrees of freedom of movement of the vertebrae appear. To assess unstable vertebral displacement I.L. Tager and I.S. Mazo (1979) introduced an additional criterion - the instability index (P), which is the sum or difference in the extent of vertebral displacement, measured in millimeters and obtained when performing FRI in two mutually opposite directions [16]:
Р=L1+L2,
where L1 is the greatest extent of vertebral displacement, L2 is the smallest extent of vertebral displacement.
According to a number of authors, a displacement of the vertebrae by 2 mm in the anteroposterior direction when performing FRI cannot be considered as a reliable sign of instability of the intervertebral segments [13], which one may disagree with when studying the issue of instability of the spinal spine, due to the fact that the above The studies are based on the summation of clinical material on instability of the lumbar spine. Nevertheless, some researchers believe that in relation to the cervical spine, “staircase displacements” of up to 2-3 mm should not be regarded as pathological. In emergency orthopedics, for example, instability of the lower part of the spine is understood as a displacement of the vertebrae relative to each other by more than 3-5 mm with the appearance of anterior or posterior spinal syndrome, and instability of the upper part of the spine (C1-C2) is a displacement of ≥7 mm, which indicates a rupture of the transverse ligaments [2].
In the literature available to us, we were unable to find specific reports on instability of the spinal cord of a non-traumatic nature as a cause of vascular disorders in the VBS and the characteristics of blood flow in the VA. At the same time, a lot of data have been published on dysfunction of blood flow in the VBL against the background of degenerative-dystrophic changes in the cervical spine.
To assess the effect of displacement of the cervical vertebrae on blood flow in the VBS at the extracranial level, we recorded changes in the systolic linear velocity of blood flow (LSVsyst.) in the V2 and V3 segments of the VA using the Angiodin device from BIOSS (Russia) at rest and after performing functional tests with rotation heads. The study of the structure of the BCS was performed using duplex scanning (DS) on an Antaros “Siemens” apparatus, Germany. The study was carried out in the supine position with the chin raised. During the diagnosis, hemodynamically significant obstacles at the extracranial level were identified (hemodynamically significant atherosclerosis of the blood vessels of the central nervous system and/or macroangiopathy), the nature of the course of the VA in the bone canal formed by the openings of the transverse processes of the cervical vertebrae.
Using the DS BCS, blood flow was assessed at the level of the V2 segment of the VA and the probable vertebrogenic effect on the VA was determined by the difference in velocity parameters between the transverse processes of the vertebrae.
In addition to identifying the characteristics of arterial blood flow in the system of carotid and vertebral arteries, we recorded venous blood flow in the vertebral venous plexuses to diagnose paravertebral venous disticulation (VD). The basin of the vertebral veins (plexuses) was examined with the patient lying on his back in the projection of the V2 and V3 segments of the VA. Considering the fact that the outflow of venous blood from the cranial cavity in a horizontal position is carried out through the jugular veins, increased venous blood flow in the vertebral plexuses indicates its difficulty. In our work, “zero” blood flow values were recorded in some patients, which, according to some authors, is quite common in the population and is one of the normal variants [5]. According to the literature, in DS, paravertebral venous discirculation manifests itself, as a rule, by expansion of the vertebral plexuses and acceleration of the linear velocity of blood flow to an average of 50.02±30.88 [5] and even up to 75-80 cm/s. [8] However, at the present stage, researchers have not been able to clearly establish standard blood flow indicators for the venous plexuses.
If indicated, in a number of cases patients underwent magnetic resonance imaging (MRI) of the brain and spine, including in vascular mode.
Patients underwent a detailed comprehensive examination of the cardiovascular (CVS), endocrine system, esophageal system, etc. If causes other than instability of the spinal cord were identified that could affect blood flow in the VBL, patients were excluded from the study.
results
When patients sought medical help in their neurological status, clinical signs of VBI were identified. The majority of those examined were diagnosed with horizontal small-scale unilateral or bilateral nystagmus, unsatisfactory performance of the finger-nose test in the form of missing on one or both sides, instability in the form of deviation of the body to the right and/or left not only in the complicated, but also in the simple Romberg test.
As a rule, nystagmus was stable and was noted in most patients both during the period of exacerbation and after relief of the pain syndrome. The degree of severity of other clinical manifestations (uncertainty when performing coordination tests, instability of body position in the Romberg test) varied depending on the timing of the examination: at the time of a painful attack, its subsidence, against the background of a subjective satisfactory state.
In a number of cases, when examining patients, attention was drawn to the puffiness of the face and the pastiness of the eyelids.
During an ophthalmological examination, all patients had signs of retinal angiopathy, expressed in vasospasm of arterioles and their tortuosity, as well as dilation, tortuosity, tension or atony of venules, which correlated with ultrasound data on paravertebral VD. Signs of congestive optic disc were not noted in any observation.
During the X-ray examination, displacement of the vertebrae only during flexion was detected in 75 patients (29.3%), only during extension - in 95 (37.1%). Signs of instability of the intervertebral segments both in the flexion and extension positions were diagnosed in 86 cases (33.6%).
In a comparative analysis of vertebral displacement, it was found that in the flexion position, unstable retrolisthesis and antelesthesis occurred in an equal number of cases, which corresponded to 79 (30.9%) and 81 (31.6%) observations. In the extension position, unstable retrolisthesis was significantly more common. They were identified in 177 people (69.1%), while unstable antelestheses occurred in only 5 patients (1.9%).
Both in the position of maximum flexion and in the position of maximum extension, the C2-C6 vertebrae were involved in the process of formation of pathological mobility of the intervertebral segments, while the C1 and C7 vertebrae remained stable.
In the flexion position, displacement of the C4 vertebra was detected in 109 patients, which accounted for 42.6% of clinical observations. The amplitude of its displacement reached an average of 2.5±0.6 mm (1-4 mm). Pathological mobility of the C3 and C5 vertebrae occurred in 89 (34.8%) and 55 (21.5%) cases, respectively, and the extent of pathological sliding of the vertebrae during functional loads was 2.5±0.7 mm (1-5 mm) and 2.5±0.6 mm (1-3 mm). Less often, according to the FRI data, displacement of the C2 and C6 vertebrae was noted. Thus, pathological mobility of the C2 vertebra occurred in 41 (16%) cases and reached 2.3±0.6 mm (1-4 mm), and displacement of the C6 vertebra - in 16 (6.25%) and corresponded to 2. 75±0.45 mm (2-3 mm).
In the extension position, displacement of the C3 and C4 vertebrae was most often recorded. The presence of an additional degree of freedom of the C3 vertebra during extension of the spinal spine was established in 120 patients (46.9%), while the displacement reached 2.4±0.6 mm (1-4 mm). Instability of the C4 vertebra was diagnosed in 130 (50.8%), with a displacement of 2.4±0.7 mm (1-4 mm). Instability of the C2 vertebra was noted somewhat less frequently - in 54 patients (21.1%) with a deviation amplitude of 2.2±0.6 mm (1-5 mm), and instability of the C5 vertebra - in 81 (31.6%) with an amplitude 2.5±0.6 mm (1-4 mm). Displacement of the C6 vertebra in the position of maximum extension was found in only 11 people (4.3%) and remained 2.25±0.9 mm (1-3 mm) (Table 1)
.
As a rule, displacements of not one, but several vertebrae were more common. Thus, in the position of maximum flexion, instability of the 1st cervical vertebra was detected only in 49 patients (19.1%). Most often, excessive mobility of 2 or 3 vertebrae was observed. Thus, simultaneous displacement of 2 vertebrae was diagnosed in 54 people (21.1%), 3 - 39 (15.2%). Displacement of 4 vertebrae was quite rare - in 12 patients (4.7%). And only one patient (0.4%) had displacement of 5 vertebrae.
In the maximum extension position, displacement of 1, 2 and even 3 vertebrae was found in equal proportions, which corresponded to 55 (21.5%), 59 (23%) and 54 (21.1%) clinical observations. As with flexion, instability of the 4th and 5th cervical vertebrae during extension is diagnosed in a rare percentage of cases. Thus, simultaneous pathological displacement of 4 vertebrae was recorded according to FRI data in 14 patients (5.5%), and 5 vertebrae - in only one (0.4%) (Table 2)
.
When studying blood flow at the extracranial level in the carotid and vertebral-basilar systems, it was found that speed indicators in the carotid vascular system corresponded to the norm, while LSCsist. in both PAs on average was below standard indicators (Table 3)
.
Features of blood flow in the VBS in the pathology of the cervical spine affect not only the arterial, but also the venous component.
Thus, in terms of arterial blood flow in the VBS, a decrease in LSCsist indicators was revealed in the group of patients as a whole. in both PAs. In 89 patients (34.7%), a vertebrogenic effect on the extracranial part of the VA was noted when turning the head, and in 66 patients (25.8%) asymmetry of the LSCsist was registered. regardless of the diameter of the PA. However, not all patients had non-straightness of the V2 segment of the VA. In most of them, blood flow asymmetry was established with almost equal diameters of the right and left VAs and with their straight course in the canal of the transverse processes of the cervical vertebrae. In 5 (1.95%) observations an increase in LSCsist was recorded. over 50 cm/s according to the AS PA type, and in 17 (6.6%) - a decrease in LSCsist. below 30 cm/s.
Features of venous blood flow in 101 patients (39.45%) consisted of registration of paravertebral VD. The results obtained, as noted above, correlated with the data of an ophthalmological examination, which revealed changes in the fundus veins against the background of VD.
Despite the direction and degree of displacement of the cervical vertebrae, intact blood flow in the VA was recorded in 51 (19.9%) patients. In these subjects, no circulatory pathology was detected either in the arterial or venous segment of the VBS, even with a displacement of the vertebrae of up to 3 mm. In a number of observations, on the contrary, in patients with a displacement of 1-2 mm, there was a simultaneous decrease in the speed of blood flow in the VA, their asymmetry, a vertebrogenic effect on the VA when turning the head, as well as paravertebral VD.
Conclusion
Instability of the spinal cord can serve as an extravasal cause of impaired blood flow in the VBL. It can be assumed that there are stages of development of the morphological process in the walls of the VA, manifested by pathophysiological changes in blood flow in the V2 and V3 segments of the VA and the progression of clinical symptoms, which may be due to an increase in the degree of displacement of the cervical vertebrae. At the initial stages of the formation of additional degrees of freedom of the cervical segments, AS of the extracranial part of the VA occurs due to irritation by the bone structures of the perivascular nerve fibers and is temporary. With the formation of a more significant displacement of the vertebrae during flexion and extension, rotation of the spine, in each individual clinical case, mechanical damage to the walls of the vessels themselves occurs and changes in blood flow become more stable, associated with more gross morphological changes in the vascular tissue of the VA (microhemorrhages were identified using the example of sectional material into the VA wall [3], decreased elasticity of the VA wall, periarterial scar process [12, 23]). Achieving a critical displacement can contribute to a temporary cessation of blood flow and the appearance of a corresponding clinical picture, expressed as a stable neurological deficit, even death.
Despite the significant impact of instability of the spinal cord on the blood flow of the spinal vein and the occurrence of neurological symptoms, not all patients can be diagnosed with dysfunction of the blood supply in the spinal vein. For the occurrence of stable changes in blood flow in the VA and the formation of the corresponding neurological deficit, the diameter of the opening of the transverse process of the cervical vertebra and the diameter of the corresponding VA passing through this opening are of greater importance. Both of these sizes are important both for the irritation of the paravasal nerve plexuses with the formation of AS VA, and for the mechanical impact on the VA itself during displacement of the vertebrae, which explains the instability of neurological symptoms at the initial stages of the formation of cervical spine instability and their acquisition of a stable character with progressive maximum permissible displacement.
The occurrence of instability of the spine can be associated with various reasons (trauma, forced posture of the head and neck, birth trauma), but, as a rule, they are all damaging to the ligamentous apparatus of the spine, which performs a support-limiting function. They can be a “whiplash” injury received in road accidents, an injury during various sports (skiing, speed skating, artistic or rhythmic gymnastics, weightlifting, etc.).
In the 80s of the last century, much attention was paid to birth injuries, during which the cervical spine was damaged [14]. It was noted that a birth injury to the brain immediately manifests itself as severe neurological symptoms, while when reserve blood supply pathways are turned on, cervical injury, even with a temporary cessation of blood flow in the VA, can manifest itself with a detailed clinical picture only when compensatory capabilities are disrupted. Often, behind the minimal local neurological signs of a birth injury suffered by the cervical spine, there may be, at first glance, a seemingly minor injury to the cervical vertebrae. One of the alarming manifestations of birth trauma to the cervical spine, especially in children of middle and high school age, is headaches that occur during mental stress during school and extracurricular activities, static loads on the cervical spine when the child is forced to sit at a desk, and motor stress during physical education lessons. On this occasion, E.I. Aukhadeyev developed strict criteria for selecting such children for physical education with strict medical supervision in order to avoid any complications (quote from A.Yu. Ratner) [14]. Underestimation of the severity of damage does not allow specific treatment to be provided to all pediatric patients, and lack of control over this pathology leads to the appearance of “spinal instability syndrome,” which may be sufficient to cause the occurrence of quite diverse and the most severe neurological syndromes in older patients [14].
It is known that compensatory mechanisms of cerebral blood flow can persist for quite a long time and do not manifest themselves in childhood, and their breakdown is possible in adulthood, when not only physical, but also psycho-emotional stress increases. And then patients of the older age group seek medical help due to increased frequency or new, but persistently progressive headaches, accompanied by signs of VBI. Currently, the cause of this pain syndrome may be the load on the cervical-collar area imposed on patients due to the nature of their work activity. Computerization of workplaces, abnormal static loads with a long stay in a forced position with neck tension, lack of dynamic unloading - all this can lead to aggravation of instability of the spine or lead to its formation in initially healthy individuals. Microtraumatization by chronic loads of the initially healthy ligamentous apparatus of the spinal cord or aggravation of an existing problem creates the risk of vertebral dislocation in response to a fall, injury, sharp turn of the head or torso. In some cases, even a prolonged position of forced flexion or extension in the workplace or at home, an uncomfortable posture of the head and neck during sleep can lead to dislocation of the vertebrae with the appearance of neurological symptoms from persistent headaches to intermittent cerebrovascular accidents caused not only by arterial dysfunction, but also venous blood flow [24].
Therefore, the relevance of this issue, which has somewhat receded into the background over the past 30 years, has again become obvious. It is possible that the occurrence of instability of the cervical spine observed in patients of working age is associated with modern working and living conditions, although it is possible that such conditions only expose a chronic problem originating in childhood: it is important to take into account the birth history (post-term, rapid labor, stimulation of labor, obstetric aid, manual influences (traction)).
conclusions
1. Displacement of a vertebra in the spine by more than 3 mm is not always the cause of changes in blood flow in the VBS; at the same time, displacement of the cervical vertebrae of less than 3 mm is often accompanied by peculiarities of blood flow in the VBS and neurological symptoms.
2. At the beginning of the formation of instability of the spinal cord, complaints and neurological symptoms indicating VBI are transient; When a certain degree of vertebral displacement is reached, neurological symptoms become permanent.
3. In the majority of clinical observations, the formation of instability of the spinal cord leads to disruption of blood flow in the VBL; in a number of observations, in patients with instability in the SC, it is not possible to detect any deviations in blood flow in the VBL.
4. Instability with displacement of the cervical vertebrae up to 2 mm, as a rule, is not accompanied by hemodynamically significant disorders, but requires dynamic monitoring, as it tends to increase displacement and the occurrence of severe vascular disorders in the VVS.